Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 113-42-8
Drug Levels and Effects
Summary of Use during Lactation
Limited information indicates that maternal doses of methylergonovine up to 0.75 mg daily produce low levels in milk. Product labeling in the U.S. currently recommends avoiding breastfeeding for 12 hours following the last dose of methylergonovine. This warning appears to be based on unpublished adverse reactions in breastfed infants after several days of maternal methylergonovine therapy. The use of shorter courses of the drug after delivery during the colostral phase of lactation are not expected to transfer appreciable amounts of drug to the breastfed infant or risk adverse effects in the infant. The lack of infant side effects was documented in one case-control study.
Long courses of methylergonovine, especially after the milk comes in, are best avoided in mothers who wish to nurse. When they are required, withholding breast feeding for 12 hours following the last dose of methylergonovine is prudent. If adverse reactions in the breastfed infant are seen, such as tachycardia, vomiting, diarrhea or agitation, the drug should be discontinued. Some sources recommend avoiding methylergonovine altogether during breastfeeding.[1]
Although results of several imperfect studies are somewhat mixed, it appears that methylergonovine can decrease serum prolactin and possibly the amount of milk production and duration of lactation, especially when used in the immediate postpartum period. The effect seems to be related to the dosage and route of administration, with injected doses having a greater impact than oral. A short course immediately postpartum does not appear to have a detrimental effect on lactation.
Drug Levels
Maternal Levels. After a regimen of oral methylergonovine 0.125 mg 3 times daily for 5 days, a single oral dose of 0.25 mg was given to 8 women. Milk levels 1 hour after the dose ranged from undetectable in 4 women (<0.5 mcg/L) to 1.3 mcg/L. By 8 hours after the dose, 7 women had undetectable milk levels, although it was 1.2 mcg/L in one individual. The authors estimated that the maximum dosage a breastfed infant would receive after a 7.5 mg daily maternal dosage would be 1.3 mcg which is about 0.3% of the adult dosage.[2]
Methylergonovine maleate 0.75 mg daily was administered to postpartum women for 4 days. The exact dosage regimen and number of women were not reported. Two hours after the last dose, milk samples contained 1.3 mcg/L of methylergonovine.[3]
Ten women who averaged 4.8 days postpartum received a single oral dose of methylergonovine 250 mcg. Milk samples were obtained from one breast from 0.5 to 5 hours after the dose. Average milk levels were 368 ng/L and 527 ng/L at 1 and 2 hours after the dose, respectively. The mean peak milk level was 657 ng/L (range 410-830 ng/L), at 1.8 hours after the dose. In 2 women, the peak milk level occurred 3 hours after the dose. By 5 hours, the average milk level was 200 ng/L. The half-life in breastmilk averaged 2.3 hours.[4]
Twelve mothers were treated with methylergonovine 0.125 mg three times daily for 5 days to treat incomplete postpartum uterine involution. The mothers collected eleven 3 mL samples of milk after an oral dose of 0.125 mg of methylergonovine over the following 12 hours. The average peak milk level was 437 ng/L at 2 hours after the dose. Milk levels fell to an average of 86 ng/L at 5 hours after the dose and were undetectable (<50 ng/L) at 6 hours and thereafter.[5]
Infant Levels. Relevant published information was not found as of the revision date.
Effects in Breastfed Infants
According to the manufacturer, there are isolated reports of adverse effects in breast-fed infants whose mothers were receiving methylergonovine for several days. One or more of the following symptoms were observed during methylergonovine therapy and disappeared upon withdrawal of the medication: elevated blood pressure, bradycardia, tachycardia, vomiting, diarrhea, restlessness, or clonic cramps. Another case reported to the manufacturer was a breast-fed infant who presented with seizures after about 4 to 6 days of maternal methylergonovine therapy. The infant's seizures began on the second day of treatment of the mother after breastfeeding. Medications were discontinued per the mother. The infantile seizures resolved about six weeks later.[6] It is not possible to determine the causality of any of the adverse effects with the information available.
A working group of the French national medication safety agency (ANSM) reported 23 cases of infants exposed to methylergonovine via breastmilk who had a total of 44 adverse reactions. (Some of these might be the same as those reported in the previous paragraph.) The working group considered tachycardia, vomiting, diarrhea and agitation to be sufficiently well documented to add to the prescribing information.[7]
A prospective case-control study compared the outcome of infants whose mothers had taken methylergonovine postpartum 0.125 mg 2 times daily for 5 days or 3 times daily for 3 days to mothers who had taken amoxicillin which served as a control group. Of 29 mothers who had taken methylergonovine, there were no differences in neonatal health or development at follow-up at 17 months postpartum between the treatment and control groups.[8]
Effects on Lactation and Breastmilk
Oral methylergonovine in a dose of 0.2 mg 3 times daily for 7 days in 10 postpartum subjects caused no difference in serum prolactin concentrations from placebo administered to 10 postpartum control women. No significant difference found in the daily milk volumes between the groups.[9]
A single intramuscular injection of methylergonovine 0.2 mg given to 4 women on day 3 postpartum caused a decrease in serum prolactin beginning 45 to 60 minutes after the dose. For 2 to 3 hours after the dose, serum prolactin levels remained about 50% lower than baseline levels.[10]
A single intramuscular injection of methylergonovine 0.2 mg was given to 14 women during the first 1.5 hours postpartum. At 80 to 90 minutes after the injection, the normal postpartum rise in serum prolactin was 56% in the women who received methylergonovine compared to a 285% in serum prolactin in women who received a placebo injection. Six treated women had no increase in serum prolactin compared to 2 of the control women.[11]
Thirty women who delivered fullterm infants received a single intramuscular dose of methylergonovine 0.2 mg after delivery, followed by oral ergotamine 1 mg 3 times daily for 6 days. Compared to 28 women who delivered fullterm infants and received no ergot derivatives, there was no difference in the milk production, as measured by weight differences before and after nursing, between the 2 groups during the first 6 days postpartum.[12]
Thirty postpartum women were given methylergonovine 0.2 mg orally 3 times daily for the first 7 days postpartum. Baseline (prior to nursing) serum prolactin was no different from those of 30 postpartum women who received no methylergonovine on days 1 and 3 postpartum. However, on day 7 postpartum, serum prolactin levels were significantly less in the treated women. Milk production was also reduced in the treated women on days 3 and 7 postpartum compared to controls.[13]
Ten women received a single intravenous dose of 0.4 mg of methylergonovine immediately postpartum were compared to 10 control mothers who received no methylergonovine; all women received a continuous infusion of oxytocin postpartum. None of the women were allowed to nurse or extract milk from their breasts or to receive hormones to suppress lactation. Serum prolactin measured during labor, immediately after administration of the drug and daily at 9 am for 5 days postpartum found no statistical differences in prolactin levels between the 2 groups.[14]
In a randomized study, 48 patients were given methylergonovine 0.125 mg orally every 8 hours for the first 7 days postpartum. Another 44 in the same hospital were not given methylergonovine. No statistical differences were found in the serum levels of prolactin at 3 days postpartum between the groups, although women with normal deliveries had higher prolactin levels than those delivered by cesarean section. At 1 month postpartum, no differences were found in the percentage of exclusive breastfeeding or in the weight gain of infants.[15]
In a prospective, randomized study, 444 postpartum mothers were given 0.125 mg of methylergonovine 3 times a day, while 436 were given placebo. Milk production among untreated women averaged 880 grams during the first 6 days, while among treated patients it was only 563 grams. After 4 weeks there were still differences in the quantity of milk produced.[16]
A prospective case-control study compared lactation in mothers had taken methylergonovine postpartum 0.125 mg 2 times daily for 5 days or 3 times daily for 3 days to mothers who had taken amoxicillin which served as a control group. The rates of exclusive breastfeeding and reports of decreased lactation were not significantly different in the two groups.[8]
References
- 1.
- Anon. Methylergometrine: Adverse effects in breastfed infants. Prescrire Int. 2014;23:102. [PubMed: 24860899]
- 2.
- Erkkola R, Kanto J et al. Excretion of methylergometrine (methylergonovine) into the human breast milk. Int J Clin Pharmacol Biopharm. 1978;16:579-80. [PubMed: 730424]
- 3.
- Iwamura S, Kambegawa A. Determination of methylergometrine and dihydroergotoxine in biological fluids. J Pharmacobiodyn. 1981;4:275-81. [PubMed: 7264872]
- 4.
- Vogel D, Burkhardt T, Rentsch K et al. Misoprostol versus methylergometrine: pharmacokinetics in human milk. Am J Obstet Gynecol. 2004;191:2168-73. [PubMed: 15592308]
- 5.
- Nakamichi T, Yawata A, Hojo H et al. Monitoring of methylergometrine in human breast milk by solid-phase extraction and high-performance liquid chromatography with fluorimetric detection. Pharmazie. 2012;67:482-4. [PubMed: 22822533]
- 6.
- Nandan Wadgaonkar. Novartis Pharmaceuticals. Personal Communication to Philip Anderson: September 27, 2012.
- 7.
- ANSM. Groupe de Travail Reproduction, Grossesse et Allaitement. Seance du 5 avril 2013 de 13h00 a 17h00. October 29, 2013. Document GT252013013. Accessed June 20, 2014. http://ansm
.sante.fr /searchengine/detail/%28cis%29/66417119. - 8.
- Gilad O, Merlob P, Stahl B et al. Outcome of breastfed infants following post-partum methylergonovine treatment. J Matern Fetal Neonatal Med. 2017;30:1569-73. [PubMed: 27846760]
- 9.
- del Pozo E, Brun del Re RB, Hinselmann M. Lack of effect of methyl-ergonovine on postpartum lactation. Am J Obstet Gynecol. 1975;123:845-6. [PubMed: 1200082]
- 10.
- Perez-Lopez FR, Delvoye P, Denayer P et al. Effect of methylergobasine maleate on serum gonadotrophin and prolactin in humans. Acta Endocrinol (Copenh). 1975;79:644-57. [PubMed: 1174274]
- 11.
- Weiss G, Klein S et al. Effect of methylergonovine on puerperal prolactin secretion. Obstet Gynecol. 1975;46:209-10. [PubMed: 1080266]
- 12.
- Jolivet A, Robyn C et al. [Effect of ergot alkaloid derivatives on milk secretion in the immediate postpartum period]. J Gynecol Obstet Biol Reprod (Paris). 1978;7:129-34. [PubMed: 641312]
- 13.
- Peters F, Lummerich M, Breckwoldt M. Inhibition of prolactin and lactation by methylergometrine hydrogenmaleate. Acta Endocrinol (Copenh). 1979;91:213-6. [PubMed: 463447]
- 14.
- del Castillo FJ, Ramirez BM, Diaz-Infante Ibarra A. [Effect of methylergovine on the secretion of prolactin in childbirth and the puerperium]. Ginecol Obstet Mex. 1980;48:311-6. [PubMed: 7250712]
- 15.
- Gonzalez P, Gayan P et al. [Plasma prolactin in the puerperium and its relation to the use of methylergonovine maleate.] Rev Chil Obstet Ginecol. 1984;49:149-55. [PubMed: 6543471]
- 16.
- Arabin B, Ruttgers H, Kubli F. [Effects of routine administration of methylergometrine during puerperium on involution, maternal morbidity and lactation]. Geburtshilfe Frauenheilkd. 1986;46:215-20. [PubMed: 3519353]
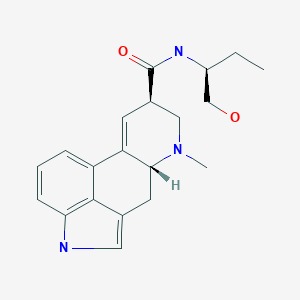
Substance Identification
Substance Name
Methylergonovine
CAS Registry Number
113-42-8
Drug Class
- Breast Feeding
- Ergot Alkaloids
- Oxytocics
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Ergonovine.[Drugs and Lactation Database (...]Review Ergonovine.. Drugs and Lactation Database (LactMed®). 2006
- Review Cabergoline.[Drugs and Lactation Database (...]Review Cabergoline.. Drugs and Lactation Database (LactMed®). 2006
- Review Ethambutol.[Drugs and Lactation Database (...]Review Ethambutol.. Drugs and Lactation Database (LactMed®). 2006
- Review Cyclosporine.[Drugs and Lactation Database (...]Review Cyclosporine.. Drugs and Lactation Database (LactMed®). 2006
- Review Fentanyl.[Drugs and Lactation Database (...]Review Fentanyl.. Drugs and Lactation Database (LactMed®). 2006
- Methylergonovine - Drugs and Lactation Database (LactMed®)Methylergonovine - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
