Continuing Education Activity
Gallstones or cholelithiasis are stones that form in the gallbladder composed of cholesterol, bilirubin, and bile. These stones are asymptomatic in most cases, with stones discovered incidentally. Symptomatic patients present with right upper abdominal pain after eating greasy or spicy food, nausea, vomiting, pain in epigastrium that radiates to the right scapula or mid-back. This activity illustrates the evaluation and management of gallstones and reviews the role of the interprofessional team in improving care for patients with this condition.
Objectives:
- Identify the risk factors associated with the development of gallstones.
- Describe the pathophysiology of gallstones.
- Outline the use of a right upper quadrant abdominal ultrasound in the evaluation of gallstones.
- Explain the importance of improving care coordination among the interprofessional team members to improve outcomes for patients affected by gallstones.
Introduction
Gallstones or cholelithiasis are responsible for one of the most prevalent digestive disorders in the United States. They are considered a disease of developed populations but are present around the world. It is both the result of a chronic disease process and the cause of subsequent acute disorders of the pancreatic, biliary, hepatic, and gastrointestinal tract. Over 6.3 million females and 14.2 million males in the United States between the ages of 20 and 74 have gallstones. Most patients with gallstones are asymptomatic, but 10% of patients will develop symptoms within five years, and 20% of patients will develop symptoms within 20 years of diagnosing gallstones. Gallstone prevalence also increases with age. Over one-quarter of females older than the age of 60 will have gallstones. Gallstones have various compositions and etiologies.[1]
The critical feature of gallstones is that they are not all symptomatic. Sometimes they may migrate near the opening of the cystic duct and block the flow of bile. This can lead to tension in the gallbladder, which results in the classic biliary colicky pain. If the cystic duct is obstructed for more than a few hours, it can lead to inflammation of the gallbladder wall (cholecystitis). Sometimes the gallstone may move into the bile duct and cause obstruction, leading to jaundice and abdominal pain. Patients who have chronic gallstones may develop progressive fibrosis and loss of motor function of the gallbladder. The best test to make a diagnosis of gallstones is ultrasound. The treatment of gallstones depends on symptoms. The standard of care for symptomatic patients is laparoscopic cholecystectomy.
Etiology
Gallstones usually form from sluggishly emptying of bile from the gallbladder. When bile is not fully drained from the gallbladder, it can precipitate as sludge, which in turn can develop into gallstones. Biliary obstruction from various causes such as strictures in the bile duct or neoplasms may also lead to gallstones. The most common cause of cholelithiasis is the precipitation of cholesterol from cholesterol-rich bile. The second most common form of gallstones is pigmented gallstones. These form from the breakdown of red blood cells and are black. The third type of gallstones is mixed pigmented stones, a combination of calcium substrates such as calcium carbonate or calcium phosphate, cholesterol, and bile. The fourth type of stone is calcium stones. These may be due to the precipitation of serum calcium in patients with hypercalcemia. Often these patients will have concurrent kidney stones.[2]
Risk factors for gallstones include:
- In pregnancy, progesterone decreases the contractility of the gallbladder leading to stasis.
- Obesity
- Genes
- Certain medications (estrogens, fibrates, somatostatin analogs)
- Stasis of the gallbladder
- Female gender
- Metabolic syndrome
- Rapid weight loss
- Prolonged fasting
- Bariatric surgery
- Crohn disease, ileal resection
Epidemiology
Most gallstones are asymptomatic. In the United States, approximately 14 million women and 6 million men with an age range of 20 to 74 have gallstones. The prevalence increases as a person ages. Obesity increases the likelihood of gallstones, especially in women, due to increases in the biliary secretion of cholesterol. On the other hand, patients with drastic weight loss or fasting have a higher chance of gallstones secondary to biliary stasis. Furthermore, there is also a hormonal association with gallstones. Estrogen has been shown to result in an increase in bile cholesterol as well as a decrease in gallbladder contractility. Women of reproductive age or on estrogen-containing birth control medication have a two-fold increase in gallstone formation compared to males. People with chronic illnesses such as diabetes also have an increase in gallstone formation and reduced gallbladder wall contractility due to neuropathy.[3]
Pathophysiology
Gallstones occur when substances in the bile reach their limits of solubility. As bile becomes concentrated in the gallbladder, it becomes supersaturated with these substances, which in time precipitate into small crystals. These crystals, in turn, become stuck in the gallbladder mucus, resulting in gallbladder sludge. Over time, these crystals grow and form large stones. Complications caused by gallstones are a direct consequence of occlusion of the hepatic and biliary tree by sludge and stones.[3]
There are two types of gallstones, cholesterol and calcium bilirubinate.
Cholesterol gallstones form the majority of gallstones. The major component of these stones is cholesterol. The bilirubinate stones contain bilirubin. In patients with a high turnover of heme, such as cirrhosis or chronic hemolysis, the unconjugated bilirubin will crystallize and eventually form stones. These stones are usually dark black or blue and account for about 15% of gallstones in the United States.
Sometimes, the cholesterol gallstones will become colonized with microorganisms, which leads to inflammation of the mucosa. The resulting leucocyte infiltration and presence of bilirubin leads to mixed stones.
Histopathology
Pathologists can analyze the composition of gallstones and bile, which may help to determine the cause of the stones, especially in cases of primary common bile duct stones, after gallbladder removal and the exact cause of the stones is unknown.[4][5]
History and Physical
Usually, patients with symptoms from gallstones present with right upper abdominal pain after eating greasy or spicy foods. There is often nausea and vomiting. Pain can also be present in the epigastric area that radiates to the right scapula or mid-back. The classic physical exam finding is a positive Murphy's sign, where the pain is elicited on deep palpation to the right upper quadrant underneath the rib cage upon deep inspiration. Patients may be asymptomatic for months to years until the discovery of gallstones. Acute cholecystitis presents similarly. However, it is more severe. Jaundice can be a sign of a common bile duct obstruction from an entrapped gallstone. In the presence of jaundice and abdominal pain, often, a procedure is an indication to go and retrieve the stone to prevent further sequelae. One such sequela is ascending cholangitis, with symptoms of right upper abdominal pain, fever, and jaundice (Charcot's triad). Progression of this condition is indicated by neurologic changes and hypotension (Reynold's pentad). Other sequelae are acute pancreatitis with symptoms of mid-epigastric pain and intractable vomiting.[6]
Evaluation
The best diagnostic test for diagnosing gallstones and subsequent acute cholecystitis is a right upper quadrant abdominal ultrasound. It is associated with a 90% specificity rate and, depending on the ultrasound operator, can detect stones as small as 2 mm as well as sludge and gallbladder polyps. Ultrasound findings that point towards acute cholecystitis versus cholelithiasis include gallbladder wall thickening greater than 3 mm, pericholecystic fluid, and a positive sonographic Murphy's sign. Gallstones can also often be present on CT scans and MRIs. However, these tests are not as sensitive for diagnosing acute cholecystitis. Approximately 10% of gallstones may be found on routine plain films due to their high calcium content. If there is a suspected stone in the common bile duct based on ultrasound results, magnetic resonance cholangiopancreatography (MRCP) is the next step. If a common duct stone is identified on the MRCP, then the gold-standard test of an endoscopic retrograde cholangiopancreatogram (ERCP) should be performed by a gastroenterologist. A percutaneous transhepatic cholangiogram (PTHC) is also useful in diagnosing common bile duct stones if an ERCP is not possible.[7]
Treatment / Management
Cholecystectomy treats symptomatic gallstones. The laparoscopic approach is the standard of care. Open cholecystectomies are the option when it is not practical or advisable to do a laparoscopic procedure. It is not wise to only remove the gallstones as studies have shown that they recur after about one year. In cases of acute cholecystitis in critically ill patients or patients who are poor surgical candidates, a decompression cholecystostomy tube can be placed to temporize the patient until stable enough for definitive surgery. Common bile duct stones can be removed with a preoperative or postoperative ERCP, PTHC, or operatively with a common bile duct exploration. Ascending cholangitis needs to be addressed urgently by removing the blockage either with ERCP, PTHC, or surgery, as well as early antibiotic administration. In cases of nonacute cholecystitis and very poor surgical candidates, gallstones can be treated medically. Ursodiol is administered daily with the hope of dissolving the gallstones and has shown mixed success with some studies at best, showing less than a 50% response rate.[8]
Differential Diagnosis
- Appendicitis
- Renal calculi
- Cholangiocarcinoma
- Bile duct stones
- Acute pancreatitis
- Peptic ulcer disease
Prognosis
Less than 50% of patients who have gallstones will develop symptoms. Today, the mortality rate following laparoscopic cholecystectomy is less than 1%; however, emergency cholecystectomy rates are 10% or greater. Other complications include retained stones in the bile duct, incisional hernia, and chronic right upper quadrant pain. Despite the fact that laparoscopic cholecystectomy is now the standard of care for symptomatic gallstones, the rates of injury to the bile duct during surgery continue to increase.
Complications
Complications from gallstones may include [9][10]:
- Gallbladder inflammation leading to cholecystitis
- Common bile duct blockage resulting in bile duct infection and jaundice
- Pancreatic duct blockage which can cause pancreatitis
- Cancer of the gallbladder
Deterrence and Patient Education
Patient education centers around maintaining a low-fat diet, medication adherence, explaining the pathophysiology of the condition, follow-up appointments to track progress, and explaining potential surgical interventions if they become necessary.
Enhancing Healthcare Team Outcomes
Gallbladder disease can be a difficult diagnosis. Early suspicion with proper testing will make the diagnosis. The condition is best managed by an interprofessional team. Having a skilled radiologist and emergency physician will often be the critical first step in properly diagnosing gallstones. Early intervention by an experienced surgeon is also vital. Practitioners should remember that not all gallstones will require surgery. The correct clinical decision must be made as a group recommendation between the primary care physician, nurse practitioner, radiologist, gastroenterologist, the patient, and the surgeon. The primary care clinicians should encourage patients to eat a healthy diet, maintain healthy body weight, eat a low-fat diet, and abstain from prolonged fasting. Nurses monitor patients perioperatively, educate patients and their families, and inform the team of changes in patient status. Close communication between the team members if vital to lower the morbidity of gallstones.[11][12][13]

Figure
Gallstone on Point-of-Care Ultrasound Contributed by Emory Emergency Medicine Ultrasound Section

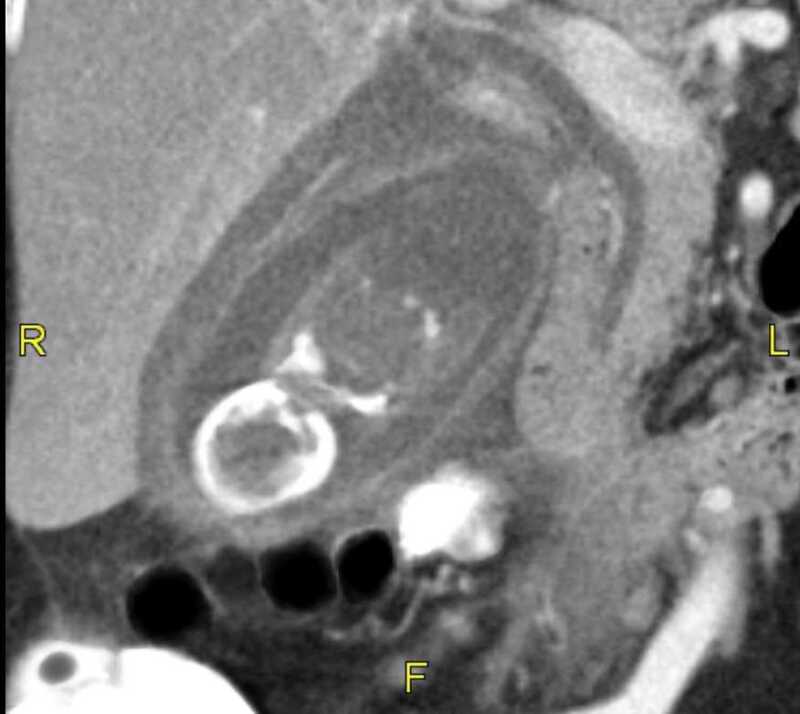
Figure
CT Acute Cholecystitis Wall Thickening Pericholecystic Fluid Gallstone Contributed by Scott Dulebohn, MD
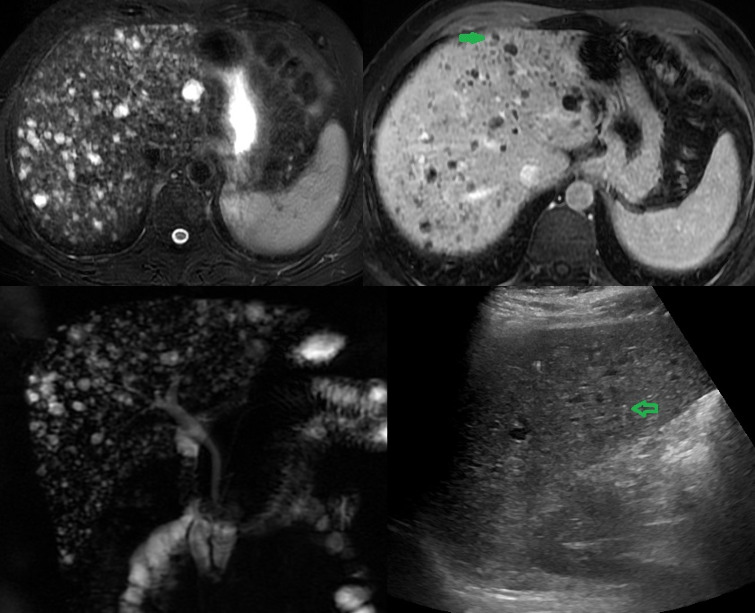
Figure
Gallstones in a female Image courtesy S Bhimji
Figure
Gallbladder Gallstones (Calculi), Common bile duct, Pancreas, Intestine, Gallbladder, Gallstones, Liver Illustration by Emma Gregory
References
- 1.
- Tsai TJ, Chan HH, Lai KH, Shih CA, Kao SS, Sun WC, Wang EM, Tsai WL, Lin KH, Yu HC, Chen WC, Wang HM, Tsay FW, Lin HS, Cheng JS, Hsu PI. Gallbladder function predicts subsequent biliary complications in patients with common bile duct stones after endoscopic treatment? BMC Gastroenterol. 2018 Feb 27;18(1):32. [PMC free article: PMC6389262] [PubMed: 29486713]
- 2.
- Rebholz C, Krawczyk M, Lammert F. Genetics of gallstone disease. Eur J Clin Invest. 2018 Jul;48(7):e12935. [PubMed: 29635711]
- 3.
- Shabanzadeh DM. New determinants for gallstone disease? . Dan Med J. 2018 Feb;65(2) [PubMed: 29393043]
- 4.
- Del Pozo R, Mardones L, Villagrán M, Muñoz K, Roa S, Rozas F, Ormazábal V, Muñoz M. [Effect of a high-fat diet on cholesterol gallstone formation]. Rev Med Chil. 2017 Sep;145(9):1099-1105. [PubMed: 29424395]
- 5.
- Charfi S, Gouiaa N, Mnif H, Chtourou L, Tahri N, Abid B, Mzali R, Boudawara TS. Histopathological findings in cholecystectomies specimens: A single institution study of 20 584 cases. Hepatobiliary Pancreat Dis Int. 2018 Aug;17(4):345-348. [PubMed: 30173787]
- 6.
- Wilkins T, Agabin E, Varghese J, Talukder A. Gallbladder Dysfunction: Cholecystitis, Choledocholithiasis, Cholangitis, and Biliary Dyskinesia. Prim Care. 2017 Dec;44(4):575-597. [PubMed: 29132521]
- 7.
- Hiwatashi K, Okumura H, Setoyama T, Ando K, Ogura Y, Aridome K, Maenohara S, Natsugoe S. Evaluation of laparoscopic cholecystectomy using indocyanine green cholangiography including cholecystitis: A retrospective study. Medicine (Baltimore). 2018 Jul;97(30):e11654. [PMC free article: PMC6078678] [PubMed: 30045318]
- 8.
- Hirajima S, Koh T, Sakai T, Imamura T, Kato S, Nishimura Y, Soga K, Nishio M, Oguro A, Nakagawa N. Utility of Laparoscopic Subtotal Cholecystectomy with or without Cystic Duct Ligation for Severe Cholecystitis. Am Surg. 2017 Nov 01;83(11):1209-1213. [PubMed: 29183521]
- 9.
- Del Vecchio Blanco G, Gesuale C, Varanese M, Monteleone G, Paoluzi OA. Idiopathic acute pancreatitis: a review on etiology and diagnostic work-up. Clin J Gastroenterol. 2019 Dec;12(6):511-524. [PubMed: 31041651]
- 10.
- Brägelmann J, Barahona Ponce C, Marcelain K, Roessler S, Goeppert B, Gallegos I, Colombo A, Sanhueza V, Morales E, Rivera MT, de Toro G, Ortega A, Müller B, Gabler F, Scherer D, Waldenberger M, Reischl E, Boekstegers F, Garate-Calderon V, Umu SU, Rounge TB, Popanda O, Lorenzo Bermejo J. Epigenome-Wide Analysis of Methylation Changes in the Sequence of Gallstone Disease, Dysplasia, and Gallbladder Cancer. Hepatology. 2021 Jun;73(6):2293-2310. [PubMed: 33020926]
- 11.
- Patel SS, Kohli DR, Savas J, Mutha PR, Zfass A, Shah TU. Surgery Reduces Risk of Complications Even in High-Risk Veterans After Endoscopic Therapy for Biliary Stone Disease. Dig Dis Sci. 2018 Mar;63(3):781-786. [PubMed: 29380173]
- 12.
- Genser L, Vons C. Can abdominal surgical emergencies be treated in an ambulatory setting? J Visc Surg. 2015 Dec;152(6 Suppl):S81-9. [PubMed: 26522504]
- 13.
- Coleman J. Bile duct injuries in laparoscopic cholecystectomy: nursing perspective. AACN Clin Issues. 1999 Nov;10(4):442-54. [PubMed: 10865529]
Disclosure: Mark Jones declares no relevant financial relationships with ineligible companies.
Disclosure: Connor Weir declares no relevant financial relationships with ineligible companies.
Disclosure: Sassan Ghassemzadeh declares no relevant financial relationships with ineligible companies.
Publication Details
Author Information and Affiliations
Authors
Mark W. Jones1; Connor B. Weir2; Sassan Ghassemzadeh3.Affiliations
Publication History
Last Update: April 24, 2023.
Copyright
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
Publisher
StatPearls Publishing, Treasure Island (FL)
NLM Citation
Jones MW, Weir CB, Ghassemzadeh S. Gallstones (Cholelithiasis) [Updated 2023 Apr 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.