Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
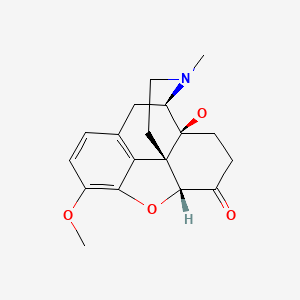
CASRN: 76-42-6
Drug Levels and Effects
Summary of Use during Lactation
Maternal use of oral opioids during breastfeeding can cause infant drowsiness, which may progress to rare but severe central nervous system depression. Sedation in breastfed infants has occurred after maternal use of oxycodone. Newborn infants seem to be particularly sensitive to the effects of even small dosages of narcotic analgesics. Daily doses of less than 60 mg of the immediate-release formulation are unlikely to result in clinically relevant exposures in breastfed infants. Extended-release oxycodone products (such as OxyContin) are not recommended in nursing mothers. If oxycodone is required by the mother of a newborn, it is not a reason to discontinue breastfeeding; however, once the mother's milk comes in, it is best to provide pain control with a nonnarcotic analgesic and limit maternal intake of oral oxycodone (and combinations) to a 2 to 3 days, especially in the outpatient setting.[1]
An institution using this strategy following a cesarean section found that mothers used 75% fewer oxycodone tablets.[2] A maximum oxycodone dosage of 30 mg daily is suggested, although some sources recommend avoiding oxycodone altogether during breastfeeding.[3,4] A 30 mg daily limit appears to offer the same benefits to the mother as higher dosages for mothers after cesarean section.[5] Oxycodone elimination is decreased in young infants with much inter-individual variability. Monitor the infant closely for drowsiness, adequate weight gain, and developmental milestones, especially in younger, exclusively breastfed infants. If the baby shows signs of increased sleepiness (more than usual), difficulty breastfeeding, breathing difficulties, or limpness, a physician should be contacted immediately. Other agents are preferred over oxycodone during breastfeeding.[3]
Drug Levels
Oxycodone is metabolized to the active metabolites, noroxycodone and oxymorphone. Oxycodone has an oral bioavailability of 60% to 87% in adults. Oxycodone elimination is decreased in young infants and much inter-individual variability exists.
Maternal Levels. Six breastfeeding mothers who were using 1 to 2 capsules containing a combination of 5 mg oxycodone and 500 mg acetaminophen every 4 to 7 hours for post-cesarean section pain had their milk sampled several times after successive doses. Peak oxycodone milk levels reportedly occurred 1 to 2 hours after the first dose and then at variable times after successive doses. The number of hours after a mother's last dose when oxycodone could still be measured in milk was depended on the number of doses taken. Oxycodone could be measured in milk up to 4, 12, and 36 hours after 4, 9, and 11 doses, respectively. In all the mothers, measured oxycodone milk levels ranged from undetectable (<5 mcg/L) to 229 mcg/L. The authors estimated that an exclusively breastfed infant would receive a maximum 8% of the maternal weight-adjusted dosage of oxycodone, but active metabolite levels were not measured.[6]
Fifty mothers who delivered by cesarean section and received oxycodone had milk (colostrum) and serum samples measured for oxycodone at 24, 48 and 72 hours postpartum without respect to the time of the previous oxycodone dose. The most common doses received by the mothers during the previous 24 hours (including one 30 mg dose rectally immediately postoperatively in some cases) were 60 mg (range 30 to 90 mg), 40 mg (range 0 to 90 mg), and 20 mg (range 0 to 50 mg), respectively. Mean colostrum concentrations at the 3 collection times were 58 mcg/L (range 7 to 130 mcg/L), 49 mcg/L (range 0 to 168 mcg/L), and 35 mcg/L (range 0 to 31 mcg/L), respectively. Little correlation was found between maternal dosage and colostrum concentration although colostrum levels correlated well with maternal serum levels, with colostrum concentrations 3.2 to 3.4 higher than serum. Ten mothers had colostrum oxycodone concentrations over 100 mcg/L and 5 had detectable oxycodone in milk 37 hours after the last dose.[7]
Forty-three women who had given birth via cesarean section were given oxycodone 10 mg every 12 hours either as controlled-release tablets either with naloxone 5 mg (Targiniq) or without naloxone (Oxycontin). In addition, women as needed oxycodone 5 or 10 mg subcutaneously, sublingually or PO, or 3 mg intravenously during the study period. In addition, participants received 25 to 50 mg of dexketoprofen three times a day and 1000 mg of acetaminophen four times a day, the first doses intravenously and subsequent doses orally. Milk samples were obtained before the first dose on the evening of the procedure and each morning until postoperative day (POD) 3, although 11 of the women were unable to produce any samples. The concentrations of oxycodone and noroxycodone were analyzed in milk. The median total oxycodone consumption from operation day to POD3 was 83 mg (range 35 to 171 mg) in the oxycodone-naloxone group and 77 mg (range 30 to153 mg) in the oxycodone group. Mothers also received median doses of 19.5 to 20 mg of rescue oxycodone on the day of the operation, 5 to 7.5 mg on POD 1, and none on PODs 2 and 3, although some women did receive doses up to 30 mg on POD 2 and 5 mg on POD 3. Oxymorphone and noroxymorphone were not measured in milk, but were measured in maternal plasma. Noroxycodone and noroxymorphone levels were found in higher concentrations in maternal plasma and noroxycodone levels were higher in milk than oxycodone. Simulations of infant doses of oxycodone intake indicated that with the maximum oxycodone milk concentration and a large milk intake, that an RID of 9% could be reached, but with typical milk intake, RID would be <1% However, the simulations did not take into account noroxycodone, oxymorphone or noroxymorphone, so firm conclusions are hard to reach.[8]
A study of 76 mothers taking a median oxycodone dosage of 33.0 mg daily (range 5.4 to 59.3 mg daily) measured oxycodone, noroxycodone, and oxymorphone in 101 breastmilk samples taken at 3-hour intervals after a dose. The highest average oxycodone milk concentrations was 10.6 mcg/L at 0 to 3 hours after a 5 mg dose and 19.5 mcg/L at 0 to 3 hours after a 10 mg dose. The highest average oxymorphone milk concentrations were 27.9 mcg/L at 3 to 6 hours after a 5 mg dose and 60.5 mcg/L after a 10 mg dose of oxycodone. The highest average noroxycodone milk concentration was 39.1 mcg/L at 3 to 6 hours after a 5 or 10 mg dose of oxycodone. Using the average concentrations of oxycodone, noroxycodone and oxymorphone in milk and assuming equal potency, the infant would receive an estimated 2.8% of an infant dosage of oxycodone in 24 hours with the median 33 mg daily maternal dosage.[9]
Infant Levels. In a study of 50 mothers taking oxycodone post-cesarean section, 45 blood samples were taken from 41 breastfed infants at 24, 48 or 72 hours postpartum. Only 1 of the samples had a detectable (>2 mcg/L) oxycodone level of 7.4 mcg/L. Because these infants were in the first 3 days postpartum, their dosage was probably limited by the small volumes of colostrum they were ingesting.[7]
A woman who was exclusively breastfeeding her infant was taking 5 to 10 mg of oxycodone every 4 to 6 hours for episiotomy pain. Her 45-day-old infant's urine drug screen showed a concentration of >2000 mcg/L (positive cutoff for opioid metabolites was 5 mcg/L).[10]
A study of 76 mothers taking a median oxycodone dose of 33.0 mg daily (range 5.4 to 59.3 mg daily) measured oxycodone, noroxycodone, and oxymorphone in the plasma of 25 of their breastfed infants. At 3 to 6 hours after breastfeeding, the plasma concentration of oxycodone was 0.2 to 0.4 mcg/L in 6 infants and noroxycodone concentrations was 0.2 to 0.3 mcg/L in 10 infants. The other infants had no quantifiable amounts (<0.1 mcg/L) of the drugs. Oxymorphone was undetectable (<0.1 mcg/L) in all infant plasma samples at any time period. Because these infants were in the first 3 days postpartum, their dosage was probably limited by the small volumes of colostrum they were ingesting.[9]
Effects in Breastfed Infants
A 10-month-old, 7.7 kg infant of a prescription drug-dependent mother died of cardiac arrest after a 12- to 24-hour period of lethargy, hypersomnolence and dyspnea. The infant also had a recent history of fever. The mother had reportedly been breastfeeding the infant 3 times a day for several weeks and had taken 180 mg of oxycodone, as well as muscle relaxants, the day prior to her infant's death. A blood oxycodone level of 600 mcg/L was measured on autopsy. The medical examiner considered it unlikely that such a high level of oxycodone in the infant's blood could be due to breastfeeding exposure as reported by the mother and thus considered the death a homicide resulting from either the intentional administration of oxycodone directly to the infant or from a higher dose of oxycodone in breastmilk than that reported by the mother.[11]
In a study of 50 mothers taking oxycodone post-cesarean section, 50 neonates were evaluated for sedation over 48 hours after birth. None was severely sedated and less than 4% had sedation of 3 on a 1 (fully alert) to 5 (difficult to rouse) scale and none more sedated than 3 on the scale. Because these infants were in the first 3 days postpartum, their oxycodone dose was probably limited by the small volumes of colostrum they were ingesting.[7]
An infant was born to a mother taking oxycodone 20 mg 3 times daily, fluoxetine 40 mg daily and quetiapine 400 mg daily. The infant was breastfed 6 to 7 times daily and was receiving 120 mcg of oral morphine 3 times daily for opiate withdrawal. Upon examination at 3 months of age, the infant's weight was at the 25th percentile for age, having been at the 50th percentile at birth. The authors attributed the weight loss to opiate withdrawal. The infant's Denver developmental score was equal to his chronological age.[12]
A woman who was exclusively breastfeeding her infant was taking 5 to 10 mg of oxycodone every 4 to 6 hours for episiotomy pain. Her 45-day-old infant was brought to the emergency department with a temperature of 98.4 degrees F, a heart rate of 154 per minute, 20 breaths per minute, a blood pressure of 71/52, and an oxygen saturation of 60% to 69% on room air. The infant had been constipated since birth, passing one stool every 5 to 8 days. The infant had sluggish movements slow, shallow, and irregular breathing. Her pupils were small, but reactive. Hydromorphone levels in urine were elevated. The patient was intubated and given opiates around the clock for two days before being extubated and discharged. The infant's constipation, CNS and respiratory depression were probably caused by oxycodone in breastmilk.[10]
In a retrospective study, nursing mothers who were taking either oxycodone, codeine or acetaminophen for pain while breastfeeding were contacted by telephone to ascertain the degree of maternally perceived central nervous system (CNS) depression. Mothers taking oxycodone reported signs of CNS depression in 20% (28/139) of their infants, while those taking acetaminophen reported infant CNS depression in only 0.5% (1/184) of their infants. Women who reported infant sedation were taking 0.4 mg/kg daily of oxycodone, and unaffected were taking 0.15 mg/kg daily. Affected infants had more hours of daily uninterrupted sleep than unaffected infants, and 4 of the affected infants reportedly had "irregular breathing". Thirty-eight of 39 mothers reported that infant sedation ceased with maternal oxycodone discontinuation. Mothers of affected infants were also more likely to experience lethargy and other side effects than mothers of unaffected infants. Mothers who took codeine reported a similar rate of infant sedation (17%) compared to oxycodone, but the groups were statistically different in parity and postmenstrual age (PMA), with the codeine group having a slightly higher PMA.[13]
A newborn infant was exclusively breastfed and found to be well by his physician at 2 days of age. At 3 days postpartum, the infant began to be sedated and became difficult to arouse and did not feed from either breast. At 4 days of age, the infant was brought to the emergency department where the infant was found to have lethargy, hypothermia, pinpoint pupils, and a poor sucking reflex. The mother reported that her milk had come in the previous evening. She had taken 10 mg of oxycodone that evening and another 5 mg the next morning in the form of Percocet (oxycodone 5 mg plus acetaminophen 325 mg). The infant was given naloxone 0.34 mg intramuscularly and within 2 minutes, the baby's eyes opened and he drank 45 mL of formula. No further sedation was seen over the next 24 hours.[14] The infant's sedation was probably caused by oxycodone in breastmilk.
A search was performed of the shared database of all U.S. poison control centers for the time period of 2001 to 2017 for calls regarding medications and breastfeeding. Of 2319 calls in which an infant was exposed to a substance via breastmilk, 7 were classified as resulting in a major adverse effect, and 3 of these involved oxycodone. A 16-day-old infant was exposed to cyclobenzaprine, acetaminophen and oxycodone in breastmilk. The infant was admitted to the hospital in a noncritical care unit for bradycardia, hypotension, and respiratory arrest. A 14-day-old infant was exposed to acetaminophen and oxycodone and developed cyanosis. The infant was treated and released. A one-month-old infant was exposed to fentanyl, morphine, oxycodone, and benzodiazepines. The infant was admitted to the intensive care unit and described as being agitated and irritable and having tachycardia, confusion, drowsiness, lethargy, miosis, respiratory depression, acidosis, and hyperglycemia. The dosages and extent of breastfeeding were not reported in any of the cases and the infants all survived.[15]
A cross-sectional survey of mothers who had breastfed their infant in the past 12 months identified 142 mothers who had taken one or more medications while nursing. One of the mothers who was taking a combination product with oxycodone and naloxone reported that her infant developed drowsiness or sleepiness, which caused her to stop the drug.[16]
In population study in the province of Ontario, Canada, 85,852 who filled an opioid prescription within seven days of discharge after delivery were matched to 538,815 did not. Compared with infants born to mothers who were not prescribed an opioid, those born to mothers prescribed an opioid were no more likely to be admitted to hospital in the 30 days after the index date. Infants born to mothers prescribed opioids after delivery were slightly more likely to be taken to the emergency department in the subsequent 30 days (hazard ratio 1.04). Forty-two percent of the mothers prescribed an opioid were prescribed oxycodone. No infant deaths occurred. Of note is that the median drug supply was for 3 days (IQR 2-4).[17]
A study of 76 mothers were taking a median oxycodone dosage of 33.0 mg daily (range 5.4 to 59.3 mg daily). Mild to moderate respiratory depression was observed in 10 infants and mild hypotension was observed in 3 infants. None of these events were attributed to oxycodone by the investigators. The risk of adverse events was probably minimized by the small amount of colostrum being ingested by the 1 to 3 day-old infants.[9]
Effects on Lactation and Breastmilk
Oxycodone can increase serum prolactin.[18] However, the prolactin level in a mother with established lactation may not affect her ability to breastfeed.
Alternate Drugs to Consider
Acetaminophen, Butorphanol, Hydromorphone, Ibuprofen, Morphine
References
- 1.
- Ito S. Opioids in breast milk: Pharmacokinetic principles and clinical implications. J Clin Pharmacol 2018;58 (Suppl 10):S151-S163. [PubMed: 30248201]
- 2.
- Peahl AF, Hallway A, Kenney B, et al. Pain and recovery following cesarean delivery in patients receiving an opioid-sparing pain regimen. AJOG Global Reports 2023;3:100248. [PMC free article: PMC10461237] [PubMed: 37645651]
- 3.
- Sachs, HC, The Committee on Drugs. The transfer of drugs and therapeutics into human breast milk: An update on selected topics.[Reaffirmed May, 2018]. Pediatrics 2013;132:e796-809 [PubMed: 23979084]
- 4.
- Lamvu G, Feranec J, Blanton E. Perioperative pain management: An update for obstetrician-gynecologists. Am J Obstet Gynecol 2018;218:193-9. [PubMed: 28666699]
- 5.
- McKenzie C, Straube L, Webster C, et al. A quality improvement effort to reduce inpatient opioid consumption following cesarean delivery. Am J Perinatol 2024;41:e406-e411. [PubMed: 35750319]
- 6.
- Marx CM, Pucino F, Carlson JD, et al. Oxycodone excretion in human milk in the puerperium. Drug Intell Clin Pharm 1986;20:474.
- 7.
- Seaton S, Reeves M, McLean S. Oxycodone as a component of multimodal analgesia for lactating mothers after Caesarean section: Relationships between maternal plasma, breast milk and neonatal plasma levels. Aust N Z J Obstet Gynaecol 2007;47:181-5. [PubMed: 17550483]
- 8.
- Pesonen A, Hakomäki H, Kokki H, et al. Breast milk oxycodone concentrations in mothers given oxycodone for post-Caesarean delivery pain management. Br J Clin Pharmacol 2024;90:1183-92. [PubMed: 38308454]
- 9.
- 10.
- Sulton-Villavasso C, Austin CA, Patra KP, et al. Index of suspicion. Case 1: Infant who has respiratory distress. Case 2: Abnormal behavior, seizures, and altered sensorium in a 7-year-old boy. Case 3: Fever and dysphagia in a 4-year-old girl. Pediatr Rev 2012;33:279-84. [PubMed: 22659261]
- 11.
- Levine B, Moore KA, Aronica-Pollak P, et al. Oxycodone intoxication in an infant: Accidental or intentional exposure? J Forensic Sci 2004;49:1358-60. [PubMed: 15568714]
- 12.
- Rampono J, Kristensen JH, Ilett KF, et al. Quetiapine and breast feeding. Ann Pharmacother 2007;41:711-4. [PubMed: 17374621]
- 13.
- Lam J, Kelly L, Ciszkowski C, et al. Central nervous system depression of neonates breastfed by mothers receiving oxycodone for postpartum analgesia. J Pediatr 2012;160:33-7. [PubMed: 21880331]
- 14.
- Timm NL. Maternal use of oxycodone resulting in opioid intoxication in her breastfed neonate. J Pediatr 2013;162:421-2. [PubMed: 23063265]
- 15.
- Beauchamp GA, Hendrickson RG, Horowitz BZ, et al. Exposures through breast milk: An analysis of exposure and information calls to U.S. poison centers, 2001-2017. Breastfeed Med 2019;14:508-12. [PubMed: 31211594]
- 16.
- Ahmadzai H, Tee LBG, Crowe A. Adverse drug reactions in breastfed infants: A cross-sectional study of lactating mothers. Breastfeed Med 2022;17:1011-17. [PubMed: 36315169]
- 17.
- Zipursky JS, Gomes T, Everett K, et al. Maternal opioid treatment after delivery and risk of adverse infant outcomes: Population based cohort study. Bmj 2023;380:e074005. [PMC free article: PMC10015218] [PubMed: 36921977]
- 18.
- Saarialho-Kere U, Mattila MJ, Seppala T. Psychomotor, respiratory and neuroendocrinological effects of a mu-opioid receptor agonist (oxycodone) in healthy volunteers. Pharmacol Toxicol 1989;65:252-7. [PubMed: 2555803]
Substance Identification
Substance Name
Oxycodone
CAS Registry Number
76-42-6
Drug Class
Breast Feeding
Lactation
Milk, Human
Analgesics, Opioid
Narcotics
Antitussive Agents
Opiates
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Dihydrocodeine.[Drugs and Lactation Database (...]Review Dihydrocodeine.. Drugs and Lactation Database (LactMed®). 2006
- Review Hydrocodone.[Drugs and Lactation Database (...]Review Hydrocodone.. Drugs and Lactation Database (LactMed®). 2006
- Review Nalbuphine.[Drugs and Lactation Database (...]Review Nalbuphine.. Drugs and Lactation Database (LactMed®). 2006
- Review Oxymorphone.[Drugs and Lactation Database (...]Review Oxymorphone.. Drugs and Lactation Database (LactMed®). 2006
- Review Morphine.[Drugs and Lactation Database (...]Review Morphine.. Drugs and Lactation Database (LactMed®). 2006
- Oxycodone - Drugs and Lactation Database (LactMed®)Oxycodone - Drugs and Lactation Database (LactMed®)
- LOC108302947 [Cebus imitator]LOC108302947 [Cebus imitator]Gene ID:108302947Gene
- Lindernia viscosa (8)Nucleotide
- zinc finger CCCH domain-containing protein 34 isoform X1 [Quercus suber]zinc finger CCCH domain-containing protein 34 isoform X1 [Quercus suber]gi|1344086880|ref|XP_023927549.1|Protein
- PREDICTED: Hibiscus syriacus WAT1-related protein At2g37460-like (LOC120198311),...PREDICTED: Hibiscus syriacus WAT1-related protein At2g37460-like (LOC120198311), transcript variant X1, mRNAgi|1965348858|ref|XM_039199647.1|Nucleotide
Your browsing activity is empty.
Activity recording is turned off.
See more...
