CASRN: 114-07-8
Drug Levels and Effects
Summary of Use during Lactation
Because of the low levels of erythromycin in breastmilk and safe administration directly to infants, it is acceptable in nursing mothers. The small amounts in milk are unlikely to cause adverse effects in the infant. Monitor the infant for irritability and possible effects on the gastrointestinal flora, such as diarrhea, candidiasis (thrush, diaper rash). One case report and unconfirmed epidemiologic evidence indicates that hypertrophic pyloric stenosis in infants might occur with maternal use of erythromycin during the first two weeks of breastfeeding; however, if it occurs, the frequency is very low and others have questioned this relationship.
Infant side effects are unlikely with topical application for acne, although topical application to the nipple may increase the risk of diarrhea in the infant. Only water-miscible cream or gel products should be applied to the breast because ointments may expose the infant to high levels of mineral paraffins via licking.[1]
Drug Levels
Maternal Levels. Two women were given a single dose of 500 mg erythromycin (salt unspecified) orally, and milk levels were measured at 2 and 6 hours after the dose. Average erythromycin milk levels at 2, 4, and 6 hours after the dose were 1, 1.2 and 1.1 mg/L, respectively.[2]
Fifteen women who were 1 month postpartum were given a single 500 mg dose of erythromycin intravenously. Mean breastmilk levels 2 hours after the dose were 2.5 mg/L.[3]
Infant Levels. Relevant published information was not found as of the revision date.
Effects in Breastfed Infants
Pyloric stenosis, vomiting, sedation, poor sucking and poor weight gain probably related to erythromycin in breastmilk was reported in a 3-week-old infant.[4]
A cohort study of infants diagnosed with infantile hypertrophic pyloric stenosis found that affected infants were 2.3 to 3 times more likely to have a mother taking a macrolide antibiotic during the 90 days after delivery. Stratification of the infants found the odds ratio to be 10 for female infants and 2 for male infants. All of the mothers of affected infants nursed their infants. Seventy-two percent of the macrolide prescriptions were for erythromycin. However, the authors did not state which macrolide was taken by the mothers of the affected infants.[5]
A study comparing the breastfed infants of mothers taking amoxicillin to those taking a macrolide antibiotic found no instances of pyloric stenosis. However, most of the infants exposed to a macrolide in breastmilk were exposed to roxithromycin. Only 2 of the 55 infants exposed to a macrolide were exposed to erythromycin. Adverse reactions occurred in 12.7% of the infants exposed to macrolides which was similar to the rate in amoxicillin-exposed infants. Reactions included rash, diarrhea, loss of appetite, and somnolence.[6]
A retrospective database study in Denmark of 15 years of data found a 3.5-fold increased risk of infantile hypertrophic pyloric stenosis in the infants of mothers who took a macrolide during the first 13 days postpartum, but not with later exposure. The proportion of infants who were breastfed was not known, but probably high. The proportion of women who took each macrolide was also not reported.[7]
In one telephone follow-up study, mothers reported diarrhea 2 infants and irritability in 2 infants out of 17 infants whose mothers were taking erythromycin during breastfeeding. None of the reactions required medical attention.[8]
Two meta-analyses failed to demonstrate a relationship between maternal macrolide use during breastfeeding and infantile hypertrophic pyloric stenosis.[9][10]
Effects on Lactation and Breastmilk
Relevant published information was not found as of the revision date.
Alternate Drugs to Consider
(Systemic Infections) Azithromycin, Clarithromycin; (Topical for Acne) Azelaic Acid, Benzoyl Peroxide, Clindamycin, Tretinoin
References
- 1.
- Noti A, Grob K, Biedermann M. Exposure of babies to C(15)-C(45) mineral paraffins from human milk and breast salves. Regul Toxicol Pharmacol. 2003;38:317-25. [PubMed: 14623482]
- 2.
- Matsuda S. Transfer of antibiotics into maternal milk. Biol Res Pregnancy Perinatol. 1984;5:57-60. [PubMed: 6743732]
- 3.
- Zhang Y, Zhang Q, Xu Z. [Tissue and body fluid distribution of antibacterial agents in pregnant and lactating women]. Zhonghua Fu Chan Ke Za Zhi. 1997;32:288-92. [PubMed: 9596854]
- 4.
- Stang H. Pyloric stenosis associated with erythromycin ingested through breast milk. Minn Med. 1986;69:669-70, 82. [PubMed: 3796569]
- 5.
- Sorensen HT, Skriver MV, Pedersen L et al. Risk of infantile hypertrophic pyloric stenosis after maternal postnatal use of macrolides. Scand J Infect Dis. 2003;35:104-6. [PubMed: 12693559]
- 6.
- Ito S, Blajchman A, Stephenson M et al. Prospective follow-up of adverse reactions in breast-fed infants exposed to maternal medication. Am J Obstet Gynecol. 1993;168:1393-9. [PubMed: 8498418]
- 7.
- Goldstein LH, Berlin M, Tsur L et al. The safety of macrolides during lactation. Breastfeed Med. 2009;4:197-200. [PubMed: 19366316]
- 8.
- Lund M, Pasternak B, Davidsen RB et al. Use of macrolides in mother and child and risk of infantile hypertrophic pyloric stenosis: Nationwide cohort study. BMJ. 2014;348:g1908. [PMC free article: PMC3949411] [PubMed: 24618148]
- 9.
- Abdellatif M, Ghozy S, Kamel MG et al. Association between exposure to macrolides and the development of infantile hypertrophic pyloric stenosis: a systematic review and meta-analysis. Eur J Pediatr. 2019;178:301-14. [PubMed: 30470884]
- 10.
- Almaramhy HH, Al-Zalabani AH. The association of prenatal and postnatal macrolide exposure with subsequent development of infantile hypertrophic pyloric stenosis: A systematic review and meta-analysis. Ital J Pediatr. 2019;45:20. [PMC free article: PMC6360705] [PubMed: 30717812]
Substance Identification
Substance Name
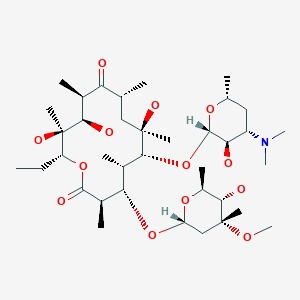
Erythromycin
CAS Registry Number
114-07-8
Drug Class
- Breast Feeding
- Lactation
- Anti-Infective Agents
- Antibacterial Agents
- Dermatologic Agents
- Macrolides
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
Publication Details
Publication History
Last Revision: April 1, 2019.
Copyright
Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
Publisher
National Institute of Child Health and Human Development, Bethesda (MD)
NLM Citation
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-. Erythromycin. [Updated 2019 Apr 1].