Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 54739-18-3
Drug Levels and Effects
Summary of Use during Lactation
Limited information indicates that maternal fluvoxamine doses of up to 300 mg daily produce low levels in breastmilk and would not be expected to cause any adverse effects in breastfed infants, especially if the infant is older than 2 months. If fluvoxamine is required by the mother, it is not a reason to discontinue breastfeeding. A safety scoring system finds fluvoxamine use to be possible during breastfeeding.[1] One infant was reported to have an elevated serum level of fluvoxamine, but most who have been tested have undetectable serum levels. Another infant developed diarrhea, vomiting and stimulation after maternal initiation of fluvoxamine. A limited amount of long-term follow-up on growth and development has found no adverse effects in breastfed infants. Monitor infants exposed to fluvoxamine through breast milk for diarrhea, vomiting, decreased sleep, and agitation.
Mothers taking an SSRI during pregnancy and postpartum may have more difficulty breastfeeding, although this might be a reflection of their disease state.[2] These mothers may need additional breastfeeding support. Breastfed infants exposed to an SSRI during the third trimester of pregnancy have a lower risk of poor neonatal adaptation than formula-fed infants.
Drug Levels
Maternal Levels. In a pooled analysis of serum levels from published studies and 1 unpublished case, the authors found that 6 mothers taking an average daily dosage of 159 mg (range 50 to 300 mg) had an average milk fluvoxamine level of 174 mcg/L (range 18 to 478 mcg/L).[3] Using the average dosage and milk level data from this paper, an exclusively breastfed infant would receive an estimated 0.98% of the maternal weight-adjusted dosage of fluvoxamine.
Two mothers breastfeeding while taking stable doses of fluvoxamine were studied with timed blood and milk samples over 24 hours. The first patient, who was taking 150 mg daily and nursing a 26-month-old, had a peak milk level of 425 mcg/L at 2.1 hours after the dose. The second patient, who was taking 50 mg daily and nursing a 3-week-old, had a peak milk level of 67 mcg/L at 4.2 hours after the dose. The authors estimated the absolute infant dosages to be 38.4 and 5.4 mcg/kg daily in the two infants, respectively, or an average 1.38% and 0.8% of the maternal weight-adjusted dosage.[4]
A nursing mother was taking fluvoxamine 50 mg daily during pregnancy and postpartum. Foremilk and hindmilk samples taken on day 2 postpartum, 11.5 and 13 hours after a dose, contained fluvoxamine 23 mcg/L and 27 mcg/L, respectively. Foremilk and hindmilk samples taken during the fourth week postpartum, 9.9 and 10.3 hours after a dose, contained fluvoxamine 16.9 mcg/L and 43.3 mcg/L, respectively. The greater difference in hindmilk drug concentration was attributed to the higher fat content of mature milk and the lipid solubility of fluvoxamine.[5]
Infant Levels. Four exclusively breastfed infants aged 6 to 13 weeks had undetectable (<1 mcg/L) fluvoxamine serum levels during maternal therapy with fluvoxamine in dosages of 100 to 150 mg daily.[6]
In a pooled analysis of 3 mother-infant pairs from published and unpublished cases, the authors found that breastfed infants had an average of 16% (range 0 to 45%) of their mothers' fluvoxamine plasma levels; 1 of the 3 infants had a plasma level greater than 10% of the mother's which was defined by the authors as being elevated.[3] In the infant with a serum concentration of 45% of the maternal serum concentration, the high concentration was considered anomalous by the authors and perhaps related to the infant's fluvoxamine metabolism by P450 enzymes.[7]
Serum levels of fluvoxamine were undetectable (<2 mcg/L) in a partially breastfed 26-month-old during maternal intake of 150 mg daily. Fluvoxamine was also undetectable in the serum of an exclusively breastfed 3-week-old during maternal intake of 50 mg daily.[4]
Effects in Breastfed Infants
One infant whose mother began taking fluvoxamine 100 mg daily 17 weeks postpartum was breastfed from birth to 5 months of age. The medical and nursing staff did not note any adverse effect in the infant during the 10 weeks of observation during maternal hospitalization. The infant had normal Bayley developmental scores at age 4 months and 21 months.[8]
No adverse effects were found in 2 infants, a partially breastfed 26-month-old during maternal intake of 150 mg daily, who also had a normal Denver Developmental Score, and an exclusively breastfed 3-week-old during maternal intake of 50 mg daily.[4]
Three mothers who took an average fluvoxamine dose of 117 mg once daily breastfed their infants exclusively for 4 months and at least 50% during months 5 and 6. Their infants had 6-month weight gains that were normal according to national growth standards and the mothers reported no abnormal effects in their infants.[9]
One study of the side effects of SSRI antidepressants in nursing mothers found no adverse reactions that required medical attention in one infant whose mother was taking fluvoxamine. No specific information on maternal fluvoxamine dosage, extent of breastfeeding or infant age was reported.[10]
A woman who was treated chronically with quetiapine 400 mg and fluvoxamine 200 mg daily took the drugs throughout pregnancy and postpartum. She partially breastfed her infant (extent not stated) for 3 months from birth. No adverse events were seen in the infant who developed normally.[11]
A cohort of 247 infants exposed to an antidepressant in utero during the third trimester of pregnancy were assessed for poor neonatal adaptation (PNA). Of the 247 infants, 154 developed PNA. Infants who were exclusively given formula had about 3 times the risk of developing PNA as those who were exclusively or partially breastfed. Four of the infants were exposed to low doses of fluvoxamine in utero and none had PNA.[12]
A 5-month-old infant developed severe diarrhea (15 times daily), mild vomiting (2 to 3 times daily), agitation and decreased sleep within 2 days after maternal initiation of fluvoxamine 50 mg daily. Symptoms resolved within 24 hours after the mother discontinued the drug and recurred a week later after fluvoxamine was restarted in the mother. Other causes of the gastrointestinal symptoms could not be found. Fluvoxamine was probably the cause of the reaction. The authors speculate that the infant might have abnormal metabolism of the drug that resulted in high serum concentrations.[13]
Effects on Lactation and Breastmilk
Fluvoxamine has caused increased prolactin levels and galactorrhea in nonpregnant, nonnursing patients.[14-18] In one case, euprolactinemic gynecomastia and galactorrhea occurred in a 19-year-old man who was also taking risperidone.[19] In a study of cases of hyperprolactinemia and its symptoms (e.g., gynecomastia) reported to a French pharmacovigilance center, fluvoxamine was found to have a 4.5-fold increased risk of causing hyperprolactinemia compared to other drugs.[20] The prolactin level in a mother with established lactation may not affect her ability to breastfeed.
In a small prospective study, 8 primiparous women who were taking a serotonin reuptake inhibitor (SRI; 3 taking fluoxetine and 1 each taking citalopram, duloxetine, escitalopram, paroxetine or sertraline) were compared to 423 mothers who were not taking an SRI. Mothers taking an SRI had an onset of milk secretory activation (lactogenesis II) that was delayed by an average of 16.7 hours compared to controls (85.8 hours postpartum in the SRI-treated mothers and 69.1 h in the untreated mothers), which doubled the risk of delayed feeding behavior in the untreated group. However, the delay in lactogenesis II may not be clinically important, since there was no statistically significant difference between the groups in the percentage of mothers experiencing feeding difficulties after day 4 postpartum.[21]
A case control study compared the rate of predominant breastfeeding at 2 weeks postpartum in mothers who took an SSRI antidepressant throughout pregnancy and at delivery (n = 167) or an SSRI during pregnancy only (n = 117) to a control group of mothers who took no antidepressants (n = 182). Among the two groups who had taken an SSRI, 33 took citalopram, 18 took escitalopram, 63 took fluoxetine, 2 took fluvoxamine, 78 took paroxetine, and 87 took sertraline. Among the women who took an SSRI, the breastfeeding rate at 2 weeks postpartum was 27% to 33% lower than mother who did not take antidepressants, with no statistical difference in breastfeeding rates between the SSRI-exposed groups.[22]
An observational study looked at outcomes of 2859 women who took an antidepressant during the 2 years prior to pregnancy. Compared to women who did not take an antidepressant during pregnancy, mothers who took an antidepressant during all 3 trimesters of pregnancy were 37% less likely to be breastfeeding upon hospital discharge. Mothers who took an antidepressant only during the third trimester were 75% less likely to be breastfeeding at discharge. Those who took an antidepressant only during the first and second trimesters did not have a reduced likelihood of breastfeeding at discharge.[23] The antidepressants used by the mothers were not specified.
A retrospective cohort study of hospital electronic medical records from 2001 to 2008 compared women who had been dispensed an antidepressant during late gestation (n = 575; fluvoxamine n = 18) to those who had a psychiatric illness but did not receive an antidepressant (n = 1552) and mothers who did not have a psychiatric diagnosis (n = 30,535). Women who received an antidepressant were 37% less likely to be breastfeeding at discharge than women without a psychiatric diagnosis, but no less likely to be breastfeeding than untreated mothers with a psychiatric diagnosis.[24]
In a study of 80,882 Norwegian mother-infant pairs from 1999 to 2008, new postpartum antidepressant use was reported by 392 women and 201 reported that they continued antidepressants from pregnancy. Compared with the unexposed comparison group, late pregnancy antidepressant use was associated with a 7% reduced likelihood of breastfeeding initiation, but with no effect on breastfeeding duration or exclusivity. Compared with the unexposed comparison group, new or restarted antidepressant use was associated with a 63% reduced likelihood of predominant, and a 51% reduced likelihood of any breastfeeding at 6 months, as well as a 2.6-fold increased risk of abrupt breastfeeding discontinuation. Specific antidepressants were not mentioned.[25]
Alternate Drugs to Consider
References
- 1.
- Uguz F. A new safety scoring system for the use of psychotropic drugs during lactation. Am J Ther. 2021;28:e118–e126. [PubMed: 30601177]
- 2.
- Grzeskowiak LE, Leggett C, Costi L, et al. Impact of serotonin reuptake inhibitor use on breast milk supply in mothers of preterm infants: A retrospective cohort study. Br J Clin Pharmacol. 2018;84:1373–9. [PMC free article: PMC5980248] [PubMed: 29522259]
- 3.
- Weissman AM, Levy BT, Hartz AJ, et al. Pooled analysis of antidepressant levels in lactating mothers, breast milk, and nursing infants. Am J Psychiatry. 2004;161:1066–78. [PubMed: 15169695]
- 4.
- Kristensen JH, Hackett LP, Kohan R, et al. The amount of fluvoxamine in milk is unlikely to be a cause of adverse effects in breastfed infants. J Hum Lact. 2002;18:139–43. [PubMed: 12033075]
- 5.
- Monfort A, Cardoso E, Eap CB, et al. Infant exposure to fluvoxamine through placenta and human milk: A case series - A contribution from the ConcePTION project. Front Psychiatry. 2023;14:1167870. [PMC free article: PMC10232980] [PubMed: 37275991] [CrossRef]
- 6.
- Hendrick V, Fukuchi A, Altshuler L, et al. Use of sertraline, paroxetine and fluvoxamine by nursing women. Br J Psychiatry. 2001;179:163–6. [PubMed: 11483479]
- 7.
- Arnold LM, Suckow RF, Lichtenstein PK. Fluvoxamine concentrations in breast milk and in maternal and infant sera. J Clin Psychopharmacol. 2000;20:491–2. [Letter] [PubMed: 10917415]
- 8.
- Yoshida K, Smith B, Kumar RC. Fluvoxamine in breast-milk and infant development. Br J Clin Pharmacol. 1997;44:210–1. [PubMed: 9278215]
- 9.
- Hendrick V, Smith LM, Hwang S, et al. Weight gain in breastfed infants of mothers taking antidepressant medications. J Clin Psychiatry. 2003;64:410–2. [PubMed: 12716242]
- 10.
- Lee A, Woo J, Ito S. Frequency of infant adverse events that are associated with citalopram use during breast-feeding. Am J Obstet Gynecol. 2004;190:218–21. [PubMed: 14749663]
- 11.
- Gentile S. Quetiapine-fluvoxamine combination during pregnancy and while breastfeeding. Arch Womens Ment Health. 2006;9:158–9. [PubMed: 16683078]
- 12.
- Kieviet N, Hoppenbrouwers C, Dolman KM, et al. Risk factors for poor neonatal adaptation after exposure to antidepressants in utero. Acta Paediatr. 2015;104:384–91. [PubMed: 25559357]
- 13.
- Uguz F. Gastrointestinal side effects in the baby of a breastfeeding woman treated with low-dose fluvoxamine. J Hum Lact. 2015;31:371–3. [PubMed: 25896469]
- 14.
- Bonin B, Vandel P, Vandel S. Fluvoxamine and galactorrhea. A case report. Therapie. 1994;49:149–51. [PubMed: 7817347]
- 15.
- Egberts AC, Meyboom RH, De Koning FH, et al. Non-puerperal lactation associated with antidepressant drug use. Br J Clin Pharmacol. 1997;44:277–81. [PMC free article: PMC2042834] [PubMed: 9296322]
- 16.
- Jeffries J, Bezchlibnyk-Butler K, Remington G. Amenorrhea and galactorrhea associated with fluvoxamine in a loxapine-treated patient. J Clin Psychopharmacol. 1992;12:296–7. [PubMed: 1527236]
- 17.
- Chakladar A, Singh J, Tak NK, et al. Fluvoxamine-associated galactorrhea: A case report. J Clin Psychopharmacol. 2020;40:101–2. [PubMed: 31804454] [CrossRef]
- 18.
- Bhattacharjee S, Biswas R, Mandal N. Selective serotonin reuptake inhibitor-induced galactorrhea with hyperprolactinemia. Indian J Psychiatry. 2021;63:613–6. [PMC free article: PMC8793705] [PubMed: 35136264]
- 19.
- Pratheesh PJ, Praharaj SK, Srivastava A. Euprolactinemic gynecomastia and galactorrhea with risperidone-fluvoxamine combination. Psychopharmacol Bull. 2011;44:70–3. [PMC free article: PMC5044559] [PubMed: 22506441]
- 20.
- Trenque T, Herlem E, Auriche P, et al. Serotonin reuptake inhibitors and hyperprolactinaemia: A case/non-case study in the French pharmacovigilance database. Drug Saf. 2011;34:1161–6. [PubMed: 22077504]
- 21.
- Marshall AM, Nommsen-Rivers LA, Hernandez LL, et al. Serotonin transport and metabolism in the mammary gland modulates secretory activation and involution. J Clin Endocrinol Metab. 2010;95:837–46. [PMC free article: PMC2840848] [PubMed: 19965920]
- 22.
- Gorman JR, Kao K, Chambers CD. Breastfeeding among women exposed to antidepressants during pregnancy. J Hum Lact. 2012;28:181–8. [PubMed: 22344850]
- 23.
- Venkatesh KK, Castro VM, Perlis RH, et al. Impact of antidepressant treatment during pregnancy on obstetric outcomes among women previously treated for depression: An observational cohort study. J Perinatol. 2017;37:1003–9. [PMC free article: PMC10034861] [PubMed: 28682318]
- 24.
- Leggett C, Costi L, Morrison JL, et al. Antidepressant use in late gestation and breastfeeding rates at discharge from hospital. J Hum Lact. 2017;33:701–9. [PubMed: 28984528]
- 25.
- Grzeskowiak LE, Saha MR, Nordeng H, et al. Perinatal antidepressant use and breastfeeding outcomes: Findings from the Norwegian Mother, Father and Child Cohort Study. Acta Obstet Gynecol Scand. 2022;101:344–54. [PMC free article: PMC9564556] [PubMed: 35170756]
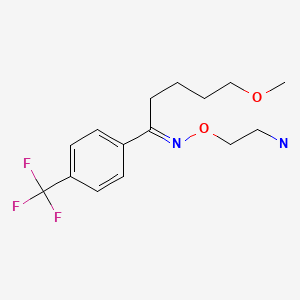
Substance Identification
Substance Name
Fluvoxamine
CAS Registry Number
54739-18-3
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Bupropion.[Drugs and Lactation Database (...]Review Bupropion.. Drugs and Lactation Database (LactMed®). 2006
- Review Escitalopram.[Drugs and Lactation Database (...]Review Escitalopram.. Drugs and Lactation Database (LactMed®). 2006
- Review Fentanyl.[Drugs and Lactation Database (...]Review Fentanyl.. Drugs and Lactation Database (LactMed®). 2006
- Review Fluoxetine.[Drugs and Lactation Database (...]Review Fluoxetine.. Drugs and Lactation Database (LactMed®). 2006
- Review Trazodone.[Drugs and Lactation Database (...]Review Trazodone.. Drugs and Lactation Database (LactMed®). 2006
- Fluvoxamine - Drugs and Lactation Database (LactMed®)Fluvoxamine - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
