Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 2078-54-8
Drug Levels and Effects
Summary of Use during Lactation
Amounts of propofol in milk are very small and are not expected to be absorbed by the infant. Although one expert panel recommends withholding nursing for an unspecified time after propofol administration, most recommend that breastfeeding can be resumed as soon as the mother has recovered sufficiently from general anesthesia to nurse and that discarding milk is unnecessary.[1-4] When a combination of anesthetic agents is used for a procedure, follow the recommendations for the most problematic medication used during the procedure. General anesthesia for cesarean section using propofol as a component for induction may delay the onset of lactation. In one study, breastfeeding before general anesthesia induction reduced requirements of propofol and sevoflurane compared to those of nursing mothers whose breastfeeding was withheld or nonnursing women.[5] Case reports have noted blue-green or green discoloration of breastmilk after nursing mothers received propofol.
Drug Levels
Maternal Levels. Five women who had undergone general anesthesia with propofol intravenously shortly after delivery had colostrum propofol levels measured. All of the women received 2 mg/kg intravenously over 20 seconds at time zero followed by a continuous infusion. In 3 women who received 0.25 to 0.37 mg/kg/minute, propofol was detectable in colostrum, but not quantifiable because of technical difficulties. In a woman who received 0.42 mg/kg/minute for 7 minutes, the highest colostrum level was 1.53 mg/L at 15 minutes after the start of the infusion. Colostrum levels decreased to 0.12 mg/L over the next 8 hours. Another woman who received 0.18 mg/kg/minute for 6 hours, the highest colostrum level was 4.91 mg/L at 30 minutes after the start of the infusion.[6]
Four women received a single intravenous bolus dose of propofol 2.5 mg/kg prior to cesarean section. Colostrum levels averaged 0.17 mg/L (range 0.14 to 0.24 mg/L) in 3 of the women 4 hours after the dose and 0.14 mg/L (range 0.089 to 0.19 mg/L) in 4 of the women 8 hours after the dose. In the same report, 3 women received a bolus dose of propofol 2.5 mg/kg followed by a continuous infusion of 5 mg/kg/hour. In one patient, colostrum level was 0.33 mg/L at 4 hours after the bolus; a second patient had levels of 0.74 mg/L at 5 hours and 0.048 mg/L at 8 hours after the bolus; a third patient had a colostrum level of 0.036 mg/L at 6 hours after the bolus.[2]
Five women who were 6 to 15 weeks postpartum were given a single dose of 2.5 mg/kg of propofol intravenously before undergoing general anesthesia. Several milk samples were collected between 5 and 24 hours after the injection from each woman. The authors estimated that the infants would receive an average of 0.0052 mg/kg in the 24 hours after a single dose of propofol. This corresponds to 0.2% of the maternal weight-adjusted dosage. The women's milk output following the surgical procedure was less than half of the normal milk output of nursing mothers. The authors concluded that this amount of propofol in milk is unlikely to affect a healthy, term infant.[3] The infants of mothers not undergoing a surgical procedure might receive a greater dose of propofol in breastmilk, but it would be unlikely to be a large dose.
A woman received 474 mg of propofol by controlled infusion during a procedure to terminate an ectopic pregnancy. The first milk she pumped 8 hours after the procedure was green in color. Although the authors suspect that propofol was the cause of the discoloration, the woman had also received several other medications during the procedure. Thirty hours later, propofol was detected in a milk sample at a concentration of 24 mcg/L, completely as unconjugated propofol.[7]
Two mothers who were breastfeeding their infants were given propofol doses that targeted a serum concentration of 6.5 mcg/L for anesthesia induction. Propofol was stopped as xenon anesthesia was started. One mother received a total of 350 mg of propofol intravenously and had an operative time of 35 minutes. Her milk propofol level was 0.13 mg/L at 300 minutes after extubation. The other mother received a total of 443 mg of propofol intravenously and had an operative time of 35 minutes. Her milk propofol level was 2.78 mg/L at 90 minutes after extubation and 0.84 mg/L 300 minutes after extubation.[8]
Infant Levels. Relevant published information was not found as of the revision date.
Effects in Breastfed Infants
Four mothers who were breastfeeding their infants received propofol as part of their general anesthesia for surgical procedures. All patients also received intravenous remifentanil and rocuronium, and inhaled xenon as part of the anesthesia. They were given doses of propofol that targeted a serum concentration of 6.5 mcg/L for induction and stopped as xenon anesthesia was started. Operation times ranged from 35 to 45 minutes. Individual infants were first breastfed as follows: 1.5 hours, 2.8 hours, 4.6 hours, and 5 hours after extubation. No signs of sedation were observed in any of the infants after their first feeding or at home after discharge.[8]
Effects on Lactation and Breastmilk
Five women who were 6 to 15 weeks postpartum were given single doses of 2 mg of midazolam and 2.5 mg/kg of propofol intravenously before undergoing general anesthesia. The women's milk output following the surgical procedure was less than half of the normal milk output of nursing mothers. The authors speculated that milk volume might be reduced postoperatively because of perioperative fluid restriction and volume losses, as well as stress-induced inhibition of milk production.[3]
A woman underwent emergency laparoscopic surgery using propofol as well as fentanyl, remifentanil, mivacurium, and dipyrone during the surgery and metamizole, piritramide, dipyrone, butylscopolamine, and metoclopramide postoperatively. Eight hours postoperatively, her milk turned bluish green, then green. Both propofol and metoclopramide have caused green urine. Thirty hours after the milk color change, propofol but not metoclopramide, was detected in milk.[7]
A randomized study compared the effects of cesarean section using general anesthesia, spinal anesthesia, or epidural anesthesia, to normal vaginal delivery on serum prolactin and oxytocin as well as time to initiation of lactation. General anesthesia was performed using propofol 2 mg/kg and rocuronium 0.6 mg/kg for induction, followed by sevoflurane and rocuronium 0.15 mg/kg as needed. Fentanyl 1 to 1.5 mcg/kg was administered after delivery. Patients in the general anesthesia group (n = 21) had higher post-procedure prolactin levels and a longer mean time to lactation initiation (25 hours) than in the other groups (10.8 to 11.8 hours). Postpartum oxytocin levels in the nonmedicated vaginal delivery group were higher than in the general and spinal anesthesia groups.[9]
A randomized, double-blind study compared the effects of intravenous propofol 0.25 mg/kg, ketamine 0.25 mg/kg, ketamine 25 mg plus propofol 25 mg, and saline placebo for pain control in mothers post-cesarean section in mothers post-cesarean section. A single dose was given immediately after clamping of the umbilical cord. The time to the first breastfeeding was 58 minutes in those who received placebo, 42.6 minutes with propofol and 25.8 minutes with propofol plus ketamine. The time was significantly shorter than the other groups with the combination.[10]
A retrospective study of women in a Turkish hospital who underwent elective cesarean section deliveries compared women who received bupivacaine spinal anesthesia (n = 170) to women who received general anesthesia (n = 78) with propofol for induction, sevoflurane for maintenance and fentanyl after delivery. No differences in breastfeeding rates were seen between the groups at 1 hour and 24 hours postpartum. However, at 6 months postpartum, 67% of women in the general anesthesia group were still breastfeeding compared to 81% in the spinal anesthesia group, which was a statistically significant difference.[11]]
A woman nursing an 8-month-old infant 6 to 8 times daily was admitted to the hospital for an appendectomy. During the procedure she received cefazolin, granisetron, ketorolac, rocuronium, succinylcholine, and sufentanil. The patient also received 2 boluses of intravenous propofol of 150 mg followed shortly thereafter by a 50 mg dose. Postoperatively, she was receiving acetaminophen, cefazolin, ibuprofen, and pantoprazole, as well as oxycodone and dimenhydrinate as needed. Twenty-two hours after the procedure, the mother extracted milk for the first time and noted it to be light green in color. Analysis of the green milk using a nonvalidated assay detected no propofol. The green color faded and was absent by postoperative day 4 when she resumed breastfeeding. The authors judged that the green color was possibly caused by propofol or one of its metabolites.[12]
A pregnant woman had an emergency cesarean section delivery in her 24th week of gestation. During the procedure she received 200 mg of propofol as well as cefazolin and acetaminophen after delivery. The first milk expressed by the mother at 12 hours after the procedure was dark green. At 30 hours after the procedure is was light green and returned to a normal color by hour 48.[13]
Alternate Drugs to Consider
Dexmedetomidine, Etomidate, Methohexital, Midazolam, Thiopental
References
- 1.
- Vargo JJ, Delegge MH, Feld AD, et al. Multisociety sedation curriculum for gastrointestinal endoscopy. Gastroenterology. 2012;143:e18–41. [PubMed: 22624720]
- 2.
- Dailland P, Cockshott ID, Didier Lirzin J, et al. Intravenous propofol during cesarean section: placental transfer, concentrations in breast milk, and neonatal effects. A preliminary study. Anesthesiology. 1989;71:827–34. [PubMed: 2589672]
- 3.
- Nitsun M, Szokol JW, Saleh HJ, et al. Pharmacokinetics of midazolam, propofol, and fentanyl transfer to human breast milk. Clin Pharmacol Ther. 2006;79:549–57. [PubMed: 16765143]
- 4.
- Shergill AK, Ben-Menachem T, Chandrasekhara V, et al. Guidelines for endoscopy in pregnant and lactating women. Gastrointest Endosc. 2012;76:18–24. [PubMed: 22579258]
- 5.
- Bhaskara B, Dayananda VP, Kannan S, et al. Effect of breastfeeding on haemodynamics and consumption of propofol and sevoflurane: A state entropy guided comparative study. Indian J Anaesth. 2016;60:180–6. [PMC free article: PMC4800934] [PubMed: 27053781]
- 6.
- Schmitt JP, Schwoerer D, Diemunsch P, et al. Ann Fr Anesth Reanim. 1987;6:267–8. [Passage of propofol in the colostrum. Preliminary data] [PubMed: 3498397]
- 7.
- Birkholz T, Eckardt G, Renner S, et al. Green breast milk after propofol administration. Anesthesiology. 2009;111:1168–9. [PubMed: 19858894]
- 8.
- Stuttmann R, Schafer C, Hilbert P, et al. The breast feeding mother and xenon anaesthesia: Four case reports. Breast feeding and xenon anaesthesia. BMC Anesthesiol. 2010;10:1. [PMC free article: PMC2837001] [PubMed: 20167123]
- 9.
- Kutlucan L, Seker IS, Demiraran Y, et al. Effects of different anesthesia protocols on lactation in the postpartum period. J Turk Ger Gynecol Assoc. 2014;15:233–8. [PMC free article: PMC4285212] [PubMed: 25584032]
- 10.
- Jaafarpour M, Vasigh A, Khajavikhan J, et al. Effect of ketofol on pain and complication after Caesarean delivery under spinal anaesthesia: A randomized double-blind clinical trial. J Clin Diagn Res. 2017;11:UC04–UC7. [PMC free article: PMC5427408] [PubMed: 28511482]
- 11.
- Karasu D, Yilmaz C, Ozgunay SE, et al. A comparison of the effects of general anaesthesia and spinal anaesthesia on breastfeeding. C R Acad Bulg Sci. 2018;71:993–1000. [CrossRef]
- 12.
- Rainone A, Delucilla L, Elofer S, et al. Propofol-induced green breast milk: A case report. Can J Hosp Pharm. 2018;71:389–91. [PMC free article: PMC6306180] [PubMed: 30626986]
- 13.
- Bulut O, Ovali F. Green breast milk: A rare side effect of propofol. J Paediatr Child Health. 2020;57:153–4. [PubMed: 32898931]
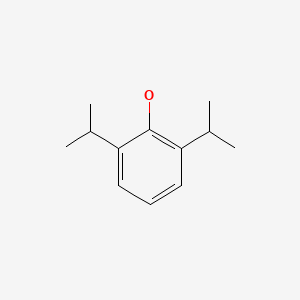
Substance Identification
Substance Name
Propofol
CAS Registry Number
2078-54-8
Drug Class
Breast Feeding
Lactation
Anesthetics, Intravenous
Hypnotics and Sedatives
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Fospropofol.[Drugs and Lactation Database (...]Review Fospropofol.. Drugs and Lactation Database (LactMed®). 2006
- Review Sevoflurane.[Drugs and Lactation Database (...]Review Sevoflurane.. Drugs and Lactation Database (LactMed®). 2006
- Review Isoflurane.[Drugs and Lactation Database (...]Review Isoflurane.. Drugs and Lactation Database (LactMed®). 2006
- Review Enflurane.[Drugs and Lactation Database (...]Review Enflurane.. Drugs and Lactation Database (LactMed®). 2006
- Review Desflurane.[Drugs and Lactation Database (...]Review Desflurane.. Drugs and Lactation Database (LactMed®). 2006
- Propofol - Drugs and Lactation Database (LactMed®)Propofol - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
