Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 192725-17-0
Drug Levels and Effects
Summary of Use during Lactation
Lopinavir appears in breastmilk in low levels and can be found in the serum of some breastfed infants. Although lopinavir has been associated with impaired adrenal gland function when given directly to infants, the effect is dose related.[1] No adverse infant effects have been clearly caused by the small amounts of lopinavir in breastmilk. Achieving and maintaining viral suppression with antiretroviral therapy decreases breastfeeding transmission risk to less than 1%, but not zero. Individuals with HIV who are on antiretroviral therapy with a sustained undetectable viral load and who choose to breastfeed should be supported in this decision. If a viral load is not suppressed, banked pasteurized donor milk or formula is recommended.[2,3]
Ritonavir used as a booster has been studied in several studies of breastfeeding mothers. It is excreted into milk in measurable concentrations and low levels can be found in the blood of some breastfed infants. No reports of adverse reactions in breastfed infants have been reported. For more information, refer to the LactMed record on ritonavir.
Drug Levels
Maternal Levels. One study measured lopinavir in breastmilk samples from nursing mothers who had been randomized to receive the drug as part of a clinical trial to evaluate maternal to child transmission of HIV infection. The dosages, dosage regimens and time of breastmilk sample collection times were not reported. Lopinavir was not detected in any of 60 breastmilk samples.[4]
Nine mothers who were receiving lopinavir 400 mg plus ritonavir 100 mg twice daily as part of a combination antiretroviral regimen provided a total of 23 milk samples at birth, 1 month, 3 months and/or 6 months postpartum. Milk samples were collected at a median of 4.5 hours (range 3.5 to 6 hours) after the previous dose. The median breastmilk lopinavir concentration was 1834 mcg/L (range 557 to 3950 mcg/L).[5]
Fifteen women had been taking lopinavir 400 mg twice daily for 53 to 182 days as part of a drug combination that included ritonavir, zidovudine, and lamivudine. Breastmilk samples were collected at just before a dose at a median of 1 month postpartum. Whole breastmilk levels contained a median of 0.06 mg/L of lopinavir, which was a median of 0.7% of maternal blood levels.[6]
Thirty women were studied at 6, 12 or 24 weeks postpartum (10 at each time). Each mother was taking zidovudine 300 mg, lamivudine 150 mg, lopinavir 400 mg, and ritonavir 100 mg twice daily by mouth starting at delivery. On the study day, at a median of 14.9 hours after the previous evening's dose, maternal plasma and breastmilk samples were obtained prior to the morning dose and 2, 4 and 6 hours after the dose. One hundred seventeen of the 121 breastmilk samples contained detectable quantities (10 mcg/L or greater) of lopinavir, with a median breastmilk concentration of 1.43 mg/L over the 6 hours.[7]
Nine HIV-positive women about to undergo cesarean section received 3 doses of lopinavir 200 mg, ritonavir 150 mg, zidovudine 300 mg, lamivudine 50 mg at 3 hour intervals before the procedure. Breastmilk samples were collected at a mean of 25 hours postpartum. In the 8 women where it was quantified, the average milk concentration of lopinavir was 4263 mcg/L (range 1143 to 5573 mcg/L).[8]
Mothers who were taking lopinavir 400 mg with ritonavir 100 mg twice daily hand-expressed breastmilk 1 to 2 hours after the morning dose at 1, 3 and 6 months postpartum. Median breastmilk lopinavir concentrations were 530 mcg/L (n = 6), 650 mcg/L (n = 8), 590 mcg/L (n = 8) at 1, 3 and 6 months, respectively. The weight-adjusted infant dosage was calculated to be 0.23% at 6 months.[9]
Infant Levels. Breastfed infants of 9 mothers who were receiving lopinavir 400 mg plus ritonavir 100 mg twice daily as part of a combination antiretroviral regimen had a total of 6 blood samples analyzed at 1 month, 3 months and/or 6 months postpartum. Samples were collected at a median of 4.5 hours (range 3.5 to 6 hours) after the previous maternal dose and a median of 30 minutes (range 20 to 60 minutes) after the previous nursing. The infants' median lopinavir plasma concentrations was 105 mcg/L (range 12 to 518 mcg/L), which was a median of 8% (range 0 to 16%) of the maternal serum concentration.[5]
Five infants were breastfed either partially or exclusively by their mothers who had been taking lopinavir 400 mg twice daily for 53 to 182 days as part of a drug combination that included ritonavir, zidovudine, and lamivudine. Infant blood was collected at a median of 1 month postpartum at 11 to 16 hours after the last dose and a median of 1 hour (range 6 minutes to 35 hours) after the last breastfeeding. Two of five infants had measurable lopinavir plasma levels of <1 mg/L.[6]
Lopinavir was measured in 117 breastfed (90% exclusive) infants whose mothers were taking lopinavir plus ritonavir for HIV infection during pregnancy and postpartum. At 8 weeks postpartum, only 2% had detectable lopinavir in their plasma at a mean concentration of 0.17 mg/L. At 12 weeks postpartum, none of the infants had detectable lopinavir in their plasma, and 96% of infants had detectable lopinavir in their hair samples at a mean concentration of 5.1 ng/mg of hair (range 0.13 to 15.8 ng/mg). The authors interpreted the results to mean that infants receive negligible exposure to lopinavir during breastfeeding.[10]
Thirty nursing mothers were studied at 6, 12 or 24 weeks postpartum (10 at each time). Each mother was taking lopinavir 400 mg twice daily by mouth starting at delivery. Infant plasma samples were obtained before their mother's first dose and at 2, 4 and 6 hours after the mother's dose. Infants were allowed to breastfeed ad libitum during the study period. Lopinavir was undetectable (<10 mcg/L) in all of the 115 infant plasma samples.[7]
Mother-infant pairs were studied among mothers taking lopinavir 400 mg with ritonavir 100 mg twice daily as part of a multi-drug HIV regimen. Infants were breastfed (extent not stated) and plasma concentrations were measured postpartum. Median plasma lopinavir concentrations at 1 (n = 3), 3 (n = 9), and 6 months (n = 8) were all less than the lower limit of quantification of 264 mcg/L. Only 2 samples had measurable lopinavir.[9]
Effects in Breastfed Infants
A study compared the rates of severe anemia in 3 groups of infants who received postpartum prophylaxis with zidovudine for prevention of maternal-to-child transmission of HIV infection. Through 6 months of age, breastfed infants whose mothers received HAART had a higher rate of severe anemia (7.4%) than breastfed infants whose mothers received only zidovudine (5.3%). Formula-fed infants had the lowest rate of severe anemia (2.5%). The anemia generally responded well to iron and multivitamin supplementation, and discontinuation of zidovudine.[11]
An unblinded study in Uganda compared the outcomes of breastfed infants and their HIV-positive mothers who were randomized to receive antiretroviral therapy that was based either on efavirenz 600 mg once daily or lopinavir 400 mg plus ritonavir 100 mg twice daily during breastfeeding. All mothers received lamivudine 150 mg, zidovudine 300 mg twice daily and trimethoprim-sulfamethoxazole once daily. All infants received prophylaxis with either zidovudine for 1 week or nevirapine for 6 weeks, plus trimethoprim-sulfamethoxazole from 6 weeks of age to 6 weeks after weaning. Almost all of the infants were exclusively breastfed until 6 months of age and about 73% were partially breastfed until 12 months of age. There was no statistical difference in hospitalizations or adverse events including anemia, neutropenia or deaths among infants in the two groups.[12]
Among 9 breastfed (extent not stated) infants whose mothers were taking lopinavir 400 mg with ritonavir 100 mg twice daily as part of a multi-drug treatment for HIV infection, no adverse effects were noted by investigators or reported by mothers at 1, 3 and 6 months of age.[9]
Effects on Lactation and Breastmilk
Gynecomastia has been reported among men receiving highly active antiretroviral therapy. Gynecomastia is unilateral initially, but progresses to bilateral in about half of cases. No alterations in serum prolactin were noted and spontaneous resolution usually occurred within one year, even with continuation of the regimen.[13-15] Some case reports and in vitro studies have suggested that protease inhibitors might cause hyperprolactinemia and galactorrhea in some male patients,[16,17] although this has been disputed.[18] The relevance of these findings to nursing mothers is not known. The prolactin level in a mother with established lactation may not affect her ability to breastfeed.
References
- 1.
- Kariyawasam D, Peries M, Foissac F, et al. Lopinavir-ritonavir impairs adrenal function in infants. Clin Infect Dis 2020;71:1030-9. [PubMed: 31633158]
- 2.
- World Health Organization. Consolidated guidelines on HIV prevention, testing, treatment, service delivery and monitoring: recommendations for a public health approach. 2021. https://www
.who.int/publications /i/item/9789240031593 [PubMed: 34370423] - 3.
- Department of Health and Human Services. Recommendations for the use of antiretroviral drugs during pregnancy and interventions to reduce perinatal HIV transmission in the United States. Infant feeding for individuals with HIV in the United States. 2023. https:
//clinicalinfohivgov /en/guidelines /perinatal/infant-feeding-individuals-hiv-united-states?view=full - 4.
- Rezk NL, White N, Bridges AS, et al. Studies on antiretroviral drug concentrations in breast milk: Validation of a liquid chromatography-tandem mass spectrometric method for the determination of 7 anti-human immunodeficiency virus medications. Ther Drug Monit 2008;30:611-9. [PMC free article: PMC2901847] [PubMed: 18758393]
- 5.
- Palombi L, Pirillo MF, Andreotti M, et al. Antiretroviral prophylaxis for breastfeeding transmission in Malawi: drug concentrations, virological efficacy and safety. Antivir Ther 2012;17:1511-9. [PubMed: 22910456]
- 6.
- Shapiro RL, Rossi S, Ogwu A, et al. Therapeutic levels of lopinavir in late pregnancy and abacavir passage into breast milk, in the Mma Bana Study, Botswana. Antivir Ther 2013;18:585-90. [PMC free article: PMC5502724] [PubMed: 23183881]
- 7.
- Corbett AH, Kayira D, White NR, et al. Antiretroviral pharmacokinetics in mothers and breastfeeding infants from 6 to 24 weeks post-partum: Results of the BAN Study. Antivir Ther 2014;19:587-95. [PMC free article: PMC4110187] [PubMed: 24464632]
- 8.
- Ramírez-Ramírez A, Sanchez-Serrano E, Loaiza-Flores G, et al. Simultaneous quantification of four antiretroviral drugs in breast milk samples from HIV-positive women by an ultra-high performance liquid chromatography tandem mass spectrometry (UPLC-MS/MS) method. PLoS One 2018;13:e0191236. [PMC free article: PMC5774716] [PubMed: 29351333]
- 9.
- Oumar AA, Bagayoko-Maiga K, Bahachimi A, et al. Efavirenz and lopinavir levels in HIV-infected women and their nursing infants, in Mali. J Pharmacol Exp Ther 2018;366:479-84. [PubMed: 29986950]
- 10.
- Gandhi M, Mwesigwa J, Aweeka F, et al. Hair and plasma data show that lopinavir, ritonavir, and efavirenz all transfer from mother to infant in utero, but only efavirenz transfers via breastfeeding. J Acquir Immune Defic Syndr 2013;63:578-84. [PMC free article: PMC3800282] [PubMed: 24135775]
- 11.
- Dryden-Peterson S, Shapiro RL, Hughes MD, et al. Increased risk of severe infant anemia following exposure to maternal HAART, Botswana. J Acquir Immune Defic Syndr 2011;56:428-36. [PMC free article: PMC3112252] [PubMed: 21266910]
- 12.
- Cohan D, Natureeba P, Koss CA, et al. Efficacy and safety of lopinavir/ritonavir versus efavirenz-based antiretroviral therapy in HIV-infected pregnant Ugandan women. AIDS 2015;29:183-91. [PMC free article: PMC4428759] [PubMed: 25426808]
- 13.
- García-Benayas T, Blanco F, Martin-Carbonero L, et al. Gynecomastia in HIV-infected patients receiving antiretroviral therapy. AIDS Res Hum Retroviruses 2003;19:739-41. [PubMed: 14585204]
- 14.
- Pantanowitz L, Evans D, Gross PD, Dezube BJ. HIV-related gynecomastia. Breast J 2003;9:131-2. [PubMed: 12603389]
- 15.
- Evans DL, Pantanowitz L, Dezube BJ, Aboulafia DM. Breast enlargement in 13 men who were seropositive for human immunodeficiency virus. Clin Infect Dis 2002;35:1113-9. [PubMed: 12384846]
- 16.
- Hutchinson J, Murphy M, Harries R, Skinner CJ. Galactorrhoea and hyperprolactinaemia associated with protease-inhibitors. Lancet 2000;356:1003-4. [PubMed: 11041407]
- 17.
- Orlando G, Brunetti L, Vacca M. Ritonavir and saquinavir directly stimulate anterior pituitary prolactin secretion, in vitro. Int J Immunopathol Pharmacol 2002;15:65-8. [PubMed: 12593790]
- 18.
- Montero A, Bottasso OA, Luraghi MR, et al. Galactorrhoea, hyperprolactinaemia, and protease inhibitors. Lancet 2001;357:473-5. [PubMed: 11273087]
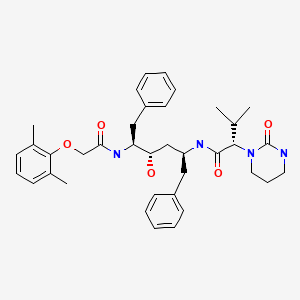
Substance Identification
Substance Name
Lopinavir
CAS Registry Number
192725-17-0
Drug Class
Breast Feeding
Milk, Human
Anti-Infective Agents
Antiviral Agents
Anti-HIV Agents
Anti-Retroviral Agents
HIV Protease Inhibitors
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Ritonavir.[Drugs and Lactation Database (...]Review Ritonavir.. Drugs and Lactation Database (LactMed®). 2006
- Review Saquinavir.[Drugs and Lactation Database (...]Review Saquinavir.. Drugs and Lactation Database (LactMed®). 2006
- Review Nelfinavir.[Drugs and Lactation Database (...]Review Nelfinavir.. Drugs and Lactation Database (LactMed®). 2006
- Review Tipranavir.[Drugs and Lactation Database (...]Review Tipranavir.. Drugs and Lactation Database (LactMed®). 2006
- Review Fosamprenavir.[Drugs and Lactation Database (...]Review Fosamprenavir.. Drugs and Lactation Database (LactMed®). 2006
- Lopinavir - Drugs and Lactation Database (LactMed®)Lopinavir - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
