Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 30516-87-1
Drug Levels and Effects
Summary of Use during Lactation
Zidovudine has been well studied during breastfeeding. Milk levels are low and most breastfed infants do not have detectable blood levels. Some breastfed infants have developed anemia during maternal therapy. Achieving and maintaining viral suppression with antiretroviral therapy decreases breastfeeding transmission risk to less than 1%, but not zero. Individuals with HIV who are on antiretroviral therapy with a sustained undetectable viral load and who choose to breastfeed should be supported in this decision. If a viral load is not suppressed, banked pasteurized donor milk or formula is recommended.[1,2]
Drug Levels
Maternal Levels. Six women were given a single oral dose of 200 mg of zidovudine. Milk samples were collected 1, 2, 4 and 6 hours after the dose. The peak milk concentration occurred 1 to 2 hours after the dose in 4 women and occurred 1 hour later in the others. The average peak milk concentration was 857 mcg/L (range 472 to 1043 mcg/L).[3]
Eighteen women who were receiving oral zidovudine 300 mg twice daily as part of a combination antiretroviral regimen had their milk analyzed at either 2 or 5 months postpartum. Milk samples were provided at a median of 4 hours (range 1 to 8.5 hours) after the last dose. The median zidovudine concentration in breastmilk was 207 mcg/L.[4]
Forty women were given postpartum prophylaxis with unstated dosages of lamivudine, nevirapine and zidovudine (or stavudine if the hemoglobin <8 g/dL). Blood and milk samples were collected once during the first 3 days postpartum and once at 7 days postpartum. The median times after a dose that samples were collected were 5.3 hours (range 0 to 99 hours) for the first sample and 6 hours (range 4.3 to 20 hours) for the 7-day sample. Average breastmilk zidovudine concentrations were calculated only for samples that had detectable (>20 mcg/L) concentrations of zidovudine. The mean breastmilk concentrations were 130 (n = 11) and 150 mcg/L (n = 13), respectively, at the two sampling times, which was equal to the simultaneous maternal serum concentrations.[5]
Fifty-eight mothers who were taking a combination regimen of lamivudine, nevirapine and zidovudine had their serum and breastmilk analyzed for the presence of these drugs. Mothers took zidovudine 200 mg twice daily starting at 34 to 36 weeks postpartum and continuing until 6 months postpartum. Breastmilk was collected within 24 hours after delivery and at 2, 6, 14 and 24 weeks postpartum at variable times after the previous dose. The median breastmilk zidovudine concentration in 35 selected samples across all visits was 9 mcg/L.[6]
Thirty-eight mothers who were receiving zidovudine 300 mg twice daily as part of a combination antiretroviral regimen provided a total of 114 milk samples at birth, 1 month, 3 months and/or 6 months postpartum. Milk samples were collected at a median of 4.5 hours (range 3.5 to 6 hours) after the previous dose. The median breastmilk zidovudine concentration was 33 mcg/L (range 5 to 117 mcg/L).[7]
Fifteen women had been taking zidovudine 300 mg twice daily for 53 to 182 days as part of a drug combination that included ritonavir, zidovudine, and lamivudine. Breastmilk samples were collected at just before a dose at a median of 1 month postpartum. Whole breastmilk levels contained a median of 7 mcg/L of zidovudine.[8]
Thirty women were studied at 6, 12 or 24 weeks postpartum (10 at each time). Each mother was taking zidovudine 300 mg, lamivudine 150 mg, lopinavir 400 mg, and ritonavir 100 mg twice daily by mouth starting at delivery. On the study day, at a median of 14.9 hours after the previous evening's dose, maternal plasma and breastmilk samples were obtained prior to the morning dose and 2, 4 and 6 hours after the dose. Ninety-eight of the 121 breastmilk samples contained detectable quantities (10 mcg/L or greater) of zidovudine, with a median breastmilk concentration of 0.2 mg/L over the 6 hours.[9]
Nine HIV-positive women about to undergo cesarean section received 3 doses of lopinavir 200 mg, ritonavir 150 mg, zidovudine 300 mg, lamivudine 50 mg at 3 hour intervals before the procedure. Breastmilk samples were collected at a mean of 25 hours postpartum. The average milk concentration of zidovudine was 101mcg/L (range 20 to 448 mcg/L).[10]
Infant Levels. Eighteen nursing mothers were receiving oral zidovudine 300 mg twice daily as part of a combination antiretroviral regimen. Their infants had serum concentrations determined at either 2 or 5 months postpartum. Serum samples were provided at a median of 4 hours (range 1 to 8.5 hours) after the last dose. The infants were also receiving oral zidovudine 4 or 6 mg/kg 3 times daily, depending on their age. The median infant serum zidovudine concentration was 123 mcg/L (range 14 to 3302 mcg/L). The average value was 25 times the IC50 for HIV.[4]
Fifty-eight infants whose mothers were taking a combination regimen of lamivudine, nevirapine and zidovudine had their serum analyzed for the presence of these drugs. Mothers took zidovudine 200 mg twice daily starting at 34 to 36 weeks postpartum and continuing until 6 months postpartum and were instructed to exclusively breastfeed for 5.5 months. Serum samples were collected within 24 hours after delivery and at 2, 6, 14 and 24 weeks postpartum. Median serum concentration of 16 selected dried blood spot samples was 24 mcg/L. At later times postpartum, zidovudine was not detectable (<30 mcg/L) in 66 infant dried blood spots.[6]
Breastfed infants of 38 mothers who were receiving zidovudine 300 mg twice daily as part of a combination antiretroviral regimen had a total of 34 blood samples analyzed at 1 month, 3 months and/or 6 months postpartum. Samples were collected at a median of 4.5 hours (range 3.5 to 6 hours) after the previous maternal dose and a median of 30 minutes (range 20 to 60 minutes) after the previous nursing. The infants' zidovudine plasma concentrations ranged from 0 to 2.5 mcg/L, which was a median of 2% (range 0 to 5%) of the maternal serum concentration.[7]
Thirty-three infants were breastfed either partially or exclusively by their mothers who had been taking zidovudine 300 mg twice daily as part of a drug combination. Infant blood was collected at a median of 1 month postpartum for 24 infants and at 3 months postpartum for 9 infants at various times after the last dose and a median of 1 hour (range 6 minutes to 35 hours) after the last breastfeeding. None of the infants had detectable zidovudine levels in their serum (<45 mcg/L).[8]
Thirty nursing mothers were studied at 6, 12 or 24 weeks postpartum (10 at each time). Each mother was taking zidovudine 300 mg twice daily by mouth starting at delivery. Infant plasma samples were obtained before their mother's first dose and at 2, 4 and 6 hours after the mother's dose. Infants were allowed to breastfeed ad libitum during the study period. Zidovudine was undetectable (<10 mcg/L) in all of the 115 infant plasma samples.[9]
Effects in Breastfed Infants
A study assigned pregnant women to zidovudine alone or highly-active antiretroviral therapy (HAART: zidovudine, lamivudine and nevirapine) to prevent maternal-to-child transmission of HIV infection. After delivery, all infants received one month of zidovudine prophylaxis; some infants were breastfed and others were formula fed. A higher percentage of infants in the HAART-exposed group had neutropenia than those in the unexposed group at 1 month of age (15.9% and 3.7%, respectively). Hematologic toxicity was transient and asymptomatic. From 2 to 6 months postpartum, no differences in hematologic toxicity were seen between breastfed and formula-fed infants. No statistical difference in hepatic toxicity was seen between the breastfed and formula-fed infants.[11]
A study compared the rates of severe anemia in 3 groups of infants who received postpartum prophylaxis with zidovudine for prevention of maternal-to-child transmission of HIV infection. Through 6 months of age, breastfed infants whose mothers received HAART had a higher rate of severe anemia (7.4%) than breastfed infants whose mothers received only zidovudine (5.3%). Formula-fed infants had the lowest rate of severe anemia (2.5%). The anemia generally responded well to iron and multivitamin supplementation, and discontinuation of zidovudine.[12]
Effects on Lactation and Breastmilk
Relevant published information was not found as of the revision date.
References
- 1.
- World Health Organization. Consolidated guidelines on HIV prevention, testing, treatment, service delivery and monitoring: Recommendations for a public health approach. 2021. https://www
.who.int/publications /i/item/9789240031593 [PubMed: 34370423] - 2.
- Department of Health and Human Services. Recommendations for the use of antiretroviral drugs during pregnancy and interventions to reduce perinatal HIV transmission in the United States. 2024. https:
//clinicalinfo .hiv.gov/sites/default /files/guidelines/documents /perinatal-hiv /guidelines-perinatal.pdf - 3.
- Ruff A, Hamzeh F, Lietman P, et al. Excretion of zidovudine (ZDV) in human breast milk. 34th Interscience Conference on Antimicrobial Agents and Chemotherapy Orlando, FL October 4-7, 1995.
- 4.
- Shapiro RL, Holland DT, Capparelli E, et al. Antiretroviral concentrations in breast-feeding infants of women in Botswana receiving antiretroviral treatment. J Infect Dis 2005;192:720-7. [PubMed: 16088821]
- 5.
- Giuliano M, Guidotti G, Andreotti M, et al. Triple antiretroviral prophylaxis administered during pregnancy and after delivery significantly reduces breast milk viral load study within the Drug Resource Enhancement Against AIDS and Malnutrition Program. J Acquir Immune Defic Syndr 2007;44:286-91. [PubMed: 17146372]
- 6.
- Mirochnick M, Thomas T, Capparelli E, et al. Antiretroviral concentrations in breast-feeding infants of mothers receiving highly active antiretroviral therapy. Antimicrob Agents Chemother 2009;53:1170-6. [PMC free article: PMC2650559] [PubMed: 19114673]
- 7.
- Palombi L, Pirillo MF, Andreotti M, et al. Antiretroviral prophylaxis for breastfeeding transmission in Malawi: drug concentrations, virological efficacy and safety. Antivir Ther 2012;17:1511-9. [PubMed: 22910456]
- 8.
- Shapiro RL, Rossi S, Ogwu A, et al. Therapeutic levels of lopinavir in late pregnancy and abacavir passage into breast milk, in the Mma Bana Study, Botswana. Antivir Ther 2013;18:585-90. [PMC free article: PMC5502724] [PubMed: 23183881]
- 9.
- Corbett AH, Kayira D, White NR, et al. Antiretroviral pharmacokinetics in mothers and breastfeeding infants from 6 to 24 weeks post-partum: Results of the BAN Study. Antivir Ther 2014;19:587-95. [PMC free article: PMC4110187] [PubMed: 24464632]
- 10.
- Ramírez-Ramírez A, Sanchez-Serrano E, Loaiza-Flores G, et al. Simultaneous quantification of four antiretroviral drugs in breast milk samples from HIV-positive women by an ultra-high performance liquid chromatography tandem mass spectrometry (UPLC-MS/MS) method. PLoS One 2018;13:e0191236. [PMC free article: PMC5774716] [PubMed: 29351333]
- 11.
- Bae WH, Wester C, Smeaton LM, et al. Hematologic and hepatic toxicities associated with antenatal and postnatal exposure to maternal highly active antiretroviral therapy among infants. AIDS 2008;22:1633-40. [PMC free article: PMC2664540] [PubMed: 18670224]
- 12.
- Dryden-Peterson S, Shapiro RL, Hughes MD, et al. Increased risk of severe infant anemia following exposure to maternal HAART, Botswana. J Acquir Immune Defic Syndr 2011;56:428-36. [PMC free article: PMC3112252] [PubMed: 21266910]
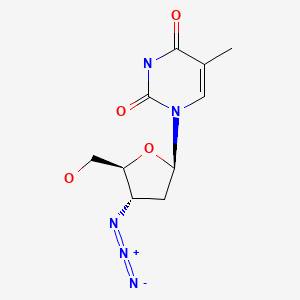
Substance Identification
Substance Name
Zidovudine
CAS Registry Number
30516-87-1
Drug Class
Breast Feeding
Lactation
Milk, Human
Anti-Infective Agents
Antiviral Agents
Anti-HIV Agents
Anti-Retroviral Agents
Reverse Transcriptase Inhibitors
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Lamivudine.[Drugs and Lactation Database (...]Review Lamivudine.. Drugs and Lactation Database (LactMed®). 2006
- Review Emtricitabine.[Drugs and Lactation Database (...]Review Emtricitabine.. Drugs and Lactation Database (LactMed®). 2006
- Review Didanosine.[Drugs and Lactation Database (...]Review Didanosine.. Drugs and Lactation Database (LactMed®). 2006
- Review Abacavir.[Drugs and Lactation Database (...]Review Abacavir.. Drugs and Lactation Database (LactMed®). 2006
- Review Raltegravir.[Drugs and Lactation Database (...]Review Raltegravir.. Drugs and Lactation Database (LactMed®). 2006
- Zidovudine - Drugs and Lactation Database (LactMed®)Zidovudine - Drugs and Lactation Database (LactMed®)
- Mefenamic Acid - Drugs and Lactation Database (LactMed®)Mefenamic Acid - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
