Introduction
The femoral sheath is a fascial tube encapsulating the key vascular structures passing through the retro-inguinal space, a critical transition point between the abdomen and the anterior thigh compartment. It is an important anatomical landmark for understanding the structures in the femoral triangle within which it lies and has clinical importance as the site of femoral hernias.[1]
Structure and Function
The inguinal ligament spans the gap between the anterior superior iliac spine and the pubic tubercle. Beneath it, the retro-inguinal space is created and is divided by the iliopectineal arch into a muscular compartment and a vascular compartment. The femoral sheath lines the vascular compartment of the retro-inguinal space, which contains the femoral artery, femoral vein, and deep inguinal lymph nodes.[2]
The femoral sheath has a conical shape and is of varying length, typically 3 to 4 cm, before it blends with the adventitia of the femoral vessels. Its anterior aspect is a continuation of the transversalis fascia, whereas the posterior aspect is formed from a continuation of the iliopsoas fascia.[3]
Anteriorly, the femoral sheath is covered by the fascia lata of the thigh, and posteriorly it is related to the underlying iliacus and pectineus muscles. The femoral sheath is bordered medially by the lacunar ligament, and on its lateral side lies the femoral nerve.
The femoral sheath is divided into three compartments by vertical septa of connective tissue that separate it into distinct functional areas:
- Lateral compartment – containing the femoral artery
- Intermediate compartment – containing the femoral vein
- Medial compartment – called the femoral canal, containing loose connective tissue and lymph nodes[4]
The function of the femoral canal (medial compartment of the femoral sheath) is to allow expansion of the femoral vein into this space following increased venous return.[5] The superior opening of the femoral canal under the inguinal ligament is termed the femoral ring. The borders of the femoral ring are:
- Anteriorly: the inguinal ligament
- Medially: the lacunar ligament
- Laterally: the septum between the femoral canal and the intermediate compartment of the femoral sheath
- Posteriorly: Pectineus muscle[3]
The ‘mouth’ of the femoral ring is covered transversely by a sheet of peritoneal fatty tissue termed the femoral septum; this area is weak and abdominal viscera can traverse through it into the femoral canal, causing a femoral hernia.[2][4]
The general function of the femoral sheath is to allow the femoral vascular structures to glide underneath the inguinal ligament during hip flexion and extension. It provides a smooth fascial layer to facilitate this.
Embryology
The femoral sheath is a fascial structure formed anteriorly by a continuation of the transversalis fascia and posteriorly by a continuation of the iliopsoas fascia. Both of these fascia layers are part of the thoracolumbar fascia, which is key to maintaining posture and the transmission of force between the scapular and pelvic girdles.[6] The embryological origin of the fascial layers of the body is intimately associated with the development of their corresponding muscular structures. Somitogenesis begins on the twentieth day of the embryo, forming somites from the segmentation of the paraxial mesoderm.[7] The dermomyotome is one of the constituent parts of the resulting somite, alongside the sclerotome. Further differentiation of the dermomyotome forms the dermis of the skin, as well as the epaxial and the hypaxial muscle compartments, the latter of which include the ventrolateral muscles of the abdominal wall.[8]
Blood Supply and Lymphatics
The femoral artery travels in the lateral compartment of the femoral sheath. It is a continuation of the external iliac artery, commencing as it passes under the inguinal ligament.[9] Distally, the femoral artery passes into the adductor canal, becoming the popliteal artery as it passes through the adductor hiatus. It gives off several important branches, none of which arise within the femoral sheath itself.
The femoral vein occupies the intermediate compartment of the femoral sheath. It is a continuation of the popliteal vein and enters the femoral sheath before becoming the external iliac vein as it passes under the inguinal ligament.
The femoral canal contains deep inguinal lymph nodes and associated lymphatic vessels.[10] The superior-most lymph node is termed the node of Cloquet.[11] These lymph nodes drain the glans clitoris in females, and the glans penis and the distal part of the spongy urethra in males.
Nerves
The femoral branch of the genitofemoral nerve (from L1-L2) is given off as it lies on psoas major. It then runs inferiorly under the inguinal ligament, accompanying the femoral artery in the lateral compartment of the femoral sheath, before piercing it anteriorly to innervate the skin over the femoral triangle.[12][13]
The femoral nerve proper (from L2-L4) travels in the muscular compartment of the retro-inguinal space, lateral to the vascular compartment lined by the femoral sheath.[14] Thus, although an important part of the femoral triangle anatomy, it does not form part of the femoral sheath.
Muscles
Behind the femoral sheath are the pectineus muscle (posteromedial) and the iliopsoas muscle (posterolateral).[2] The origin of the pectineus muscle is the pectineal line of the pubis, and its distal insertion point is the pectineal line of the femur, which is a continuation from the inferior part of the lesser trochanter. The iliopsoas muscle is a congruence of two posterior abdominal wall muscles; the iliacus, which arises from the iliac fossa, and the psoas major, which arises from the transverse processes of lumbar vertebrae L1-L5. Together, as the iliopsoas muscle, it inserts at the lesser trochanter of the femur. There is no muscular covering anteriorly over the femoral sheath; instead, it is covered by the fascia lata and cribriform fascia, subcutaneous tissue, and skin.
Surgical Considerations
The medial part of the femoral sheath, termed the femoral canal, is the site through which abdominal viscera can protrude, resulting in a femoral hernia. Femoral hernia repair can be performed with mesh (hernioplasty) or primary suture closure (herniorrhaphy). Modern practice internationally has favored mesh repair, either via an open approach or laparoscopically, in the elective setting for both male and female groin hernia repair.[15][1] However, controversy remains as to the best management for femoral hernias.[16][17][18][19] This is because they are far less common than inguinal hernias, and there is a lack of long-term outcome data from the various repair techniques.[20]
The three classic open approaches to repair of femoral hernia are the infra-inguinal (Lockwood) approach, the trans-inguinal (Lotheissen) approach, and the high (McEvedy) approach, with each offering advantages in certain situations. The Lockwood approach, for example, involves a parallel incision approximately 1cm below the inguinal ligament and is suitable for elective repair as there is little opportunity to allow for bowel resection if required in emergency surgery[21]. Contemporary surgical practice has moved towards the laparoscopic approach for elective repair of femoral hernia, however, with classic open approaches increasingly being superseded. Indeed, the laparoscopic approach is increasingly recognized also as an option for emergency repair.[22]
The two laparoscopic surgical techniques for groin hernias are the transabdominal preperitoneal (TAPP) and the totally intraperitoneal (TEP) approach.[23] In the former, the peritoneal cavity is entered, and an incision is made pre-peritoneally to enable repair of the herniated site, whereas, in TEP, the peritoneum remains intact, and repair is performed without entering the cavity[24]. Current evidence involving a meta-analysis of 15 randomized-control trials suggests the recurrence rate and long-term outcomes of the two techniques are comparable.[25]
Clinical Significance
Femoral Hernia
Femoral hernias are the least common kind of groin hernia, accounting for between 20% and 31% of groin repairs in women and only 1% of groin repairs in men.[26] There is a strong preponderance towards women, with one study identifying 88% of femoral hernias as presenting in women, and the average age of presentation is typically in the 6th to 7th decade.[27] However, they may be underdiagnosed, particularly in patients with a high body-mass index (BMI); one study reported that 37% of women undergoing endoscopic inguinal hernia repair were found to have a synchronous undiagnosed femoral hernia.[28]
The typical clinical presentation of femoral hernia is a swelling inferior to the inguinal ligament and inferior and lateral to the pubic tubercle.[1] The risk of strangulation in femoral hernia is higher than for inguinal hernia.[26] Incarcerated bowel within a strangulated femoral hernia may present with severe pain and an acute bowel obstruction requiring emergent surgical intervention, and this is associated with worse outcomes than in patients managed electively.[29][30]
Femoral Vascular Access
The femoral vein is a relatively safe option for gaining central venous access when more proximal locations are less easily accessible. Ultrasound guidance helps reduce vascular bleeding by 60% when used for femoral vein cannulation.[31][32] The femoral artery is also a commonly used site of arterial access, both for obtaining blood in emergency situations and diagnostic procedures, such as digital subtraction angiography in neurosurgery.[33][34]
Node of Cloquet
The node of Cloquet, which lies within the medial compartment of the femoral sheath (otherwise known as the femoral canal), is the junctional point between the external iliac lymph chain and the deep inguinal nodes.[35] As such, it is the sentinel node for the iliac and obturator lymphatic system. Studies investigating the predictive value of metastatic deposits in Cloquet's node for deep pelvic malignancy have shown a positive predictive value of 70% and a negative predictive value of 84%.[11] This means that the decision on whether to perform deep pelvic lymphadenectomy can potentially be made based on a sentinel node biopsy of the node of Cloquet.[11] A further study found the pathological status of Cloquet's node to be superior to the radiological diagnosis when determining the appropriate extent of lymph node dissection that should be undertaken in patients with lower limb melanoma and palpable inguinal lymphadenopathy.[36]

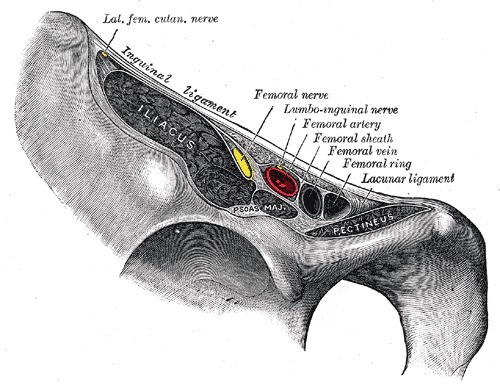
Figure
Vascular Lacuna, Femoral Nerve, Ilioinguinal nerve, Femoral sheath, Femoral artery, Femoral vein and ring Henry Vandyke Carter, Public Domain, via Wikimedia Commons

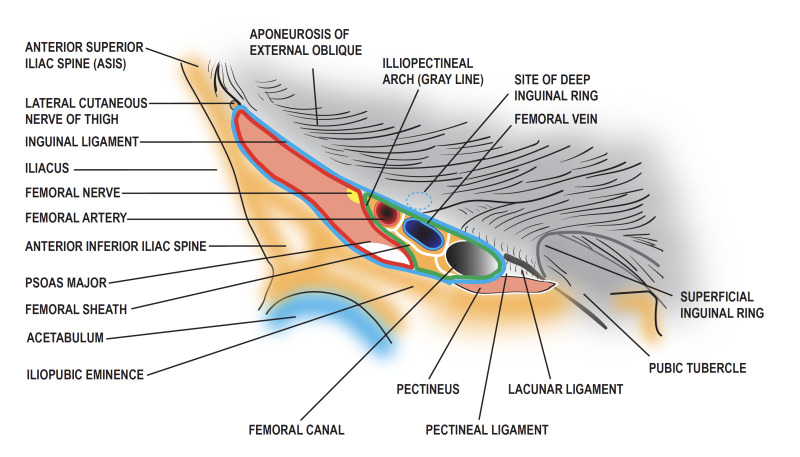
Figure
Genitofemoral Nerve. The genitofemoral nerve arises from the lumbar plexus and supplies sensation to the thigh and genitalia. Illustration by E Gregory

Figure
Diagram of the femoral sheath and its contents. Contributed by Penney Dellavalle

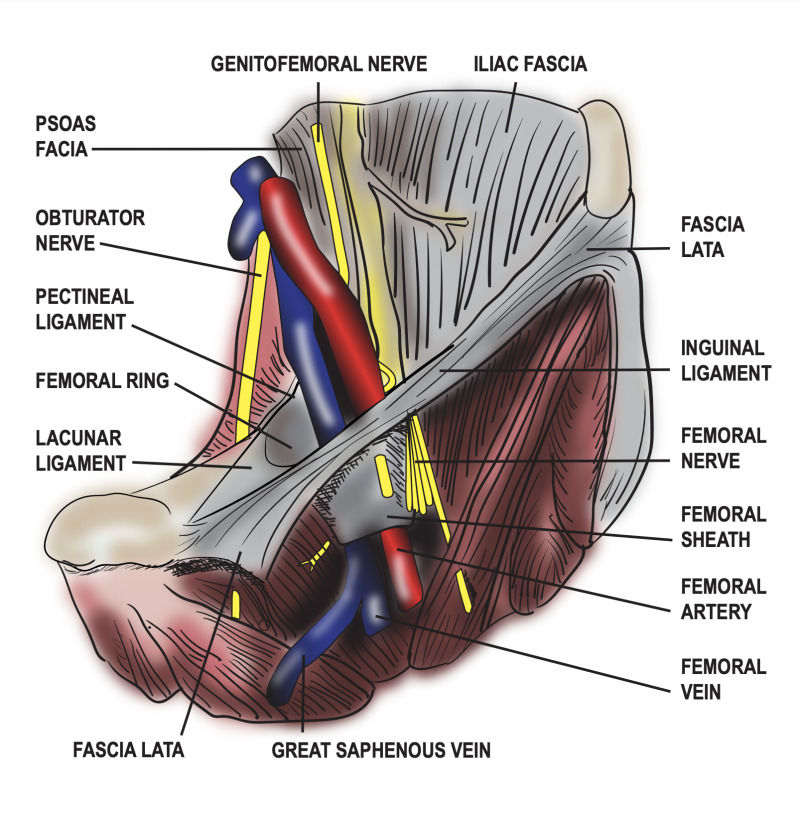
Figure
Diagram of the femoral sheath and its contents. Contributed by Penney Dellavalle.
References
- 1.
- HerniaSurge Group. International guidelines for groin hernia management. Hernia. 2018 Feb;22(1):1-165. [PMC free article: PMC5809582] [PubMed: 29330835]
- 2.
- Lytle WJ. Inguinal anatomy. J Anat. 1979 May;128(Pt 3):581-94. [PMC free article: PMC1232909] [PubMed: 468709]
- 3.
- Yoshida S, Nakagomi K, Goto S. Abscess formation in the prevesical space and bilateral thigh muscles secondary to osteomyelitis of the pubis--basis of the anatomy between the prevesical space and femoral sheath. Scand J Urol Nephrol. 2004;38(5):440-1. [PubMed: 15764260]
- 4.
- Totté E, Van Hee R, Kox G, Hendrickx L, van Zwieten KJ. Surgical anatomy of the inguinal region: implications during inguinal laparoscopic herniorrhaphy. Eur Surg Res. 2005 May-Jun;37(3):185-90. [PubMed: 16088185]
- 5.
- Benjamin M. The fascia of the limbs and back--a review. J Anat. 2009 Jan;214(1):1-18. [PMC free article: PMC2667913] [PubMed: 19166469]
- 6.
- Gatton ML, Pearcy MJ, Pettet GJ, Evans JH. A three-dimensional mathematical model of the thoracolumbar fascia and an estimate of its biomechanical effect. J Biomech. 2010 Oct 19;43(14):2792-7. [PubMed: 20709320]
- 7.
- Vieira L. Embryology of the Fascial System. Cureus. 2020 Aug 30;12(8):e10134. [PMC free article: PMC7524024] [PubMed: 33005546]
- 8.
- Willard FH, Vleeming A, Schuenke MD, Danneels L, Schleip R. The thoracolumbar fascia: anatomy, function and clinical considerations. J Anat. 2012 Dec;221(6):507-36. [PMC free article: PMC3512278] [PubMed: 22630613]
- 9.
- Kaki A, Blank N, Alraies MC, Kajy M, Grines CL, Hasan R, Htun WW, Glazier J, Mohamad T, Elder M, Schreiber T. Access and closure management of large bore femoral arterial access. J Interv Cardiol. 2018 Dec;31(6):969-977. [PubMed: 30456854]
- 10.
- Scaglioni MF, Suami H. Lymphatic anatomy of the inguinal region in aid of vascularized lymph node flap harvesting. J Plast Reconstr Aesthet Surg. 2015 Mar;68(3):419-27. [PubMed: 25465766]
- 11.
- Shen P, Conforti AM, Essner R, Cochran AJ, Turner RR, Morton DL. Is the node of Cloquet the sentinel node for the iliac/obturator node group? Cancer J. 2000 Mar-Apr;6(2):93-7. [PubMed: 11069226]
- 12.
- Cesmebasi A, Yadav A, Gielecki J, Tubbs RS, Loukas M. Genitofemoral neuralgia: a review. Clin Anat. 2015 Jan;28(1):128-35. [PubMed: 25377757]
- 13.
- Iwanaga J, Simonds E, Schumacher M, Kikuta S, Watanabe K, Tubbs RS. Revisiting the genital and femoral branches of the genitofemoral nerve: Suggestion for a more accurate terminology. Clin Anat. 2019 Apr;32(3):458-463. [PubMed: 30592097]
- 14.
- Lonchena TK, McFadden K, Orebaugh SL. Correlation of ultrasound appearance, gross anatomy, and histology of the femoral nerve at the femoral triangle. Surg Radiol Anat. 2016 Jan;38(1):115-22. [PubMed: 25821034]
- 15.
- Rosenberg J, Bisgaard T, Kehlet H, Wara P, Asmussen T, Juul P, Strand L, Andersen FH, Bay-Nielsen M., Danish Hernia Database. Danish Hernia Database recommendations for the management of inguinal and femoral hernia in adults. Dan Med Bull. 2011 Feb;58(2):C4243. [PubMed: 21299930]
- 16.
- Clyde DR, de Beaux A, Tulloh B, O'Neill JR. Minimising recurrence after primary femoral hernia repair; is mesh mandatory? Hernia. 2020 Feb;24(1):137-142. [PubMed: 31407108]
- 17.
- Chen J, Lv Y, Shen Y, Liu S, Wang M. A prospective comparison of preperitoneal tension-free open herniorrhaphy with mesh plug herniorrhaphy for the treatment of femoral hernias. Surgery. 2010 Nov;148(5):976-81. [PubMed: 20356615]
- 18.
- Ceriani V, Faleschini E, Sarli D, Lodi T, Roncaglia O, Bignami P, Osio C, Somalvico F. Femoral hernia repair. Kugel retroparietal approach versus plug alloplasty: a prospective study. Hernia. 2006 Apr;10(2):169-74. [PubMed: 16482402]
- 19.
- Kang JS, Qiao F, Nie L, Wang Y, He SW, Wu B. Preperitoneal femoral hernioplasty: an "umbrella" technique. Hernia. 2015 Oct;19(5):805-8. [PubMed: 24927966]
- 20.
- Chan G, Chan CK. Longterm results of a prospective study of 225 femoral hernia repairs: indications for tissue and mesh repair. J Am Coll Surg. 2008 Sep;207(3):360-7. [PubMed: 18722941]
- 21.
- Sorelli PG, El-Masry NS, Garrett WV. Open femoral hernia repair: one skin incision for all. World J Emerg Surg. 2009 Nov 30;4:44. [PMC free article: PMC2789711] [PubMed: 19948016]
- 22.
- Okazaki R, Poudel S, Hane Y, Saito T, Muto J, Syoji Y, Hase R, Senmaru N, Hirano S. Laparoscopic approach as a safe and effective option for incarcerated femoral hernias. Asian J Endosc Surg. 2022 Apr;15(2):328-334. [PubMed: 34749433]
- 23.
- Peitsch WK. A modified laparoscopic hernioplasty (TAPP) is the standard procedure for inguinal and femoral hernias: a retrospective 17-year analysis with 1,123 hernia repairs. Surg Endosc. 2014 Feb;28(2):671-82. [PubMed: 24043647]
- 24.
- Aiolfi A, Cavalli M, Ferraro SD, Manfredini L, Bonitta G, Bruni PG, Bona D, Campanelli G. Treatment of Inguinal Hernia: Systematic Review and Updated Network Meta-analysis of Randomized Controlled Trials. Ann Surg. 2021 Dec 01;274(6):954-961. [PubMed: 33427757]
- 25.
- Aiolfi A, Cavalli M, Del Ferraro S, Manfredini L, Lombardo F, Bonitta G, Bruni PG, Panizzo V, Campanelli G, Bona D. Total extraperitoneal (TEP) versus laparoscopic transabdominal preperitoneal (TAPP) hernioplasty: systematic review and trial sequential analysis of randomized controlled trials. Hernia. 2021 Oct;25(5):1147-1157. [PMC free article: PMC8514389] [PubMed: 33851270]
- 26.
- Lockhart K, Dunn D, Teo S, Ng JY, Dhillon M, Teo E, van Driel ML. Mesh versus non-mesh for inguinal and femoral hernia repair. Cochrane Database Syst Rev. 2018 Sep 13;9(9):CD011517. [PMC free article: PMC6513260] [PubMed: 30209805]
- 27.
- Kunduz E, Sormaz İC, Yapalak Y, Bektasoglu HK, Gok AF. Comparison of surgical techniques and results for emergency or elective femoral hernia repair. Ulus Travma Acil Cerrahi Derg. 2019 Nov;25(6):611-615. [PubMed: 31701494]
- 28.
- Putnis S, Wong A, Berney C. Synchronous femoral hernias diagnosed during endoscopic inguinal hernia repair. Surg Endosc. 2011 Dec;25(12):3752-4. [PubMed: 21638171]
- 29.
- Alhambra-Rodriguez de Guzmán C, Picazo-Yeste J, Tenías-Burillo JM, Moreno-Sanz C. Improved outcomes of incarcerated femoral hernia: a multivariate analysis of predictive factors of bowel ischemia and potential impact on postoperative complications. Am J Surg. 2013 Feb;205(2):188-93. [PubMed: 23021195]
- 30.
- Humes DJ, Radcliffe RS, Camm C, West J. Population-based study of presentation and adverse outcomes after femoral hernia surgery. Br J Surg. 2013 Dec;100(13):1827-32. [PubMed: 24227371]
- 31.
- Wiles BM, Child N, Roberts PR. How to achieve ultrasound-guided femoral venous access: the new standard of care in the electrophysiology laboratory. J Interv Card Electrophysiol. 2017 Jun;49(1):3-9. [PubMed: 28168447]
- 32.
- Powell JT, Mink JT, Nomura JT, Levine BJ, Jasani N, Nichols WL, Reed J, Sierzenski PR. Ultrasound-guidance can reduce adverse events during femoral central venous cannulation. J Emerg Med. 2014 Apr;46(4):519-24. [PubMed: 24462032]
- 33.
- Khan Z, Nattanamai P, Keerthivaas P, Newey CR. An Evaluation of Complications in Femoral Arterial Sheaths Maintained Post-Neuroangiographic Procedures. Cureus. 2018 Feb 26;10(2):e2230. [PMC free article: PMC5919764] [PubMed: 29713575]
- 34.
- Bhatia K, Guest W, Lee H, Klostranec J, Kortman H, Orru E, Qureshi A, Kostynskyy A, Agid R, Farb R, Radovanovic I, Nicholson P, Krings T, Pereira VM. Radial vs. Femoral Artery Access for Procedural Success in Diagnostic Cerebral Angiography : A Randomized Clinical Trial. Clin Neuroradiol. 2021 Dec;31(4):1083-1091. [PubMed: 33373017]
- 35.
- Plata Bello A, Apatov SE, Benfante NE, Rivero Belenchón I, Picola Brau N, Mercader Barrull C, Jenjitranant P, Vickers AJ, Fine SW, Touijer KA. Prevalence of High-Risk Prostate Cancer Metastasis to Cloquet's Ilioinguinal Lymph Node. J Urol. 2022 Jun;207(6):1222-1226. [PMC free article: PMC9912356] [PubMed: 35050701]
- 36.
- Koh YX, Chok AY, Zheng H, Xu S, Teo MC. Cloquet's node trumps imaging modalities in the prediction of pelvic nodal involvement in patients with lower limb melanomas in Asian patients with palpable groin nodes. Eur J Surg Oncol. 2014 Oct;40(10):1263-70. [PubMed: 24947073]
Disclosure: Navid Mahabadi declares no relevant financial relationships with ineligible companies.
Disclosure: Valerie Lew declares no relevant financial relationships with ineligible companies.
Disclosure: Michael Kang declares no relevant financial relationships with ineligible companies.
Publication Details
Author Information and Affiliations
Authors
Navid Mahabadi1; Valerie Lew2; Michael Kang3.Affiliations
Publication History
Last Update: April 11, 2023.
Copyright
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
Publisher
StatPearls Publishing, Treasure Island (FL)
NLM Citation
Mahabadi N, Lew V, Kang M. Anatomy, Abdomen and Pelvis: Femoral Sheath. [Updated 2023 Apr 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.