This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
This publication is provided for historical reference only and the information may be out of date.
Introduction
In the United States, trauma remains the leading cause of death in adults. Of all injuries sustained in trauma, the aortic injury is one of the most time-sensitive, life-threatening conditions, second only to head injury as a cause of death. The morbidity and mortality associated with traumatic aortic injury are about 30% within the first 24 hours. Some predisposing factors for traumatic aortic injury include penetrating chest injuries, deceleration injuries, and blunt chest trauma. There are no clinical findings specific to aortic injury. However, hypotension, external evidence of trauma, and altered mental status are common. Many patients with complete transection of the thoracic aorta die before arriving at the emergency department (ED). Those who survive arrival in the ED may have small tears or partial-thickness tears of the aortic wall with a pseudo-aneurysm formation. The survival of patients after traumatic aortic injury depends on a clinician’s high index of suspicion, rapid diagnosis, and prompt management.[1][2][3]
Etiology
Blunt force trauma is more common. This involves rapid deceleration mechanisms such as motor vehicle accidents or falls from great heights. Aortic trauma can also be caused by penetrating traumas, such as stab injury and firearm injury.[4]
Epidemiology
It is the second most common cause of death in patients with blunt force trauma (head trauma is the most common). Over 80% of those with aortic injury die at the scene. Up to 15% of all deaths following motor vehicle collisions are due to injury to the thoracic aorta.
Pathophysiology
The aorta has some fixed regions, particularly the relatively fixed aortic arch (to the thoracic inlet by the brachiocephalic vessels). The remaining portions of the aorta are relatively free. Ascending and descending aorta are relatively mobile except at specific points. These can result in an unequal distribution of shear forces on the relatively fixed arch and mobile ascending and descending aorta and stress at the site of attachment of the aorta, particularly the aortic root and the aortic isthmus.
The most common sites of injury are the following:
- Aortic isthmus
- Just distal to the origin of the left subclavian artery. This is the transition zone between the mobile ascending aorta and the relatively fixed descending aorta.
- Tethered site of the aorta at the ligamentum arteriosum.
- Ascending aorta, just proximal to the origin of the brachiocephalic vessels.
Major mechanisms involved in aortic trauma injuries are as follows:
- Rapid acceleration and deceleration. Significant deceleration occurs in head-on collisions or lateral impact. The greatest risk involves frontal or side impacts.
- Significant falls, greater than 4 meters can also result in aortic trauma. These involve the thoracic aorta. In this case, significant physical forces can result in; blunt force compression of chest wall contents (particularly the aorta against the spinal column and tearing of the aorta. In addition, this type of trauma may cause the vertebral column, sternum, first rib, and clavicle to compress the aorta in the region of the isthmus.
- Twisting against fixation points – usually, twisting of the aorta at the ligamentum arteriosum just distal to the left subclavian artery can also result in aortic trauma.
- Seatbelt injuries: This involves the abdominal aorta. Although the abdominal aorta is relatively rarely injured in blunt trauma, severe trauma may disrupt the abdominal aorta.
- Other high-risk mechanisms involved in blunt aortic trauma such as the ejection of an unrestrained passenger from the vehicle, and injuries resulting in death at the scene of the accident.
- Mechanism of injury: rupture of the adventitia. This can cause lethal internal hemorrhage.
Type of injury:
- Intimal tear: This leads to disruption of the media and can cause a false lumen.
- Mediastinal hematoma: Since traumatic aortic injury differs from spontaneous aortic injury with respect to the involvement of multiple layers of the aorta, mediastinal hematoma usually develops secondary to trauma.
- Transection of the aorta: Complete rupture of the aorta, including the adventitial layer and periadventitial connective tissue, results in immediate exsanguination.
Beware that delayed adventitial rupture may occur during hospitalization.
History and Physical
History
There are no clinical findings specific for aortic injury. However, hypotension, external evidence of trauma, and altered mental status are common.
The symptoms may include the following:
- Chest pain: Usually retro-sternal, or intra-scapular pain
- Difficulty breathing or swallowing
- Dysphagia, stridor, or a hoarse voice, may occur due to pressure from a mediastinal hematoma.
Be aware that symptoms may not reliably predict aortic injury.
Physical Examination
- Usually, no clinical signs of traumatic aortic injury are present in patients with aortic injury
- Steering wheel marks or seatbelt signs may be present.
- A discrepancy may exist between the blood pressures in each arm. Upper-extremity hypertension
- Femoral pulses may be diminished or absent
- Pseudo-coarctation: Increased blood pressure in upper extremities and lower blood pressure in the lower extremities
- A new heart murmur not previously present
Evaluation
Clinical suspicion should be based on the mechanism and severity of the injury, the hemodynamic stability of the patient, and/or the presence of associated injuries. The possibility of aortic injuries should be considered and excluded in patients with a history of falls from heights or high-speed motor vehicle crashes.[5][6]
Chest Radiograph
Although this has low sensitivity, it is used as a primary screening test and often determines whether additional imaging is required.
The following findings may be present in patients with aortic injury; but, they are not diagnostic.
- Widening of the mediastinum (this may not be evident)
- If it is greater than 8 cm at the level of the aortic arch, it requires further evaluation and imaging studies.
- Loss of the normal shadow of the aortic knob
- Left apical pleural cap of fluid, or blood
- Left pleural effusion
- Deviation/Displacement of the trachea, or esophagus to the right
Beware that it is difficult to assess these findings on a supine, portable chest radiograph.
FAST Examination
Although FAST examination is required to evaluate any intra-abdominal injury, it may not provide adequate information about the aortic injury, since it does not include the aorta.
CT Scan
The decision of whether to obtain a CT scan or angiography depends on institutional preferences, the patient's status, and the presence of associated injuries. CT scan is an initial screening modality for patients where the mechanism of injury may suggest this type of injury. In recent years, newer generation multi-detector helical CT scans have replaced angiography.
CTA Chest
Currently, CT angiography is increasingly used, and it is the investigational modality of choice. Most experts agree that a negative CT-angiogram may obviate the need for angiography. It should be obtained in patients who are involved in high-speed accidents, to exclude aortic injury.
For mediastinal hematoma, the following signs may be seen:
- Abnormal soft tissue density around the mediastinal structures
- A periaortic hematoma is a sensitive finding of aortic injury.
The following signs may suggest aortic injury:
- Intraluminal filling defect due to intimal flap or clot. An intimal flap is visible in most patients with an aortic injury.
- Abnormal aortic contour due to mural hematoma.
- Pseudoaneurysm formation: tear in the muscularis layer occurs, through which the intimal layer may protrude. This may make it susceptible to rupture.
- Extravasation of contrast: Active extravasation of injected contrast medium suggests active hemorrhage and necessitates immediate thoracotomy.
The severity of the aortic injury is classified as follows:
- Type 1: Intimal tear
- Type 2: Intramural hematoma
- Type 3: Pseudo-aneurysm
- Type 4: Rupture
Treatment / Management
Treatment of an aortic injury is a surgical emergency. The survival of patients following a traumatic aortic injury depends on early recognition, rapid diagnosis, and prompt management. Surgical repair of the injured thoracic aorta is associated with high mortality and morbidity. The initial resuscitation includes ABCDE, based upon Advanced Trauma Life Support (ATLS) principles: If any life-threatening condition is identified, it should be immediately treated.[7][8][9]
Assessment of associated injuries includes:
- Rapid identification and control ongoing hemorrhage
- Monitoring and controlling the heart rate and blood pressure
- Avoiding over-resuscitation
Management decisions for patients with aortic injury depend on the following:
- Hemodynamic status of the patient: Patients who are hemodynamically unstable should be immediately taken to the operating room. Consider major intra-thoracic injury, if a chest tube drains a large initial rush of bright red arterial blood, or has significant blood (more than 200 ml). Such a patient should be taken to the operating room, immediately.
- The severity of injury: Generally, for type 1 injuries, nonoperative management is suggested. Patients with intimal hemorrhage with and without partial intimal laceration may heal spontaneously. However, the repair is required for type 2, 3, and 4 aortic injuries.
Associated injuries and medical conditions: beware that despite having a contained aortic injury, the patient may be hemodynamically unstable due to hemorrhage from other organs, such as the liver or spleen. Hemorrhage control is still the priority. However, if the aorta is not the cause of active hemorrhage, control of active bleeding should be the priority.
Indications for operative repair are as follows:
- Unstable patient
- Large amount of blood return from the chest tube (more than 200 ml)
- Contrast extravasation on CT scan
- Rapidly expanding mediastinal hematoma
- Penetrating aortic injury.
Surgical treatment is by either primary repair of the aorta or resection of the injured segment and grafting. The repair of the aorta should not be delayed beyond the time required to evaluate and treat other emergent conditions. The aortic repair can be performed by either an open or endovascular method. Since the endovascular technique is not widely available, its role in the treatment of traumatic aortic disruption has yet to be determined.
Differential Diagnosis
- Aortic regurgitation imaging
- Aortic stenosis imaging
- Cardiogenic shock
- Emergent management of pleural effusion
- Mechanical back pain
- Myocardial infarction
- Myocarditis
- Pleural effusion
- Pulmonary embolism (PE)
- Thoracic outlet syndrome imaging
Enhancing Healthcare Team Outcomes
Aortic trauma is not an uncommon presentation to the emergency department. The condition needs a prompt referral to a thoracic or vascular surgeon. Because of the risk of rupture and high mortality, the condition is best managed by an interprofessional team that includes an emergency department physician, trauma surgeon, thoracic surgeon, interventional radiologist, vascular surgeon, and intensivist. Once diagnosed the two options for repair include open surgery or an endovascular procedure. The patient should be closely monitored in an ICU setting after surgery. The biggest risk of surgery is paraplegia, which even in the best of hands occurs at a rate of 5-10%.[10][11][12] [level 5]
References
- 1.
- Senst B, Kumar A, Diaz RR. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Sep 12, 2022. Cardiac Surgery. [PubMed: 30422530]
- 2.
- Engelhardt M, Elias K, Debus S, Zischek C. [Management of Vascular Trauma in Military Conflicts and Terrorist Attacks]. Zentralbl Chir. 2018 Oct;143(5):466-474. [PubMed: 30357789]
- 3.
- Siiskonen T, Ciraj-Bjelac O, Dabin J, Diklic A, Domienik-Andrzejewska J, Farah J, Fernandez JM, Gallagher A, Hourdakis CJ, Jurkovic S, Järvinen H, Järvinen J, Knežević Ž, Koukorava C, Maccia C, Majer M, Malchair F, Riccardi L, Rizk C, Sanchez R, Sandborg M, Merce MS, Segota D, Sierpowska J, Simantirakis G, Sukupova L, Thrapsanioti Z, Vano E. Establishing the European diagnostic reference levels for interventional cardiology. Phys Med. 2018 Oct;54:42-48. [PubMed: 30337009]
- 4.
- Pelletti G, Cecchetto G, Viero A, De Matteis M, Viel G, Montisci M. Traumatic fatal aortic rupture in motorcycle drivers. Forensic Sci Int. 2017 Dec;281:121-126. [PubMed: 29127893]
- 5.
- Aida H, Kagaya S. [Experience of Surgical Repair for Cardiac Trauma]. Kyobu Geka. 2018 Sep;71(9):643-647. [PubMed: 30185736]
- 6.
- Tanious A, Wooster M, Giarelli M, Armstrong PA, Johnson B, Illig KA, Zwiebel B, Grundy LS, Hooker R, Caldeira C, Back MA, Shames ML. Positive Impact of an Aortic Center Designation. Ann Vasc Surg. 2018 Jan;46:142-146. [PubMed: 28887248]
- 7.
- Katayama Y, Kitamura T, Hirose T, Kiguchi T, Matsuyama T, Sado J, Kiyohara K, Izawa J, Tachino J, Ebihara T, Yoshiya K, Nakagawa Y, Shimazu T. Delay of computed tomography is associated with poor outcome in patients with blunt traumatic aortic injury: A nationwide observational study in Japan. Medicine (Baltimore). 2018 Aug;97(35):e12112. [PMC free article: PMC6392548] [PubMed: 30170440]
- 8.
- Marcaccio CL, Dumas RP, Huang Y, Yang W, Wang GJ, Holena DN. Delayed endovascular aortic repair is associated with reduced in-hospital mortality in patients with blunt thoracic aortic injury. J Vasc Surg. 2018 Jul;68(1):64-73. [PMC free article: PMC6019106] [PubMed: 29452832]
- 9.
- Trust MD, Teixeira PGR. Blunt Trauma of the Aorta, Current Guidelines. Cardiol Clin. 2017 Aug;35(3):441-451. [PubMed: 28683912]
- 10.
- Ajaja MR, Cheikh A, Moutaouekkil EM, Madani M, Arji M, Hassani AE, Lakhal B, Slaoui A. Endovascular treatment of acute aortic isthmian ruptures: case study. Pan Afr Med J. 2017;28:217. [PMC free article: PMC5881556] [PubMed: 29629003]
- 11.
- Ghazy T, Mikulasch S, Reeps C, Hoffmann RT, Wijatkowska K, Diab AH, Kappert U, Matschke K, Weiss N, Mahlmann A. Experts' Results in Blunt Thoracic Aortic Injury are Reproducible in Lower Volume Tertiary Institutions. Early and Mid-term Results of an Observational Study. Eur J Vasc Endovasc Surg. 2017 Nov;54(5):604-612. [PubMed: 28958467]
- 12.
- Pu X, Huang XY, Ning Y, Wu WH, Pu JZ, Huang LJ. [Effect of emergency thoracic endovascular aortic repair in patients with acute traumatic thoracic aortic injury]. Zhonghua Xin Xue Guan Bing Za Zhi. 2018 Jul 24;46(7):559-563. [PubMed: 30032548]
Disclosure: Steven Myers declares no relevant financial relationships with ineligible companies.
Disclosure: Muhammad Waseem declares no relevant financial relationships with ineligible companies.
Figures

X-ray, Cardiac, Traumatic Aortic Injury Contributed by chestatlas.com (H. Shulman MD)
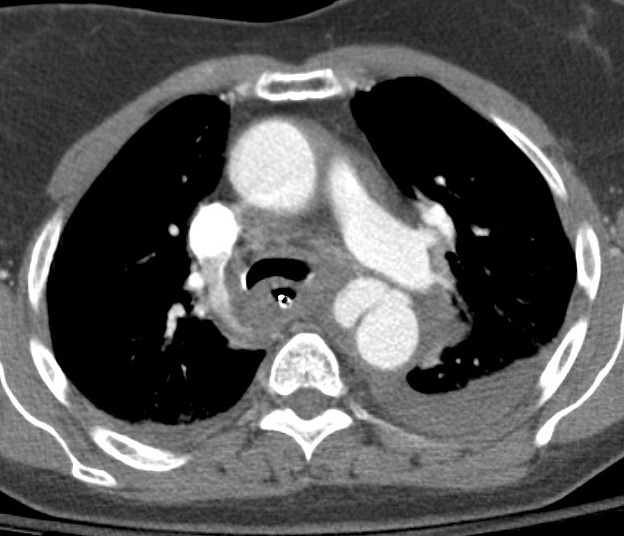
CT Scan, Cardiac, Traumatic Aortic Injury Contributed by chestatlas.com (H. Shulman MD)

Cardiac, Traumatic Aortic Injury Contributed by chestatlas.com (H. Shulman MD)

CT Scan, Cardiac, Traumatic Aortic Injury Contributed by chestatlas.com (H. Shulman MD)

CT Scan, Cardiac, Traumatic Aortic Injury Contributed by chestatlas.com (H. Shulman MD)