Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 84-80-0
Drug Levels and Effects
Summary of Use during Lactation
Vitamin K is naturally found in human milk. Maternal vitamin K supplementation is typically not needed to meet the 75 mcg per day recommended adequate maternal dietary intake during lactation.[1] Maternal supplementation with 5 mg daily increases milk vitamin K levels and can improve vitamin K status in breastfed infants who also receive intramuscular vitamin K shortly after birth. Although exclusively breastfed infants are at higher risk of vitamin K deficiency bleeding (VKDB), a condition that can involve intracranial hemorrhage, sometimes leading to infant death, maternal vitamin K supplementation alone is not an adequate or safe substitute for vitamin K administered directly to the newborn after birth to prevent VKDB, especially in preterm infants.[2-4]
Drug Levels
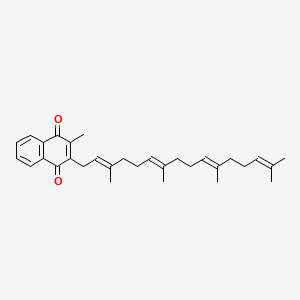
Maternal Levels. Vitamin K is naturally present in human milk in concentrations of 1 to 9 mcg/L (2.2 to 20 nmol/L).[5,6] Similar levels have been reported in colostrum.[5] Levels are approximately 1 mcg/L higher in hindmilk than foremilk.[7] Vitamin K1 (phylloquinone) is the predominant form in plasma and milk and derives from maternal dietary plant sources. Vitamin K2 (menaquinones) are also present in milk, mainly as menatetrenone (menaquninone-4; MK-4), at approximately one-half the levels of vitamin K1.[6,8] Since MK-4 can be synthesized from phylloquinone in the mother, dietary phylloquinone is the main source of milk MK-4.[8] It can also be derived from maternal dietary poultry in countries where vitamin K3 (menadione), a chemical precursor of MK-4, is used in poultry feed.[9] Other menaquinones are synthesized by some bacteria. Their milk levels can be increased in mothers who consume certain fermented foods.[6] Relevant published information regarding vitamin K milk levels in mothers taking MK-4 supplements was not found as of the revision date.
Four lactating mothers were given 0.1, 0.5, 1, or 3 mg single doses of oral vitamin K1. Milk was sampled at baseline and then at random times over 2 days after administration in 3 of the mothers and at fixed 6-hour intervals over 1 day in the fourth mother. Baseline milk levels were 2 to 3 mcg/L. Peak milk vitamin K1 levels occurred at 12 to 24 hours after administration in all subjects. The highest level reported was approximately 150 mcg/L, occurring 18 hours after a 3 mg dose. Menaquinone levels were not measured.[7]
Eleven lactating mothers between 2 and 6 months postpartum were given a single oral 20 mg vitamin K1 supplement and their milk was collected at 0, 12, 24, 48, 96 hours, and 1 week after administration. The average peak milk vitamin K1 level was approximately 130 mcg/L at 12 hours after administration compared to 1.1 mcg/L at baseline. By 48 hours the average milk level had decreased to 35 mcg/L, and returned to baseline after 1 week. Menaquinone levels were not measured.[10]
Twenty exclusively breastfeeding mothers were given either 2.5 or 5 mg of oral vitamin K1 once daily for 6 weeks beginning within 3 days of delivery. All infants were given 1 mg of intramuscular vitamin K1 at birth. Breastmilk samples were collected at baseline and 18 to 24 hours after a dose (peak level) at 2 and 6 weeks. Average milk vitamin K1 levels were approximately 1 mcg/L at baseline in both groups, increasing to 27 and 59 mcg/L at 2 weeks, and 22 and 44 mcg/L at 6 weeks, in the 2.5 mg and 5 mg groups, respectively. The same investigators then gave 5 mg or placebo to 22 different exclusively breastfeeding mothers on the same postpartum schedule, but for 12 weeks instead of 6 weeks. At 2, 6 and 12 weeks, average milk vitamin K1 levels were approximately 80 mcg/L in the 5 mg group and 1 mcg/L in the placebo group at all three time points. Menaquinone levels were not measured.[11] Using the milk levels reported in this study, an exclusively breastfed infant would receive 12 mcg/kg daily of vitamin K1 from a daily 5 mg maternal vitamin K1 dose.
Six lactating mothers of preterm infants ranging from 26 to 30 weeks gestation were given 2.5 mg of oral vitamin K1 once daily for 2 weeks beginning at 2 weeks postpartum. Breastmilk vitamin K1 was measured at baseline, then daily for 14 days. Milk was collected 6 times a day during routine pumping to calculate a daily average level in the mothers' milk. The average baseline milk level was 3 mcg/L. This increased to 22.6 mcg/L after 1 day, then gradually increased daily to 64.2 mcg/L on day 6 with no further significant changes. Menaquinone levels were not measured.[12] Based on the highest average level reported in this study, an exclusively maternal breastmilk fed preterm infant would receive 9 mcg/kg daily from a maternal vitamin K1 dose of 2.5 mg daily.
Thirty-one lactating mothers were given 0, 0.8, 2, or 4 mg of oral vitamin K1 once daily beginning on postpartum day 4 and continuing until day 16. Milk was sampled at baseline, and then prior to administration on days 8, 16, and 19. At baseline, the average milk vitamin K1 level was 6 to 7 mcg/L and the average milk MK-4 level was 2 to 3 mcg/L in all groups. Milk levels did not significantly change in the control (0 mg) group over time. On day 8 the average vitamin K1 levels were 23.3, 41.3, and 88.7 mcg/L, and MK-4 levels were 2.7, 3.8, 9.9 mcg/L in the 0.8, 2 and 4 mg groups, respectively. On day 16 average vitamin K1 levels were 24.5, 60.6, and 139.6 mcg/L, and MK-4 levels were 3.5, 5.5, and 16.5 mcg/L, respectively. On day 19, three days after maternal supplement discontinuation, average levels decreased to 12.4, 12.1, and 44.9 mcg/L, and MK-4 decreased to levels of 3.2, 3 and 9 mcg/L, respectively. Only the 4 mg group still had levels higher than the control group on day 19. The authors reported a highly significant correlation between vitamin K1 and MK-4 milk levels.[8] Using the highest average milk levels of both vitamin K1 and MK-4 reported in this study, an exclusively breastfed infant would receive a daily dosage of 23 mcg/kg of total vitamin K from a maternal 4 mg daily vitamin K1 supplement.
Infant Levels. Twenty-two exclusively breastfeeding mothers were given either 5 mg of oral vitamin K1 or placebo once daily for 12 weeks beginning within 3 days of delivery. All infants were given 1 mg of intramuscular vitamin K1 at birth. Average infant plasma vitamin K1 levels were between 2 and 3 mcg/L at 2, 6, and 12 weeks in the 5 mg group compared to between 0.2 and 0.4 mcg/L in the placebo group. Average infant PIVKA-II (des-gamma-carboxy-prothrombin) levels at 12 weeks were 0.42 mcg/L in the 5 mg group compared to 1.48 mcg/L in the placebo group (upper limit of normal is 2 mcg/L). The higher level in the placebo group suggests a relative vitamin K deficiency. Infant prothrombin times at 2, 6, and 12 weeks were not different between the two groups.[11]
Effects in Breastfed Infants
Exclusive breastfeeding and failure to give infants a dose of prophylactic vitamin K at birth resulted in the death of 3 otherwise normal, consecutive male siblings from intracranial hemorrhage. A fourth male sibling was examined at 17 days of age and found to have abnormal clotting parameters. The infant and parents were found to have no genetic conditions that could account for the abnormal clotting. Within 24 hours, the infant’s clotting profile normalized after 1 mg of vitamin K injection.[3]
Effects on Lactation and Breastmilk
Effects in Breastfed Infants
Three consecutive, full term, home-born, male singletons in India from the same set of parents died between 1 to 2 months of age due to intracranial hemorrhage. All three were exclusively breastfed and were not given prophylactic vitamin K at birth. The fourth singleton was pre-emptively examined at 17 days of age and found to have abnormal clotting parameters. The fourth infant and parents were determined to have no genetic conditions that could account for the abnormal clotting. Within 24 hours, the infant’s clotting profile normalized after 1 mg of intramuscular vitamin K injection.[3]
Thirty-seven preterm infants across four UK neonatal intensive care units were given a standard injection of intramuscular vitamin K1 after birth. When enteral feedings were initiated, they were fed breastmilk and then eventually breastmilk plus a bovine-derived milk fortifier containing vitamin K, per routine feeding protocol. Prior to discharge home, serum biomarkers of vitamin K status were normal. After discharge at 48 weeks postmenstrual age, 12 were exclusively fed breastmilk only, and 25 were fed formula or mixed breastmilk and formula. In the former group, 67% had abnormal biomarkers indicating vitamin K deficiency, compared to 4% of the latter group. No bleeding events were reported.[13]
A 23-week gestational age preterm female infant in a UK neonatal intensive care unit was fed her mother’s milk plus a human milk derived fortifier. Although she was administered 0.2 mg of vitamin K1 after birth, she developed vitamin K deficiency related minor bleeding on postnatal day 73.[14]
References
- 1.
- National Institutes of Health Office of Dietary Supplements. Vitamin K fact sheet for health professionals. 2021. [Accessed December 9, 2023]. https://ods
.od.nih.gov /factsheets/VitaminK-HealthProfessional/. - 2.
- Shahrook S, Ota E, Hanada N, et al. Vitamin K supplementation during pregnancy for improving outcomes: A systematic review and meta-analysis. Sci Rep 2018;8:11459. [PMC free article: PMC6065418] [PubMed: 30061633]
- 3.
- Mahajan V, Tahlan A, Azad C, et al. Recurrent intracranial bleed in 3 siblings: Short of a shot of vitamin K! J Pediatr Hematol Oncol 2021;43:e580-e582. [PubMed: 32404684]
- 4.
- Hand I, Noble L, Abrams SA. Vitamin K and the newborn infant. Pediatrics 2022;149:e2021056036. [PubMed: 35190810]
- 5.
- Greer FR. Vitamin K status of lactating mothers and their infants. Acta Paediatr Suppl 1999;88 (Suppl 430):95-103. [PubMed: 10569231]
- 6.
- Kojima T, Asoh M, Yamawaki N, et al. Vitamin K concentrations in the maternal milk of Japanese women. Acta Paediatr 2004;93:457-63. [PubMed: 15188971]
- 7.
- von Kries, R, Shearer M, McCarthy PT, et al. Vitamin K1 content of maternal milk: influence of the stage of lactation, lipid composition, and vitamin K1 supplements given to the mother. Pediatr Res 1987;22:513-7. [PubMed: 3684378]
- 8.
- Thijssen HH, Drittij MJ, Vermeer C, Schoffelen E. Menaquinone-4 in breast milk is derived from dietary phylloquinone. Br J Nutr 2002;87:219-26. [PubMed: 12064330]
- 9.
- Booth SL. Vitamin K: Food composition and dietary intakes. Food Nutr Res 2012;56:5505. [PMC free article: PMC3321250] [PubMed: 22489217]
- 10.
- Greer FR, Marshall S, Cherry J, Suttie JW. Vitamin K status of lactating mothers, human milk, and breast-feeding infants. Pediatrics 1991;88:751-6. [PubMed: 1896278]
- 11.
- Greer FR, Marshall SP, Foley AL, Suttie JW. Improving the vitamin K status of breastfeeding infants with maternal vitamin K supplements. Pediatrics 1997;99:88-92. [PubMed: 8989344]
- 12.
- Bolisetty S, Gupta JM, Graham GG, et al. Vitamin K in preterm breastmilk with maternal supplementation. Acta Paediatr 1998;87:960-2. [PubMed: 9764891]
- 13.
- Clarke P, Shearer MJ, Card DJ, et al. Exclusively breastmilk-fed preterm infants are at high risk of developing subclinical vitamin K deficiency despite intramuscular prophylaxis at birth. J Thromb Haemost 2022;20:2773-85. [PMC free article: PMC9828794] [PubMed: 36087073]
- 14.
- Vasu V, Mulla S, Pandya A, et al. Late-onset vitamin K deficiency bleeding in an extremely preterm infant fed an exclusively human milk-based diet. J Thromb Haemost 2024;22:466-9. [PubMed: 37981048]
Substance Identification
Substance Name
Vitamin K
CAS Registry Number
84-80-0
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Vitamin D.[Drugs and Lactation Database (...]Review Vitamin D.. Drugs and Lactation Database (LactMed®). 2006
- Review Vitamin B(12).[Drugs and Lactation Database (...]Review Vitamin B(12).. Drugs and Lactation Database (LactMed®). 2006
- Review Vitamin A.[Drugs and Lactation Database (...]Review Vitamin A.. Drugs and Lactation Database (LactMed®). 2006
- Late-onset vitamin K deficiency bleeding in an extremely preterm infant fed an exclusively human milk-based diet.[J Thromb Haemost. 2024]Late-onset vitamin K deficiency bleeding in an extremely preterm infant fed an exclusively human milk-based diet.Vasu V, Mulla S, Pandya A, Card D, Shearer MJ, Clarke P. J Thromb Haemost. 2024 Feb; 22(2):466-469. Epub 2023 Nov 20.
- Review Beta-Carotene.[Drugs and Lactation Database (...]Review Beta-Carotene.. Drugs and Lactation Database (LactMed®). 2006
- Vitamin K - Drugs and Lactation Database (LactMed®)Vitamin K - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
