Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 83-43-2
Drug Levels and Effects
Summary of Use during Lactation
Amounts of methylprednisolone in breastmilk are very low and no adverse reactions in breastfed infants have been reported, even with intravenous doses of 1 gram. With maternal intravenous doses of 1 gram, fully breastfed infants would receive doses less than their daily cortisol output, and much less than the therapeutic dose used in neonates.[1,2] Accumulation of the drug does not occur in breastmilk with consecutive daily doses of 1 gram. Avoiding breastfeeding during the infusion and for as little as 2 hours after a 1 gram intravenous dose markedly reduces infant exposure. Smaller oral doses and local injections, such as for tendinitis, require no special precautions. Medium to large doses of corticosteroids given systemically or injected into joints or the breast have been reported to cause temporary reduction of lactation.
Drug Levels
Maternal Levels. In one woman taking 6 mg daily of methylprednisolone by mouth, 2 peak milk levels occurred: one at 2 hours after the dose and another 8 hours after the dose. Peaks were about 7 mcg/L, while levels fell to about 2.5 mcg/L 6 hours after the dose and to about 1 mcg/L 10 hours after the dose.[3]
A woman with multiple sclerosis had a relapse in the first 3 months postpartum. She was given intravenous methylprednisolone 1 gram daily for 3 days. Milk samples were obtained after one of the doses. The breastmilk methylprednisolone was 3 mg/L immediately after the dose and 1.2 mg/L at 4 hours after the dose. The authors estimated that an infant who nurses at 4 hours after a dose will ingest 0.168 mg of methylprednisolone which is equivalent of 0.84 mg of cortisol or 42% of the daily output. An infant who nurses starting at 8 hours after a dose will ingest 0.048 mg of methylprednisolone which is equivalent to 12% of daily cortisol production. The authors did not specify their method of calculating these values.[4]
A woman with multiple sclerosis who was 5 months postpartum received 1 gram of methylprednisolone infused intravenously over 2 hours on 3 successive days. She provided milk samples at 0, 1, 2, 4, 8 and 12 hours after each dose. Breastmilk levels at 0 and 12 hours were not quantifiable (<0.06 mg/L). Peak levels occurred at 1 hour after the end of the infusion and averaged 5.3 mg/L (range 5.1 to 5.6 mg/L). By 4 hours after the dose, milk levels averaged 1.1 mg/L (range 1.0 to 1.6 mg/L) and by 8 hours, milk levels averaged 0.27 mg/L (range 0.2 to 0.37 mg/L). The authors calculated that a fully breastfed infant would have received an average of 0.19 mg/kg daily (range 0.16 to 0.21 mg/kg daily) of methylprednisolone, which is less than the lowest recommended therapeutic dose for infants. Withholding nursing for 2 to 4 hours after a dose would reduce the dose substantially.[5]
A woman who was nursing a 9-month-old infant was given intravenous methylprednisolone 1 gram daily for 3 days to treat multiple sclerosis. Cortisol milk levels were measured in breastmilk because of a lack of a methylprednisolone assay. The milk cortisol concentration was 306 mcg/L at the fourth hour after the last dose, which the authors state is approximately equal to the endogenous production of cortisol in an infant (note that normal breastmilk cortisol is less than 20 mcg/L). The authors considered that waiting 4 hours after a 1 gram dose of methylprednisolone before resuming breastfeeding to be adequate.[6]
Sixteen nursing mothers with multiple sclerosis received 1 gram of methylprednisolone intravenously over 1 hour, either monthly (n = 7) or over 3 consecutive days (n = 9).[7] Breastmilk samples were taken at 1, 2 4, 8 and 12 hours after each dose, and 2 women receiving 3 doses also provided milk samples prior to their doses. Peak milk methylprednisolone concentrations occurred 1 hour after the end of the infusion in all women and averaged 1.24 mg/L (range 0.55 to 2.1 mg/L). Subsequent average milk levels were 0.76 mg/L, 0.29 mg/L, 0.04 mg/L and 0.01 mg/L at 2, 4, 8 and 12 hours after the infusion, respectively. The average daily dosage over the 13 hours from the start of the infusion to 12 hours after the infusion was 0.047 mg/kg. No accumulation of the drug occurred in breastmilk of the mothers receiving 3 consecutive days of therapy.[7]
Twelve women with postpartum relapses of multiple sclerosis were given 1-hour infusions of methylprednisolone 1 gram daily for 3 to 5 days. Maternal blood and milk samples were obtained before and 0.5 hours after the start of the infusion, at the end of the infusion, and 1, 2, 4, 8, 12, and 24 hours after the end of the infusion. Milk methylprednisolone levels averaged 1, 2.09, 1.9, 1.17, 0.59, and 0.04 mg/L through 8 hours, respectively. Milk levels were below the quantification limit (<0.026 mg/L) before the infusion and at 12 and 24 hours after the infusion. The average milk level over 24 hours was 0.46 mg/L which resulted in an average infant dosage of 0.0695 mg/kg daily and a weight-adjusted relative infant dosage of 0.5%.[8]
Infant Levels. Relevant published information was not found as of the revision date.
Effects in Breastfed Infants
None reported with methylprednisolone or any other corticosteroid. Three infants were breastfed from birth during maternal use of methylprednisolone 6 to 8 mg daily with no reported adverse effects up to 3 months. In one of the papers, 2 infants had normal blood cell counts, no increase in infections and above average growth rates.[3,9]
Sixteen nursing mothers with multiple sclerosis received 1 gram of methylprednisolone intravenously over 1 hour, either monthly (n = 7) or over 3 consecutive days (n = 9). Infants did not breastfeed for 4 hours after the dose. No adverse effects were observed in infants during 3 to 12 months of follow-up.[7]
A woman with rheumatoid arthritis was treated during pregnancy with methylprednisolone 8 to 16 mg daily. After delivery, she was maintained on methylprednisolone 8 mg daily plus corticosteroid (not specified) injections into her metacarpal joints while breastfeeding (extent not stated) her infant. At 9 months of age, the baby had normal growth and psychomotor development, with no clinical nor laboratory alterations. The baby received routine vaccinations with no adverse effects.[10]
Twelve infants of mothers receiving methylprednisolone 1 gram intravenously over 1 hour for 3 or 5 days were breastfed by their mothers except for the first 2 hours after the infusion. The infants averaged 8 months of age (range 1 to 16 months). The infants were normal in weight and height and had reached their milestones at the time of the study. No adverse effects were seen in the infants during a 6 to 24 month follow-up period.[8]
Effects on Lactation and Breastmilk
A patient who was 6 weeks postpartum and predominantly breastfeeding her infant received 24 mg of depot methylprednisolone plus 15 mg of lidocaine intralesionally for tenosynovitis of the wrist. Thirty hours after the injection, lactation ceased. Her breasts were soft and not engorged at that time. Thirty-six hours later, lactation resumed slowly, reaching normal milk production 24 hours later. The author hypothesized that the suppression might have occurred because the injection was in a highly mobile joint, which might have caused rapid release of the corticosteroid. Medium to large doses of corticosteroids given systemically or injected into joints or the breast have been reported to cause temporary reduction of lactation.[11-15]
A study of 46 women who delivered an infant before 34 weeks of gestation found that a course of another corticosteroid (betamethasone, 2 intramuscular injections of 11.4 mg of betamethasone 24 hours apart) given between 3 and 9 days before delivery resulted in delayed lactogenesis II and lower average milk volumes during the 10 days after delivery. Milk volume was not affected if the infant was delivered less than 3 days or more than 10 days after the mother received the corticosteroid.[16] An equivalent dosage regimen of methylprednisolone might have the same effect.
A study of 87 pregnant women found that betamethasone given as above during pregnancy caused a premature stimulation of lactose secretion during pregnancy. Although the increase was statistically significant, the clinical importance appears to be minimal.[17] An equivalent dosage regimen of methylprednisolone might have the same effect.
Sixteen nursing mothers with multiple sclerosis received 1 gram of methylprednisolone intravenously over 1 hour, either monthly (n = 7) or over 3 consecutive days (n = 9). None of the mothers reported a decrease in their milk supply.[12]
Alternate Drugs to Consider
References
- 1.
- Drago BB, Kimura D, Rovnaghi CR, et al. Double-blind, placebo-controlled pilot randomized trial of methylprednisolone infusion in pediatric acute respiratory distress syndrome. Pediatr Crit Care Med 2015;16:e74-81. [PubMed: 25634565]
- 2.
- Huang YY, Chen MJ, Chiu NT, et al. Adjunctive oral methylprednisolone in pediatric acute pyelonephritis alleviates renal scarring. Pediatrics 2011;128:e496-504. [PubMed: 21844061]
- 3.
- Coulam CB, Moyer TP, Jiang NS, et al. Breast-feeding after renal transplantation. Transplant Proc 1982;14:605-9. [PubMed: 6817481]
- 4.
- Strijbos E, Coenradie S, Touw DJ, et al. High-dose methylprednisolone for multiple sclerosis during lactation: Concentrations in breast milk. Mult Scler 2015;21:797-8. [PubMed: 25583837]
- 5.
- Cooper SD, Felkins K, Baker TE, et al. Transfer of methylprednisolone into breast milk in a mother with multiple sclerosis. J Hum Lact 2015;31:237-9. [PubMed: 25691380]
- 6.
- Gunduz S, Gencler OS, Celik HT. Four hours is enough for lactation interruption after high-dose methylprednisolone treatment in multiple sclerosis mothers by measuring milk cortisol levels. J Matern Fetal Neonatal Med 2016;29:3495. [PubMed: 26755401]
- 7.
- Boz C, Terzi M, Zengin Karahan, S, et al. Safety of IV pulse methylprednisolone therapy during breastfeeding in patients with multiple sclerosis. Mult Scler 2018;24:1205-11. [PubMed: 28649909]
- 8.
- Zengin Karahan S, Boz C, Terzi M, et al. Methylprednisolone concentrations in breast milk and serum of patients with multiple sclerosis treated with IV pulse methylprednisolone. Clin Neurol Neurosurg 2020;197:106118. [PubMed: 32768896]
- 9.
- Grekas DM, Vasiliou SS, Lazarides AN. Immunosuppressive therapy and breast-feeding after renal transplantation. Nephron 1984;37:68. [PubMed: 6371564]
- 10.
- Costanzo G, Firinu D, Losa F, et al. Baricitinib exposure during pregnancy in rheumatoid arthritis. Ther Adv Musculoskelet Dis 2020;12:1759720X19899296. [PMC free article: PMC6997965] [PubMed: 32071617]
- 11.
- McGuire E. Sudden loss of milk supply following high-dose triamcinolone (Kenacort) injection. Breastfeed Rev 2012;20:32-4. [PubMed: 22724311]
- 12.
- Babwah TJ, Nunes P, Maharaj RG. An unexpected temporary suppression of lactation after a local corticosteroid injection for tenosynovitis. Eur J Gen Pract 2013;19:248-50. [PubMed: 24261425]
- 13.
- Smuin DM, Seidenberg PH, Sirlin EA, et al. Rare adverse events associated with corticosteroid injections: A case series and literature review. Curr Sports Med Rep 2016;15:171-6. [PubMed: 27172081]
- 14.
- Das N, Dave S, Dangaich R, et al. Lactation failure following therapeutic steroid treatment in a mother with postpartum depression and spinal-dural arteriovenous fistula: Case report and literature review. Int J Gynaecol Obstet 2024;165:389-91. [PubMed: 38093554]
- 15.
- Rosen-Carole C, Datta P, Palmiter K, et al. Transfer of injected triamcinolone into human milk of a lactating patient suffering from idiopathic granulomatous mastitis. Breastfeed Med 2023;18:74-7. [PubMed: 36638194]
- 16.
- Henderson JJ, Hartmann PE, Newnham JP, et al. Effect of preterm birth and antenatal corticosteroid treatment on lactogenesis II in women. Pediatrics 2008;121:e92-100. [PubMed: 18166549]
- 17.
- Henderson JJ, Newnham JP, Simmer K, et al. Effects of antenatal corticosteroids on urinary markers of the initiation of lactation in pregnant women. Breastfeed Med 2009;4:201-6. [PubMed: 19772378]
Substance Identification
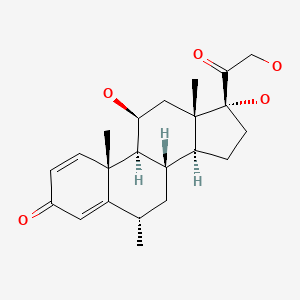
Substance Name
Methylprednisolone
CAS Registry Number
83-43-2
Drug Class
Breast Feeding
Lactation
Milk, Human
Corticosteroids, Systemic
Glucocorticoids
Anti-Inflammatory Agents
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Prednisolone.[Drugs and Lactation Database (...]Review Prednisolone.. Drugs and Lactation Database (LactMed®). 2006
- Review Hydrocortisone.[Drugs and Lactation Database (...]Review Hydrocortisone.. Drugs and Lactation Database (LactMed®). 2006
- Review Triamcinolone.[Drugs and Lactation Database (...]Review Triamcinolone.. Drugs and Lactation Database (LactMed®). 2006
- Review Prednisone.[Drugs and Lactation Database (...]Review Prednisone.. Drugs and Lactation Database (LactMed®). 2006
- Review Dexamethasone.[Drugs and Lactation Database (...]Review Dexamethasone.. Drugs and Lactation Database (LactMed®). 2006
- Methylprednisolone - Drugs and Lactation Database (LactMed®)Methylprednisolone - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
