Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 50-18-0
Drug Levels and Effects
Summary of Use during Lactation
Cyclophosphamide appears in milk in potentially toxic amounts; additionally, highly toxic active metabolites could add to the risk to the infant. Neutropenia has been reported in 2 infants whose mothers breastfed them while receiving cyclophosphamide. Most sources consider breastfeeding to be contraindicated during maternal cytotoxic antineoplastic drug therapy, especially alkylating agents such as cyclophosphamide.[1] Although some have suggested withholding breastfeeding for 1 to 3 days after a dose,[2] it appears to take more than 21 days for the drug and its metabolites to be completely eliminated from breastmilk. Some authors’ data suggest that it might take 6 weeks for milk levels to drop to a safe level after a dose of cyclophosphamide 750 mg/sq. m.[3]
Chemotherapy may adversely affect the normal microbiome and chemical makeup of breastmilk.[4] Women who receive chemotherapy during pregnancy are more likely to have difficulty nursing their infant.
Drug Levels
Maternal Levels. Unmetabolized cyclophosphamide was qualitatively detected in milk 1, 3, 5 and 6 hours after IV injection of 500 mg of drug in one patient.[5,6] Quantitative determination was not reported.
A mother who had been exclusively breastfeeding for 6 months was diagnosed with multiple sclerosis. In preparation for stem cell transplantation, she received intravenous cyclophosphamide 2.8 grams daily for 4 consecutive days. She was also receiving anti-thymocyte immune globulin, methylprednisolone, mesna, and furosemide. She provided milk samples several times on each of the 4 days for analysis of cyclophosphamide. No metabolites, including active metabolites, were measured. Peak cyclophosphamide milk levels occurred at 4 to 5 hours each day. However, the level of exposure was lower on each successive day, presumably because of autoinduction of the drug's metabolism. Peak level ranged from 40.8 mg/L on day 1 to 13.2 mg/L on day 4; the average level ranged from 15.1 mg/L on day 1 to 3.1 mg/L on day 4; and the estimated daily infant dosage ranged from 2.3 mg/kg on day 1 to 0.5 mg/kg on day 4. The weight-adjusted percentage of the maternal dosage ranged from 4.8% on day 1 to 0.9% on day 4.[7]
A woman was diagnosed with B-cell non-Hodgkins lymphoma at 4 months postpartum. She received R-CHOP therapy every 21 days for 6 cycles. It consisted of rituximab 375 mg/sq. m, cyclophosphamide 750 mg/sq. m, doxorubicin 50 mg/sq. m, vincristine 1.4 mg/sq. m (capped at 2 mg) plus prednisone 40 mg/sq. m daily. She also received oral 300 mg of allopurinol daily during the whole therapy course. Milk samples were collected twice daily during the first 3 cycles then once daily for the remaining cycles for a total of 290 samples. Cyclophosphamide was detectable in milk shortly after administration, with the peak milk level of over 1 mg/L occurring shortly after the first dose. The toxic metabolites,4-ketocyclophosphamide, 4-hydroxycyclophosphamide, carboxycyclophosphamide, and N-dechloroethylcyclophosphamide were also detectable in milk. Cyclophosphamide dropped to low levels after a week, but the drug and some of its toxic metabolites were still detectable at 21 days after the dose.[3]
A woman with breast cancer diagnosed during pregnancy received chemotherapy beginning a few days after delivery. It consisted of doxorubicin 118 mg and cyclophosphamide 1180 mg every 2 weeks for 4 cycles, followed by paclitaxel 156 mg weekly and carboplatin 900 mg every 4 weeks. She collected 97 milk samples. A second patient was diagnosed with breast cancer 6.5 months postpartum. Her treatment consisted of doxorubicin 130 mg and cyclophosphamide 1300 mg every 2 weeks for 4 cycles, followed by paclitaxel weekly and carboplatin every 4 weeks. She collected 15 milk samples. A selection of 30 samples from the two patients were analyzed for cyclophosphamide. Peak milk levels after the first round of chemotherapy were about 15.5 mg/L in the first patient and about 18 mg/L in the second. Levels decreased to less than 200 mcg/L by about 2 days after the dose. The authors calculated the time for the milk concentration to reach a relative infant dosage (RID) level below 1% to be one day; however potentially toxic metabolites were not measured.[2] A further pharmacokinetic analysis of all breastmilk samples found that cyclophosphamide levels in milk decrease rapidly and that milk should be discarded for 1 to 2 days after each dose in a cycle to achieve a cumulative relative infant dosage of <1%. However, this estimate did not include the presence of active metabolite(s) in milk, so this time represents the minimum time to withhold breastfeeding.[8]
Infant Levels. Relevant published information was not found as of the revision date.
Effects in Breastfed Infants
In one 23-day-old infant, neutropenia, thrombocytopenia and a low hemoglobin were possibly caused by cyclophosphamide after 3 days of maternal treatment with cyclophosphamide 6 mg/kg IV daily (total dose 300 mg).[9]
In a 4-month-old, neutropenia was probably caused by cyclophosphamide in a mother 9 days after the last of 6 weekly doses of 800 mg cyclophosphamide intravenously, 2 mg vincristine intravenously and daily doses of 30 mg of prednisolone orally. Neutropenia persisted at least 12 days and was accompanied by a brief episode of diarrhea.[10]
A woman was diagnosed with B-cell lymphoma at 27 weeks of pregnancy. Labor was induced at 34 4/7 weeks and treatment was begun with a standard regimen of rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone in unspecified doses on a 21-day cycle, starting on day 2 postpartum. She pumped and discarded her milk and fed her infant donor milk for the first 10 days of each cycle and then breastfed her infant for the remaining 10 days before the next treatment cycle. The 10-day period of breastfeeding abstinence was determined by using about 3 half-lives of vincristine. After completion of 4 cycles of chemotherapy, her infant was reportedly healthy and developing without any complications.[11]
Effects on Lactation and Breastmilk
Telephone follow-up study was conducted on 74 women who received cancer chemotherapy at one center during the second or third trimester of pregnancy to determine if they were successful at breastfeeding postpartum. Only 34% of the women were able to exclusively breastfeed their infants, and 66% of the women reported experiencing breastfeeding difficulties. This was in comparison to a 91% breastfeeding success rate in 22 other mothers diagnosed during pregnancy, but not treated with chemotherapy. Other statistically significant correlations included: 1. mothers with breastfeeding difficulties had an average of 5.5 cycles of chemotherapy compared with 3.8 cycles among mothers who had no difficulties; and 2. mothers with breastfeeding difficulties received their first cycle of chemotherapy on average 3.4 weeks earlier in pregnancy. Of the 56 women who received a cyclophosphamide-containing regimen, 34 had breastfeeding difficulties.[12]
References
- 1.
- Pistilli B, Bellettini G, Giovannetti E, et al. Chemotherapy, targeted agents, antiemetics and growth-factors in human milk: How should we counsel cancer patients about breastfeeding? Cancer Treat Rev. 2013;39:207–11. [PubMed: 23199900]
- 2.
- Damoiseaux D, Calpe S, Rosing H, et al. Presence of 5 chemotherapeutic drugs in breast milk as a guide for the safe use of chemotherapy during breastfeeding: Results from a case series. Clin Pharmacol Ther. 2022;112:404–10. [PubMed: 35486426]
- 3.
- Codacci-Pisanelli G, Honeywell RJ, Asselin N, et al. Breastfeeding during R-CHOP chemotherapy: Please abstain! Eur J Cancer. 2019;119:107–11. [PubMed: 31437753]
- 4.
- Urbaniak C, McMillan A, Angelini M, et al. Effect of chemotherapy on the microbiota and metabolome of human milk, a case report. Microbiome. 2014;2:24. [PMC free article: PMC4109383] [PubMed: 25061513]
- 5.
- Duncan JH, Colvin OM, Fenselau C. Mass spectrometric study of the distribution of cyclophosphamide in humans. Toxicol Appl Pharmacol. 1973;24:317–23. [PubMed: 4741053]
- 6.
- Wiernik PH, Duncan JH. Cyclophosphamide in human milk. Lancet. 1971;1:912. [PubMed: 4102054]
- 7.
- Fierro ME, Datta P, Rewers-Felkins K, et al. Cyclophosphamide use in multiple sclerosis: Levels detected in human milk. Breastfeed Med. 2019;14:128–30. [PubMed: 30589584]
- 8.
- Damoiseaux D, Centanni D, Beijnen JH, et al. Predicting chemotherapy distribution into breast milk for breastfeeding women using a population pharmacokinetic approach. Clin Pharmacokinet. 2023;62:969–80. [PMC free article: PMC10338611] [PubMed: 37154994]
- 9.
- Durodola JI. Administration of cyclophosphamide during late pregnancy and early lactation: A case report. J Natl Med Assoc. 1979;71:165–6. [PMC free article: PMC2537339] [PubMed: 423292]
- 10.
- Amato D, Niblett JS. Neutropenia from cyclophosphamide in breast milk. Med J Aust. 1977;1:383–4. [PubMed: 859486]
- 11.
- Hersey AE, Giglio P, Kurt H, et al. Diffuse large B-cell lymphoma during third-trimester pregnancy and lactation. Obstet Gynecol. 2020;135:383–6. [PubMed: 31923071]
- 12.
- Stopenski S, Aslam A, Zhang X, et al. After chemotherapy treatment for maternal cancer during pregnancy, is breastfeeding possible? Breastfeed Med. 2017;12:91–7. [PubMed: 28170295]
Substance Identification
Substance Name
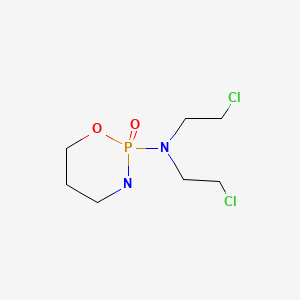
Cyclophosphamide
CAS Registry Number
50-18-0
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- Synthesis of deuterium-labeled analogs of cyclophosphamide and its metabolites.[J Med Chem. 1975]Synthesis of deuterium-labeled analogs of cyclophosphamide and its metabolites.Griggs LJ, Jarman M. J Med Chem. 1975 Nov; 18(11):1102-6.
- Mass spectrometric characterization of activated N-(2-chloroethyl)amino oxazaphosphorine derivative.[Biomed Mass Spectrom. 1977]Mass spectrometric characterization of activated N-(2-chloroethyl)amino oxazaphosphorine derivative.Przybylski M, Ringsdorf H, Lenssen U, Peter G, Voelcker G, Wagner T, Hohorst HJ. Biomed Mass Spectrom. 1977 Aug; 4(4):209-15.
- Review Carmustine.[Drugs and Lactation Database (...]Review Carmustine.. Drugs and Lactation Database (LactMed®). 2006
- Synthesis and antitumor activity of cyclophosphamide analogs. 1. Benzo annulated cyclophosphamide and related systems.[J Med Chem. 1975]Synthesis and antitumor activity of cyclophosphamide analogs. 1. Benzo annulated cyclophosphamide and related systems.Ludeman SM, Zon G. J Med Chem. 1975 Dec; 18(12):1251-3.
- Review Mitoxantrone.[Drugs and Lactation Database (...]Review Mitoxantrone.. Drugs and Lactation Database (LactMed®). 2006
- Cyclophosphamide - Drugs and Lactation Database (LactMed®)Cyclophosphamide - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
