Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 443-48-1
Drug Levels and Effects
Summary of Use during Lactation
With maternal intravenous and oral therapy, breastfed infants receive metronidazole in doses that are less than those used to treat infections in infants, although the active metabolite adds to the total infant exposure. Plasma levels of the drug and metabolite are measurable, but less than maternal plasma levels. Case reports of Candida infections and diarrhea have been reported, and a comparative trial suggested that oral and rectal colonization with Candida might be more common in infants exposed to metronidazole.
Neither topical nor vaginal metronidazole have been studied during breastfeeding. After vaginal administration, plasma levels are less than 2% of those after a 500 mg oral dose. After topical administration, blood levels are about 1% of the peak plasma levels after a 250 mg oral dose. Only water-miscible cream or gel products should be applied to the breast because ointments may expose the infant to high levels of mineral paraffins via licking.[1]
Because of the well demonstrated genotoxicity and mutagenicity in bacteria, carcinogenicity in animals, and possible mutagenicity in humans,[2,3] concern has been raised about exposure of healthy infants to metronidazole via breastmilk. The relevance of these findings has been questioned and no definitive study has yet been performed in humans.
Opinions vary among experts on the advisability of using metronidazole during longer-term therapy while breastfeeding, but some sources recommend discontinuing breastfeeding for 12 to 24 hours after a single dose of 2 grams, but not after lower dosages.[4] Other drugs are available for some conditions that metronidazole is used to treat. Topical or vaginal use of metronidazole during breastfeeding is unlikely to be of concern, although the manufacturer of one vaginal product recommends not breastfeeding during treatment and for 2 days after the last dose.
Drug Levels
Maternal Levels. Ten women were given a single oral dose of metronidazole 200 mg at 5 days postpartum. Milk levels averaged 3.4 mg/L at 4 hours, 2.8 mg/L at 8 hours and 1.3 mg/L at 12 hours (5 women) after the dose.[5]
Seventeen mothers in a randomized study received oral metronidazole 200 mg 3 times daily for 7 days postpartum. Milk metronidazole levels taken at unstated times on day 6 averaged 4.7 mg/L (range 1.1 to 15.2 mg/L).[6]
Three women were given a single 2 gram oral dose of metronidazole for trichomoniasis. Average milk levels were 45.8 mg/L at 2 hours after the dose, 27.9 mg/L at 8 hours after the dose, 19.1 mg/L at 12 hours after the dose, 12.6 mg/L at 18 hours (2 women) and 3.5 mg/L at 36 hours after the dose (2 women). The authors estimated that the infants would receive a total of 25.3 mg over the 48 hours following this dose.[7]
Fifteen women received 200 mg (n = 11) or 400 mg (n = 4) of metronidazole orally 3 times a day for postpartum endometritis 0 to 22 days postpartum. Single milk samples taken after 1 to 9 days of therapy and from 30 minutes to 4 hours after a 200 mg dose contained 1.6 to 12.2 mg/L of metronidazole and 1.1 to 3.8 mg/L of hydroxymetronidazole. Milk samples taken 2 to 3 hours after a 400 mg dose contained 11.6 to 18 mg/L of metronidazole and 2.4 to 6.3 mg/L of hydroxymetronidazole.[8]
Twelve women taking oral metronidazole 400 mg 3 times daily at an average of 4.3 days postpartum had milk samples taken on days 3 and 4 postpartum. Milk levels of metronidazole averaged 15.5 mg/L at 2 hours after the dose, 12.9 mg/L at 4 hours after the dose, 10.6 mg/L at 6 hours after the dose, and 9.1 mg/L at 8 hours after the dose. Milk levels of hydroxymetronidazole averaged 5.5 mg/L at 2 hours after the dose, 5.7 mg/L at 4 hours after the dose, 5.6 mg/L at 6 hours after the dose, and 5.5 mg/L at 8 hours after the dose. The authors estimated that a breastfed neonate ingesting 500 mL of milk daily with this maternal dosage would receive less than 10% of the recommended newborn dosage of metronidazole.[9]
Fifteen women who were 1 month postpartum were given a single intravenous dose of metronidazole 500 mg. The average breastmilk levels at 2 hours after the dose was 7.55 mg/L.[10]
Three postpartum women were treated with intravenous metronidazole 500 mg 3 times daily for 2 days following a cesarean section. The women provided a breastmilk sample 1 to 2 hours after a dose on the second day of therapy. Metronidazole concentrations in milk were 7.3, 9.6 and 10.1 mg/L.[11]
Infant Levels. Ten 5-day-old infants were breastfed every 4 hours after a single 200 mg oral dose of metronidazole was given to their mothers. Two infants had metronidazole serum levels of 0.28 and 0.4 mg/L and 3 had unmeasurable (<0.05 mg/L) levels 8 hours after the dose. Another 2 infants had metronidazole serum levels of 0.2 mg/L and another 3 had unmeasurable (<0.05 mg/L) levels 12 hours after the dose.[5]
Breastfed newborn infants whose mothers were taking oral metronidazole 3 times daily had blood samples taken 1 to 2 hours after a maternal dose. Eleven infants whose mothers were taking a dose of 600 mg daily had plasma metronidazole levels averaging 0.8 mg/L (range 0.3 to 1.4 mg/L) and hydroxymetronidazole levels averaging 0.4 mg/L (range 0.1 to 0.8 mg/L). Four infants whose mothers were taking 1200 mg daily had plasma metronidazole levels averaging 2.4 mg/L (range 0.6 to 4.9 mg/L) and hydroxymetronidazole levels averaging 1.1 mg/L (range 0.4 to 2.3 mg/L). The infants had plasma metronidazole levels ranging from 4 to 32% of maternal plasma levels and plasma hydroxymetronidazole ranging from 8 to 96% of maternal plasma levels.[8]
Seven breastfed infants whose mothers were taking oral metronidazole 400 mg 3 times daily had serum levels measured 4 to 8 hours after a maternal dose and 30 to 90 minutes after breastfeeding. Their average plasma levels were 1.6 mg/L for metronidazole and 1.4 mg/L for hydroxymetronidazole. These levels corresponded to 12.5% and 25.6% of maternal metronidazole and hydroxymetronidazole plasma levels, respectively.[9]
Effects in Breastfed Infants
None of ten 5-day-old infants who were breastfed every 4 hours after a single maternal 200 mg oral dose of metronidazole had any signs of oral or gastrointestinal upset during the 12-hour study period.[5]
Sixteen newborn breastfed infants (aged 0 to 22 days) of mothers receiving 200 mg or 400 mg of oral metronidazole 3 times daily reportedly suffered no observable adverse reactions during the 9 days of the study.[8]
A case of diarrhea and secondary lactose intolerance was possibly caused by metronidazole in breastmilk transmitted to the infant in the early neonatal period.[12]
In a controlled, comparative study, 35 newborn infants were monitored for 10 days during maternal therapy with metronidazole and another antibiotic (33 ampicillin, 1 erythromycin and 1 cephalexin) for postpartum infection or prophylaxis. Dosages and routes of administration were not stated, but some mothers received the drugs intravenously initially and then were switched to oral therapy. Compared to infants of mothers who received ampicillin alone or no antibiotics, more infants exposed to metronidazole and ampicillin had very loose stools than in the other groups, especially when the drugs were given intravenously. More frequent and heavier growth of Candida species was found in the oral and perianal swabs of metronidazole-exposed infants, but this did not quite reach statistical significance (p=0.053). One infant exposed to metronidazole and ampicillin developed oral thrush. No differences were found between the groups in diaper rash, feeding problems or weight gain to the time of discharge.[9]
Effects on Lactation and Breastmilk
Relevant published information was not found as of the revision date.
Alternate Drugs to Consider
(Anaerobic bacterial infections) Amoxicillin and Clavulanic Acid, Clindamycin, Doxycycline; (Giardiasis) Tinidazole; (Topical for Rosacea) Azelaic Acid; (Vaginal) Clindamycin
References
- 1.
- Noti A, Grob K, Biedermann M, et al. Exposure of babies to C(15)-C(45) mineral paraffins from human milk and breast salves. Regul Toxicol Pharmacol 2003;38:317-25. [PubMed: 14623482]
- 2.
- Dobiás L, Cerna M, Rossner P, et al. Genotoxicity and carcinogenicity of metronidazole. Mutat Res 1994;317:177-94. [PubMed: 7515153]
- 3.
- Bendesky A, Menendez D, Ostrosky-Wegman P. Is metronidazole carcinogenic? Mutat Res 2002;511:133-44. [PubMed: 12052431]
- 4.
- Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep 2021;70:1-187. [PMC free article: PMC8344968] [PubMed: 34292926]
- 5.
- Gray MS, Kane PO, Squires S. Further observations on metronidazole (Flagyl). Br J Vener Dis 1961;37:278-9. [PMC free article: PMC1047447] [PubMed: 13901320]
- 6.
- Anon. An evaluation of metronidazole in the prophylaxis of anaerobic infections in obstetrical patients. J Antimicrob Chemother 1978;4:55-62. [PubMed: 357408]
- 7.
- Erickson SH, Oppenheim GL, Smith GH. Metronidazole in breast milk. Obstet Gynecol 1981;57:48-50. [PubMed: 7454176]
- 8.
- Heisterberg L, Branebjerg PE. Blood and milk concentrations of metronidazole in mothers and infants. J Perinat Med 1983;11:114-20. [PubMed: 6854509]
- 9.
- Passmore CM, McElnay JC, Rainey EA, et al. Metronidazole excretion in human milk and its effect on the suckling neonate. Br J Clin Pharmacol 1988;26:45-51. [PMC free article: PMC1386498] [PubMed: 3203060]
- 10.
- Zhang Y, Zhang Q, Xu Z. Tissue and body fluid distribution of antibacterial agents in pregnant and lactating women. Zhonghua Fu Chan Ke Za Zhi 1997;32:288-92. [PubMed: 9596854]
- 11.
- Geballa-Koukoula A, Panderi I, Zervas K, et al. A porous graphitized carbon LC-ESI/MS method for the quantitation of metronidazole and fluconazole in breast milk and human plasma. J Chromatogr B Analyt Technol Biomed Life Sci 2018;1084:175-84. [PubMed: 29604616]
- 12.
- Clements CJ. Metronidazole and breast feeding. N Z Med J 1980;92:329. [PubMed: 6934434]
Substance Identification
Substance Name
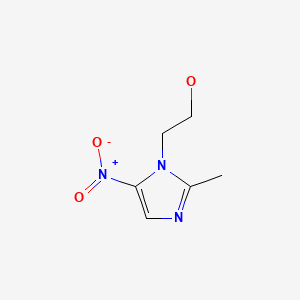
Metronidazole
CAS Registry Number
443-48-1
Drug Class
Breast Feeding
Lactation
Milk, Human
Anti-Infective Agents
Antibacterial Agents
Antiprotozoal Agents
Nitroimidazoles
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Tinidazole.[Drugs and Lactation Database (...]Review Tinidazole.. Drugs and Lactation Database (LactMed®). 2006
- Review Ornidazole.[Drugs and Lactation Database (...]Review Ornidazole.. Drugs and Lactation Database (LactMed®). 2006
- Review Secnidazole.[Drugs and Lactation Database (...]Review Secnidazole.. Drugs and Lactation Database (LactMed®). 2006
- Review Neomycin.[Drugs and Lactation Database (...]Review Neomycin.. Drugs and Lactation Database (LactMed®). 2006
- Review Acitretin.[Drugs and Lactation Database (...]Review Acitretin.. Drugs and Lactation Database (LactMed®). 2006
- Metronidazole - Drugs and Lactation Database (LactMed®)Metronidazole - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
