Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 59-92-7
Drug Levels and Effects
Summary of Use during Lactation
Limited data indicate that levodopa is poorly excreted into breastmilk and that the sustained-release product may result in a smaller amount of drug transferred to the breastfed infant than with the immediate-release product. Several studies indicate that levodopa can decrease serum prolactin during lactation. The prolactin level in a mother with established lactation may not affect her ability to breastfeed. The effect of long-term use of levodopa on breastfeeding has not been adequately evaluated, although some mothers were able to successfully breastfeed her infant without apparent harm while using relatively low doses of levodopa and carbidopa for Parkinson's disease.
Drug Levels
Maternal Levels. One mother with Parkinson's disease took sustained-release levodopa 200 mg and carbidopa 50 mg 4 times daily. At 4.5 months postpartum, milk levodopa levels were measured after a morning dose of the drug. The peak levodopa milk level occurred 3 hours after the dose at a concentration of 315 mcg/L and returned to baseline of about 200 mcg/L 6 hours after the dose. On a different day, the same mother was given a single dose of immediate-release levodopa 200 mg and carbidopa 50 mg. The peak levodopa milk level occurred 3 hours after the dose at a concentration of 683 mcg/L and returned to baseline of about 220 mcg/L 6 hours after the dose. The infant was breastfed and weighed before and after each feeding. The infant ingested 0.127 mg and 0.181 mg of levodopa after maternal intake of the sustained- and immediate-release products, respectively.[1] Using data in the article, the infant would receive an average of about 0.3% of the maternal weight-adjusted dosage with the sustained release product and 0.5% of the maternal weight-adjusted dosage with the immediate-release product.
Infant Levels. Relevant published information was not found as of the revision date.
Effects in Breastfed Infants
One mother with Parkinson's disease took sustained-release levodopa 200 mg and carbidopa 50 mg 4 times daily. She successfully breastfed her infant whose development was normal at 2 years of age.[1]
A 37-year-old Israeli woman with Parkinson's disease became pregnant while taking a continuous infusion of levodopa 20 mg/mL and carbidopa 5 mg/mL gel. She breastfed her infant for 3 months while receiving the drug, although the extent of breastfeeding and the dosage of the gel is not clear from the paper. At 10 months of age, the infant's psychomotor development was deemed to be normal.[2]
Effects on Lactation and Breastmilk
Levodopa decreases serum prolactin in normal women and those with hyperprolactinemia and can suppress inappropriate lactation in galactorrhea, although not consistently.[3-11] The prolactin level in a mother with established lactation may not affect her ability to breastfeed.
One mother with Parkinson's disease took sustained-release levodopa 200 mg and carbidopa 50 mg 4 times daily. She successfully breastfed her infant.[1]
On postpartum day 3, 5 women were given a single oral dose of 500 mg of levodopa or bromocriptine 5 mg followed by a single oral dose of metoclopramide 10 mg 3 hours later. Bromocriptine suppressed basal serum prolactin to a greater extent than levodopa. Over the next 3 hours, serum prolactin increased after metoclopramide in the patients who received levodopa, but not in those who received bromocriptine.[12]
Six women who were 2 to 4 days postpartum, but were not nursing, were given 500 mg of levodopa orally on one day and 100 mg of levodopa plus 35 mg of carbidopa orally on the next day. Both regimens suppressed basal serum prolactin levels. However, levodopa alone caused an 78% decrease in prolactin while the lower dose combination produced only a 51% decrease. The maximal effect occurred about 2 hours after the dose with both regimens.[7]
Seven women in the first week postpartum who were breastfeeding about 7 times daily were given levodopa 500 mg orally and their serum prolactin responses was studied. The following day, they started carbidopa 50 mg orally every 6 hours for 2 days. On the third day, they received a single dose of carbidopa 50 mg plus levodopa 125 mg orally. Decreases in basal serum prolactin occurred by 30 minutes after the levodopa and after 45 minutes with the combination. Decreases were maximum at 120 minutes after the dose and were 62% with levodopa alone and 48% with the combination, although the difference between the 2 regimens was not statistically significant.[13]
A 37-year-old Israeli woman with Parkinson's disease became pregnant while taking a continuous infusion of levodopa 20 mg/mL and carbidopa 5 mg/mL gel. She breastfed her infant for 3 months while receiving the drug, although the extent of breastfeeding and the dosage of the gel is not clear from the paper.[2]
References
- 1.
- Thulin PC, Woodward WR, Carter JH, et al. Levodopa in human breast milk: Clinical implications. Neurology. 1998;50:1920–1. [PubMed: 9633767]
- 2.
- Zlotnik Y, Giladi N, Hilel A, et al. Levodopa-carbidopa intestinal gel (LCIG) infusion during pregnancy and delivery: First documented case. Parkinsonism Relat Disord. 2014;20:1317–8. [PubMed: 25262534]
- 3.
- Ayalon D, Peyser MR, Toaff R, et al. Effect of L-dopa on galactopoiesis and gonadotropin levels in the inappropriate lactation syndrome. Obstet Gynecol. 1974;44:159–70. [PubMed: 4418555]
- 4.
- Leblanc H, Yen SS. The effect of L-dopa and chlorpromazine on prolactin and growth hormone secretion in normal women. Am J Obstet Gynecol. 1976;126:162–4. [PubMed: 961756]
- 5.
- Board JA, Fierro RJ, Wasserman AJ, et al. Effects of alpha- and beta-adrenergic blocking agents on serum prolactin levels in women with hyperprolactinemia and galactorrhea. Am J Obstet Gynecol. 1977;127:285–7. [PubMed: 556882]
- 6.
- Kaulhausen H, Oney T, Leyendecker G. Inhibition of the renin-aldosterone axis and of prolactin secretion during pregnancy by L-dopa. Br J Obstet Gynaecol. 1982;89:483–8. [PubMed: 7044409]
- 7.
- Rao R, Scommegna A, Frohman LA. Integrity of central dopaminergic system in women with postpartum hyperprolactinemia. Am J Obstet Gynecol. 1982;143:883–7. [PubMed: 7102764]
- 8.
- Malarkey WB, Jacobs LS, Daughaday WH. Levodopa suppression of prolactin in nonpuerperal galactorrhea. N Engl J Med. 1971;285:1160–3. [PubMed: 5107027]
- 9.
- Rapoport B, Refetoff S, Fang VS, et al. Suppression of serum thyrotropin (TSH) by l-dopa in chronic hypothyroidism: Interrelationships in the regulation of TSH and prolactin secretion. J Clin Endocrinol Metab. 1973;36:256–62. [PubMed: 4630270]
- 10.
- Refetoff S, Fang VS, Rapoport B, et al. Interrelationships in the regulation of TSH and prolactin secretion in man: effects of l-dopa, TRH and thyroid hormone in various combinations. J Clin Endocrinol Metab. 1974;38:450–7. [PubMed: 4205563]
- 11.
- Masala A, Alagna S, Devilla L, et al. Muscarinic receptor blockade by pirenzepine: Effect on prolactin secretion in man. J Endocrinol Invest. 1982;5:53–5. [PubMed: 6808052]
- 12.
- Nappi C, Mercorio F, Nappi F, et al. Arch Ostet Ginecol. 1981;86:75–85. [Effect of oral administration of metoclopramide on blood levels of prolactin in the puerperium] [PubMed: 7201788]
- 13.
- Petraglia F, De Leo V, Sardelli S, et al. Prolactin changes after administration of agonist and antagonist dopaminergic drugs in puerperal women. Gynecol Obstet Invest. 1987;23:103–9. [PubMed: 3583091]
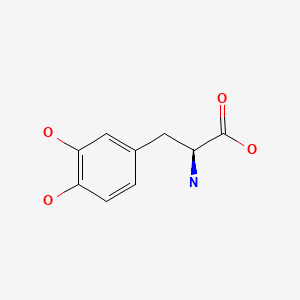
Substance Identification
Substance Name
Levodopa
CAS Registry Number
59-92-7
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Methyldopa.[Drugs and Lactation Database (...]Review Methyldopa.. Drugs and Lactation Database (LactMed®). 2006
- A comparison of the effects of reversible and irreversible inhibitors of aromatic L-amino acid decarboxylase on the half-life and other pharmacokinetic parameters of oral L-3,4-dihydroxyphenylalanine.[Drug Metab Dispos. 1983]A comparison of the effects of reversible and irreversible inhibitors of aromatic L-amino acid decarboxylase on the half-life and other pharmacokinetic parameters of oral L-3,4-dihydroxyphenylalanine.Huebert ND, Palfreyman MG, Haegele KD. Drug Metab Dispos. 1983 May-Jun; 11(3):195-200.
- Review Metaproterenol.[Drugs and Lactation Database (...]Review Metaproterenol.. Drugs and Lactation Database (LactMed®). 2006
- Catechol-O-methyltransferase inhibition protects against 3,4-dihydroxyphenylalanine (DOPA) toxicity in primary mesencephalic cultures: new insights into levodopa toxicity.[Neurochem Int. 2003]Catechol-O-methyltransferase inhibition protects against 3,4-dihydroxyphenylalanine (DOPA) toxicity in primary mesencephalic cultures: new insights into levodopa toxicity.Blessing H, Bareiss M, Zettlmeisl H, Schwarz J, Storch A. Neurochem Int. 2003 Jan; 42(2):139-51.
- Review Dopamine.[Drugs and Lactation Database (...]Review Dopamine.. Drugs and Lactation Database (LactMed®). 2006
- Levodopa - Drugs and Lactation Database (LactMed®)Levodopa - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
