Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 7235-40-7
Drug Levels and Effects
Summary of Use during Lactation
Beta-carotene is a plant pigment that is converted into vitamin A in the body. Maternal vitamin A requirements are increased during lactation, but there are no specific guidelines for increased beta-carotene intake or indications for high-dose supplementation in nursing mothers. Typical beta-carotene intake in a Western diet is 6 to 8 mg daily. Beta-carotene is a normal component of human colostrum and mature milk, where it contributes to antioxidant defenses in the neonate.[1] A systematic review found that in infants younger than 6 months, those fed primarily human milk have greater blood carotenoid concentrations than those fed formula.[2] Some evidence suggests that there is a correlation between beta-carotene and infant motor development in exclusively breastfed infants, but not in overall psychomotor performance.[3] Beta-carotene supplementation during pregnancy and for 6 months postpartum in nursing mothers with poor diets in a resource-poor setting reduced the number of days of illness in the mothers, but does not reduce infant morbidity or mortality according to another study.[4,5] The bioavailability of beta-carotene is dependent on the fat content of the meal and the form in which it is administered, with synthetic pharmaceutical forms having the best bioavailability. High-dose beta-carotene supplements lead to a slow increase in breastmilk beta-carotene concentrations, with an accumulation half-life of about 9 days. Levels drop towards baseline slowly over several weeks after discontinuation. In general, beta-carotene is well tolerated, although excessive maternal intake of beta-carotene can lead to a harmless, reversible discoloration of the breastfed infant's skin.[6] In HIV-infected women, high-dose beta-carotene plus vitamin A supplementation increases the rate of HIV viral shedding into breastmilk and increases HIV infection in breastfed infants, although the mortality rate over the first 2 years of life is not increased.[7,8] The viral shedding may be a result of an increase in subclinical mastitis caused by beta-carotene.[9] Beta-carotene concentration in breastmilk is not affected by refrigeration, freezing, or low-temperature microwaving. The concentration does decrease when milk passes through a tube feeding system, regardless of light exposure.[10]
Dietary supplements do not require extensive pre-marketing approval from the U.S. Food and Drug Administration. Manufacturers are responsible to ensure the safety, but do not need to prove the safety and effectiveness of dietary supplements before they are marketed. Dietary supplements may contain multiple ingredients, and differences are often found between labeled and actual ingredients or their amounts. A manufacturer may contract with an independent organization to verify the quality of a product or its ingredients, but that does not certify the safety or effectiveness of a product. Because of the above issues, clinical testing results on one product may not be applicable to other products. More detailed information about dietary supplements is available elsewhere on the LactMed Web site.
Drug Levels
Maternal Levels. A systematic review of 47 articles found the mean concentration of beta-carotene in mature milk worldwide to be 24.6 mcg/L, which would provide an average dose of 19.2 mg daily of beta-carotene to a fully breastfed infant.[2] Some of the studies in this review are discussed in more detail below. [11-15]
Healthy nursing mothers in the United States were given either 60 mg (n = 6) or 210 mg (n = 6) of beta-carotene as capsules (Hoffmann-La Roche, Inc., Nutley, NJ) as a single dose. Both doses increased breastmilk beta-carotene levels to a similar extent, with peak concentrations of around 1.1 mcg/L of lipid occurring 2 to 3 days after the dose. Mothers with higher baseline beta-carotene levels had higher peak concentrations.[12]
Healthy nursing mothers in the United States were given either 7 doses of a placebo (n = 4) or of an algae-derived beta-carotene supplement containing 64 mg of all-trans beta-carotene and 69 mg 9-cis beta-carotene (Henkel Corp., LaGrange, Il). Foremilk samples of breastmilk were obtained daily for 8 days and again at 1 month after the first dose. All-trans beta-carotene levels in milk increased to about 2.1 mg/L of whole milk after 5 days of supplementation and further increased only slightly by day 8. Levels were still elevated above baseline at 1 month. Milk levels of 9-cis beta-carotene increased steadily from baseline to day 8, with a much lower peak value of about 40 ng/L. The lower value was possibly the result of isomerization of 9-cis beta-carotene to all-trans beta-carotene.[13]
Five healthy exclusively breastfeeding mothers over 1 month postpartum (average 279 days postpartum) in the United States were given 30 mg of beta-carotene as capsules (Hoffmann-La Roche, Inc. Nutley, NJ) daily for 28 days with high-fat yogurt. Milk beta-carotene levels increased an average of 6.4 fold over the 28-day period, with an average maximum concentration of about 200 mcg/L. The accumulation half-life of beta-carotene in milk was 9 days, which was almost twice as long as the accumulation half-life in serum. At one month after the end of supplementation, milk levels remained about double of baseline levels.[11]
In a study in rural Bangladesh, 139 mothers received oral beta-carotene 7.8 mg or placebo once daily for 9 months beginning between 1 and 3 weeks postpartum. Baseline maternal vitamin A status prior to administration was not measured. Average milk retinol levels were similar between the two groups at 3 and 6 months postpartum, but were higher in the beta-carotene group at 9 months (286 mcg/L vs 226 mcg/L). The percentage of women with milk levels <300 mcg/L was also lower (63% vs 80%) at 9 months in the beta-carotene group. The results were the same when the authors controlled for milk fat content.[16]
Twenty-one postpartum women in the United States received either water-dispersible beadlets of beta-carotene in capsules (n = 11), which were assayed to contain 31 to 35 mg of beta-carotene and 1.2 mg of alpha-carotene, or an identical placebo (n = 10) daily for 4 weeks starting on 4 days postpartum. During the 4 weeks of the study, there was no significant change in average breastmilk beta-carotene concentrations, whereas those in the placebo group had a decrease in average beta-carotene milk concentrations which as not statistically significant. Differences between this study and previous studies was suggested to be caused by differences in subjects' milkfat levels which were lower in this study.[14]
A study compared 4 groups of women in West Java, Indonesia who received supplementation during pregnancy until delivery. All groups received 30 mg of iron and 0.4 mg of folic acid daily. Experimental groups received either beta-carotene 4.5 mg daily as a water-soluble granulate, zinc 30 mg daily, beta-carotene 4.5 mg plus zinc 30 mg daily, or only the iron and folic acid as a control group. Milk samples were collected during the first and sixth months postpartum. The milk beta-carotene level was significantly different from the control group only in the 6-month sample of the zinc plus beta-carotene group. The vitamin A status of the mothers and their infants was also better in the group that received beta-carotene and zinc.[15]
A study of 866 HIV-infected women in Tanzania were enrolled in a study to receive 1 of 4 supplements during pregnancy and lactation. Groups received either multivitamins, multivitamins plus vitamin A and beta-carotene, vitamin A and beta-carotene alone, or placebo daily. The beta-carotene dose was 30 mg. At 24 months of age, the multivitamin-supplemented group's infants had significantly better growth parameters than the other groups.[17]
A study of HIV-infected women in Tanzania were enrolled in a study to receive 1 of 4 supplements during pregnancy and lactation. Groups receive either multivitamins (thiamine, riboflavin, vitamin B6, niacin, vitamin B12, vitamin C, vitamin E, and folic acid), multivitamins plus vitamin A and beta-carotene, vitamin A and beta-carotene alone, or placebo daily. The beta-carotene dose was 30 mg. Breastmilk samples were collected at delivery and at 3-month intervals thereafter. Average breastmilk beta-carotene concentrations in the beta-carotene supplemented groups were consistently about 10-fold higher than in the groups that received no beta-carotene at any time up to 1 year of age.[18]
Twelve women were given carrot paste and 14 were given tomato paste with a high-fat meal once daily for 3 days. The carrot supplement contained 15 mg of all-trans beta-carotene and the tomato supplement contained 15 mg of all-trans lycopene. Breastmilk beta-carotene levels nearly doubled after 3 days of supplementation, whereas lycopene levels increased by about 15% one day after the 3 days of supplementation.[19]
Infant Levels. A systematic review of studies on beta-carotene plasma levels of breastfed infants found that in 54 infants from 4 to 12 weeks of age in the US, the average beta-carotene plasma level was about 70 mcg/L. In studies from outside the US, 62 infants aged 1 to 26 weeks had an average beta-carotene plasma concentration of 223 mcg/L.[2]
Effects in Breastfed Infants
A nursing mother was eating 2 to 3 pounds of carrots a week as raw and cooked carrots. The mother's skin was yellow in color, but her sclera were clear. At 2 months of age, her breastfed infant was diagnosed as having jaundice because of a yellow coloration of the skin. Breastfeeding was discontinued and the infant's skin returned to a normal color. The mother continued her diet and examination of the maternal serum found elevated levels of beta-carotene which was probably the cause of her infant's skin discoloration.[6]
HIV-infected women in Tanzania received 1 of 4 supplements during pregnancy and lactation in a series of studies. Groups received either multivitamins (thiamine, riboflavin, vitamin B6, niacin, vitamin B12, vitamin C, vitamin E, and folic acid), multivitamins plus vitamin A and beta-carotene, vitamin A and beta-carotene alone, or placebo daily. The beta-carotene dose was 30 mg. At 24 months of age, the multivitamin-supplemented group's infants had significantly better growth parameters than the other groups.[17] One study found that the infants of mothers supplemented with vitamin A and beta-carotene had a higher rate of HIV transmission than those supplemented with multivitamins alone or placebo.[7] After 6 months postpartum, women who received vitamin A plus beta-carotene had greater shedding of the HIV virus into breastmilk than women who had not; multivitamins without vitamin A and beta-carotene did not increase viral shedding.[7] Beta-carotene appeared to have a shedding effect that was independent of vitamin A.[8] One possible explanation comes from another similar study in which those who received vitamin A plus beta-carotene alone had a 45% increased risk of severe subclinical mastitis and those who received multivitamins plus vitamin A and beta-carotene had a 29% increased risk of severe subclinical mastitis.[9]
Breastmilk samples were collected at the first, third and sixth months postpartum from 39 mother-infant pairs of exclusively breastfed infants. Psychomotor testing found a correlation between beta-carotene intake in breastmilk during the first 3 months of life and infant motor development, but not overall psychomotor development, at 6 months of life. Some long-chain polyunsaturated fatty acids, DHA, alpha-linolenic acid and total n-3 PUFAs, also correlated with motor development.[3]
Effects on Lactation and Breastmilk
Relevant published information was not found as of the revision date.
References
- 1.
- Ostrea EM Jr, Balun JE, Winkler R, et al. Influence of breast-feeding on the restoration of the low serum concentration of vitamin E and beta-carotene in the newborn infant. Am J Obstet Gynecol. 1986;154:1014–7. [PubMed: 3706423]
- 2.
- Zaidi Y, Stroh R, Moran NE. Systematic review of carotenoid concentrations in human milk and infant blood. Nutr Rev. 2022;80:2029–50. [PubMed: 35389473]
- 3.
- Zielinska MA, Hamulka J, Grabowicz-Chądrzyńska I, et al. Association between breastmilk LC PUFA, carotenoids and psychomotor development of exclusively breastfed infants. Int J Environ Res Public Health. 2019;16:1144. [PMC free article: PMC6479893] [PubMed: 30935000]
- 4.
- Christian P, West KP Jr, Khatry SK, et al. Vitamin A or beta-carotene supplementation reduces symptoms of illness in pregnant and lactating Nepali women. J Nutr. 2000;130:2675–82. [PubMed: 11053506]
- 5.
- Gogia S, Sachdev HS. Maternal postpartum vitamin A supplementation for the prevention of mortality and morbidity in infancy: A systematic review of randomized controlled trials. Int J Epidemiol. 2010;39:1217–26. [PubMed: 20522482]
- 6.
- Thomson ML. Carotinaemia in a suckling. Arch Dis Child. 1943;18:112. (Letter.) [PMC free article: PMC1987848] [PubMed: 21032250]
- 7.
- Fawzi WW, Msamanga GI, Hunter D, et al. Randomized trial of vitamin supplements in relation to transmission of HIV-1 through breastfeeding and early child mortality. AIDS. 2002;16:1935–44. [PubMed: 12351954]
- 8.
- Villamor E, Koulinska IN, Aboud S, et al. Effect of vitamin supplements on HIV shedding in breast milk. Am J Clin Nutr. 2010;92:881–6. [PMC free article: PMC2937587] [PubMed: 20739426]
- 9.
- Arsenault JE, Aboud S, Manji KP, et al. Vitamin supplementation increases risk of subclinical mastitis in HIV-infected women. J Nutr. 2010;140:1788–92. [PMC free article: PMC2937574] [PubMed: 20739447]
- 10.
- Tacken KJ, Vogelsang A, van Lingen RA, et al. Loss of triglycerides and carotenoids in human milk after processing. Arch Dis Child Fetal Neonatal Ed. 2009;94:F447–50. [PubMed: 19416803]
- 11.
- Canfield LM, Giuliano AR, Neilson EM, et al. Kinetics of the response of milk and serum beta-carotene to daily beta-carotene supplementation in healthy, lactating women. Am J Clin Nutr. 1998;67:276–83. [PubMed: 9459376]
- 12.
- Canfield LM, Giuliano AR, Neilson EM, et al. beta-Carotene in breast milk and serum is increased after a single beta-carotene dose. Am J Clin Nutr. 1997;66:52–61. [PubMed: 9209169]
- 13.
- Johnson EJ, Qin J, Krinsky NI, et al. Beta-carotene isomers in human serum, breast milk and buccal mucosa cells after continuous oral doses of all-trans and 9-cis beta-carotene. J Nutr. 1997;127:1993–9. [PubMed: 9311956]
- 14.
- Gossage CP, Deyhim M, Yamini S, et al. Carotenoid composition of human milk during the first month postpartum and the response to beta-carotene supplementation. Am J Clin Nutr. 2002;76:193–7. [PubMed: 12081834]
- 15.
- Dijkhuizen MA, Wieringa FT, West CE, et al. Zinc plus beta-carotene supplementation of pregnant women is superior to beta-carotene supplementation alone in improving vitamin A status in both mothers and infants. Am J Clin Nutr. 2004;80:1299–307. [PubMed: 15531679]
- 16.
- Rice AL, Stoltzfus RJ, de Francisco A, et al. Maternal vitamin A or beta-carotene supplementation in lactating Bangladeshi women benefits mothers and infants but does not prevent subclinical deficiency. J Nutr. 1999;129:356–65. [PubMed: 10024613]
- 17.
- Villamor E, Saathoff E, Bosch RJ, et al. Vitamin supplementation of HIV-infected women improves postnatal child growth. Am J Clin Nutr. 2005;81:880–8. [PubMed: 15817867]
- 18.
- Webb AL, Aboud S, Furtado J, et al. Effect of vitamin supplementation on breast milk concentrations of retinol, carotenoids and tocopherols in HIV-infected Tanzanian women. Eur J Clin Nutr. 2009;63:332–9. [PMC free article: PMC3095494] [PubMed: 17940544]
- 19.
- Haftel L, Berkovich Z, Reifen R. Elevated milk beta-carotene and lycopene after carrot and tomato paste supplementation. Nutrition. 2015;31:443–5. [PubMed: 25701332]
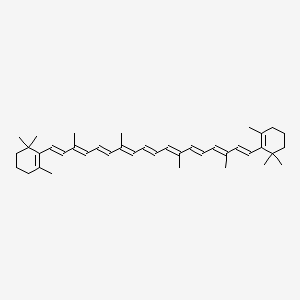
Substance Identification
Substance Name
Beta-Carotene
CAS Registry Number
7235-40-7
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- Review Marine Oils.[Drugs and Lactation Database (...]Review Marine Oils.. Drugs and Lactation Database (LactMed®). 2006
- Review Melatonin.[Drugs and Lactation Database (...]Review Melatonin.. Drugs and Lactation Database (LactMed®). 2006
- Review Glucosamine.[Drugs and Lactation Database (...]Review Glucosamine.. Drugs and Lactation Database (LactMed®). 2006
- Review Coenzyme Q10.[Drugs and Lactation Database (...]Review Coenzyme Q10.. Drugs and Lactation Database (LactMed®). 2006
- Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas.[Cochrane Database Syst Rev. 2022]Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas.Crider K, Williams J, Qi YP, Gutman J, Yeung L, Mai C, Finkelstain J, Mehta S, Pons-Duran C, Menéndez C, et al. Cochrane Database Syst Rev. 2022 Feb 1; 2(2022). Epub 2022 Feb 1.
- Beta-Carotene - Drugs and Lactation Database (LactMed®)Beta-Carotene - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
