Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 33069-62-4
Drug Levels and Effects
Summary of Use during Lactation
Most sources consider breastfeeding to be contraindicated during maternal antineoplastic drug therapy.[1] It might be possible to breastfeed safely during intermittent therapy with an appropriate period of breastfeeding abstinence. Some have suggested a breastfeeding abstinence period of 6 to 10 days,[2] but more recent pharmacokinetic modeling using a worst-case scenario suggests that 6 days would be adequate to minimize both systemic and gut toxicity after the colostral phase.[3]
Chemotherapy may adversely affect the normal microbiome and chemical makeup of breastmilk.[4] Women who receive chemotherapy during pregnancy are more likely to have difficulty nursing their infant than typical mothers.
Drug Levels
Maternal Levels. A woman with a history of treatment for thyroid cancer and recurrence during pregnancy was treated postpartum with paclitaxel and carboplatin. Her intravenous paclitaxel dose was 56.1 mg (30 mg per square meter) weekly for 6 weeks. Whole milk samples were obtained at 4, 28, 172, and 316 hours after the sixth dose. The highest milk paclitaxel level was 1.17 mg/L in the 28-hour sample and paclitaxel was undetectable (<80 mcg/L) in the 316 hour sample. Metabolites were not measured. The authors calculated an average milk paclitaxel level over the 316 hour collection period of 0.78 mg/L, resulting in an estimated total weight-adjusted infant daily dose of 16.7% of the maternal weekly dose.[5] Note that the above estimate of the infant daily dose is expressed as percentage of the maternal weekly dose, and that authors used a level of zero as the trough milk level, rather than a milk level taken before the sixth dose (which would equal approximately the 172-hour level of 0.97 mg/L), resulting in an underestimate of the AUC and infant dose.
A 17-week pregnant woman with breast cancer received a regimen of fluorouracil, epirubicin and cyclophosphamide, followed by 9 weekly doses of paclitaxel 80 mg/sq. m. Her infant was delivered after the 6th dose of paclitaxel. She pumped milk and discarded it until after the 9th dose of paclitaxel when maternal blood and milk samples were collected. Paclitaxel concentration in milk was 111.4 mcg/L at 11 hours after the dose. Milk concentration decrease to 6.8 mcg/L at 27 hours after the dose. Milk paclitaxel levels were undetectable (<2.5 mcg/L) at 71.25 hours after the dose, and thereafter until 360 hours after the dose.[6]
A woman with breast cancer diagnosed during pregnancy received chemotherapy beginning a few days after delivery. It consisted of doxorubicin 118 mg and cyclophosphamide 1180 mg every 2 weeks for 4 cycles, followed by paclitaxel 156 mg weekly and carboplatin 900 mg every 4 weeks. She collected 97 milk samples over 3 cycles of chemotherapy. A selection of 26 samples were analyzed for paclitaxel. Milk levels increased with each dose, with peak levels ranging from 6 mcg/L after the first dose to 12.5 mcg/L after the second dose to about 20 mcg/L after the third dose. Milk levels dropped rapidly to less than 4 mcg/L by 2 days after the dose and to nearly 0 by 5 to 6 days after the dose. The authors calculated the times for the milk concentrations to reach various relative infant dosage (RID) levels. It took less than 1 day to fall below an RID of 1%. It took less than 1 day on the first two cycles and 1 day on the third cycle to fall below 0.1%, and 2 to 3 days to fall below 0.01%; however, potentially toxic metabolites were not measured.[7] A further pharmacokinetic analysis of all breastmilk samples found that paclitaxel levels in milk decrease rapidly and that milk need be discarded for 1 day or less after each dose in a cycle to achieve a cumulative relative infant dosage of <1%. However, this estimate did not include the presence of active metabolite(s) in milk, so this time represents the minimum time to withhold breastfeeding.[8]
The same authors developed a physiologically based pharmacokinetic model for paclitaxel. Assuming the worst-case scenario, the model predicted reductions of infant peripheral blood exposure of 71%, 86%, and 92% when milk was discarded for 1, 2, or 3 days after the maternal dose, respectively. In addition, the model predicted that it would take 6 days for the gut concentration to fall below the IC50 for cell death. However, these values apply only to mature milk and not necessarily to colostrum.[3]
Infant Levels. Relevant published information was not found as of the revision date.
Effects in Breastfed Infants
Relevant published information was not found as of the revision date.
Effects on Lactation and Breastmilk
A telephone follow-up study was conducted on 74 women who received cancer chemotherapy at one center during the second or third trimester of pregnancy to determine if they were successful at breastfeeding postpartum. Only 34% of the women were able to exclusively breastfeed their infants, and 66% of the women reported experiencing breastfeeding difficulties. This was in comparison to a 91% breastfeeding success rate in 22 other mothers diagnosed during pregnancy, but not treated with chemotherapy. Other statistically significant correlations included: 1. mothers with breastfeeding difficulties had an average of 5.5 cycles of chemotherapy compared with 3.8 cycles among mothers who had no difficulties; and 2. mothers with breastfeeding difficulties received their first cycle of chemotherapy on average 3.4 weeks earlier in pregnancy. Of the 9 women who received a taxane-containing regimen, 7 had breastfeeding difficulties.[9]
References
- 1.
- Pistilli B, Bellettini G, Giovannetti E, et al. Chemotherapy, targeted agents, antiemetics and growth-factors in human milk: How should we counsel cancer patients about breastfeeding? Cancer Treat Rev 2013;39:207-11. [PubMed: 23199900]
- 2.
- Johnson HM, Mitchell KB. ABM clinical protocol #34: Breast cancer and breastfeeding. Breastfeed Med 2020;15:429-34. [PubMed: 32516007]
- 3.
- Damoiseaux D, Amant F, Beijnen JH, et al. Physiologically-based pharmacokinetic model to predict doxorubicin and paclitaxel exposure in infants through breast milk. CPT Pharmacometrics Syst Pharmacol 2023;12:1931-44. [PMC free article: PMC10725259] [PubMed: 37798909]
- 4.
- Urbaniak C, McMillan A, Angelini M, et al. Effect of chemotherapy on the microbiota and metabolome of human milk, a case report. Microbiome 2014;2:24. [PMC free article: PMC4109383] [PubMed: 25061513]
- 5.
- Griffin SJ, Milla M, Baker TE, et al. Transfer of carboplatin and paclitaxel into breast milk. J Hum Lact 2012;28:457-9. [PubMed: 23087196]
- 6.
- Jackson CGCA, Morris T, Hung N, Hung T. Breast milk paclitaxel excretion following intravenous chemotherapy-a case report. Br J Cancer 2019;121:421-4. [PMC free article: PMC6738114] [PubMed: 31363168]
- 7.
- Damoiseaux D, Calpe S, Rosing H, et al. Presence of 5 chemotherapeutic drugs in breast milk as a guide for the safe use of chemotherapy during breastfeeding: Results from a case series. Clin Pharmacol Ther 2022;112:404-10. [PubMed: 35486426]
- 8.
- Damoiseaux D, Centanni D, Beijnen JH, et al. Predicting chemotherapy distribution into breast milk for breastfeeding women using a population pharmacokinetic approach. Clin Pharmacokinet 2023;62:969-80. [PMC free article: PMC10338611] [PubMed: 37154994]
- 9.
- Stopenski S, Aslam A, Zhang X, Cardonick E. After chemotherapy treatment for maternal cancer during pregnancy, is breastfeeding possible? Breastfeed Med 2017;12:91-7. [PubMed: 28170295]
Substance Identification
Substance Name
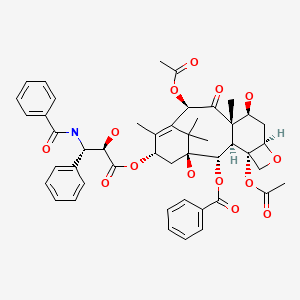
Paclitaxel
CAS Registry Number
33069-62-4
Drug Class
Breast Feeding
Milk, Human
Antineoplastic Agents, Phytogenic
Antimitotic Agents
Tubulin Modulators
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Docetaxel.[Drugs and Lactation Database (...]Review Docetaxel.. Drugs and Lactation Database (LactMed®). 2006
- Review Vinblastine.[Drugs and Lactation Database (...]Review Vinblastine.. Drugs and Lactation Database (LactMed®). 2006
- Review Vinorelbine.[Drugs and Lactation Database (...]Review Vinorelbine.. Drugs and Lactation Database (LactMed®). 2006
- New antibiotics SF2315A and B produced by an Excellospora sp. II. The structural elucidation.[J Antibiot (Tokyo). 1988]New antibiotics SF2315A and B produced by an Excellospora sp. II. The structural elucidation.Sasaki T, Gomi S, Sezaki M, Takeuchi Y, Kodama Y, Kawamura K. J Antibiot (Tokyo). 1988 Jul; 41(7):843-8.
- Review Doxorubicin.[Drugs and Lactation Database (...]Review Doxorubicin.. Drugs and Lactation Database (LactMed®). 2006
- Paclitaxel - Drugs and Lactation Database (LactMed®)Paclitaxel - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
