This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
Continuing Education Activity
Epistaxis (nosebleed) is one of the most common ear, nose, and throat (ENT) emergencies that present to the emergency room or primary care. There are two types of nosebleeds: anterior (more common), and posterior (less common, but more likely to require medical attention). The source of 90% of anterior nosebleeds lies within Kiesselbach's plexus (also known as Little's area) on the anterior nasal septum. This activity reviews the cause, pathophysiology, and presentation of epistaxis and highlights the role of the interprofessional team in its management.
Objectives:
- Recall the causes of epistaxis.
- Describe the common anatomic locations of epistaxis.
- Summarize the treatment options for epistaxis.
- Review the importance of improving care coordination among interprofessional team members to improve outcomes for patients affected by epistaxis.
Introduction
Epistaxis (nosebleed) is one of the most common ear, nose, and throat (ENT) emergencies that present to the emergency department or the primary care clinic. There are two types of nosebleeds: anterior (more common), and posterior (less common, but more likely to require medical attention). The source of 90% of anterior nosebleeds is within Kiesselbach's plexus (also known as Little’s area) on the anterior nasal septum. There are five named vessels whose terminal branches supply the nasal cavity:
1) Anterior ethmoidal artery
2) Posterior ethmoidal artery
3) Sphenopalatine artery
4) Greater palatine artery
5) Superior labial artery
The watershed area of these five vessels is in the anterior nasal septum, comprising Kiesselbach's plexus. This lies at the entrance to the nasal cavity and so is subject to extremes of heat and cold, and of high and low moisture, and is easily traumatized. The mucosa over the septum in this area is especially thin, making this the site of the majority of epistaxis. More rarely, vessels in the posterior or superior nasal cavity will bleed, leading to the so-called "posterior" epistaxis. This is more common in patients on anticoagulants, patients who are hypertensive, and patients with underlying blood dyscrasia or vascular abnormalities. Management will depend on the severity of the bleeding and the patient's concomitant medical problems.[1][2][3]
Etiology
There are multiple causes of epistaxis which can be divided into local, systemic, environmental, and medication-induced.
Local causes:
- Digital manipulation
- Deviated septum
- Trauma
- Chronic nasal cannula use
Systemic causes:
- Alcoholism
- Hypertension
- Vascular malformations
- Coagulopathies (von Willebrand disease, hemophilia)
Environmental factors:
- Allergies
- Environmental dryness ( more common in winter months)
Medications:
- NSAIDs (ibuprofen, naproxen, aspirin)
- Anticoagulants (warfarin)
- Platelet aggregation inhibitors (clopidogrel)
- Topical nasal steroid sprays
- Supplement/alternative medications (vitamin E, ginkgo, ginseng)
- Illicit drugs (cocaine)
While epistaxis is a very common spontaneous problem, rarer etiologies such as neoplasms or vascular malformations must always be in the differential diagnosis, particularly if additional symptoms such as unilateral nasal obstruction, pain, or other cranial nerve deficits are noted.[4][5][6]
Epidemiology
Nosebleeds are rarely fatal, accounting for only four of the 2.4 million deaths in the United States. About 60% of people have experienced a nosebleed during their life, and only 10% of nosebleeds are severe enough to warrant treatment/medical intervention. They occur most commonly in children ranging from 2 to 10 years old and the elderly ranging from 50 to 80 years old.
Pathophysiology
Nosebleeds are caused by the rupture of a blood vessel within the nasal mucosa. Rupture can be spontaneous, initiated by trauma, use of certain medications, and/or secondary to other comorbidities or malignancies. An increase in the patient's blood pressure can increase the length of the episode. Anticoagulant medications, as well as clotting disorders, can also increase the bleeding time.
Most nosebleeds occur in the anterior part of the nose (Kiesselbach's plexus), and an etiologic vessel can usually be found on careful nasal examination.
Bleeding from the posterior or superior nasal cavity is often termed a posterior nosebleed. This is usually presumed due to bleeding from Woodruff's plexus, which are the posterior and superior terminal branches of the sphenopalatine and posterior ethmoidal arteries. These are often difficult to control and are associated with bleeding from both nostrils or into the nasopharynx, where it is swallowed or coughed up, presenting as hemoptysis. It can generate a greater flow of blood into the posterior pharynx and have a higher risk for airway compromise or aspiration due to increased difficulty in controlling the bleed.
History and Physical
The history should include duration, severity, frequency, laterality of the bleed, inciting event, and interventions provided prior to seeking care. Inquire about anticoagulant, aspirin, NSAID, and topical nasal steroid use. Obtain a relevant family history, particularly relating to coagulopathy and vascular/collagen disease, as well as any history of drug and alcohol use.
Prepare proper equipment and proper personal protective equipment (PPE) before beginning the physical examination. Equipment may include a nasal speculum, bayonet forceps, headlamp, suction catheter, packing, silver nitrate swabs, cotton pledgets, and topical vasoconstrictors and anesthetic. Have the patient in a seated position in an exam chair in a room with suction available. Carefully insert the speculum and slowly open the blades to visualize the bleeding site. A headlight is essential to allow for hands-free illumination, and clot may need to be suctioned from the nasal cavity to identify the bleeding source.
A posterior nosebleed is not easy to visualize and may be suggested by active bleeding into the posterior pharynx without a visualized vessel on nasal examination. Nasal endoscopy greatly increases the success in identifying the bleeding source.
Evaluation
Differentiating an anterior or posterior is key in management. Diagnosis of anterior bleeding is can be made by direct visualization using a nasal speculum and light source. A topical spray with anesthetic and epinephrine may be helpful for vasoconstriction to help control bleeding and to aid in the visualization of the source. Usually, the diagnosis of posterior bleeding is made after measures to control anterior bleeding have failed. Clinical features of posterior bleeding can include active bleeding into the posterior pharynx in the absence of an identified anterior source; high-flow posterior bleeds may cause blood to emanate from both nares. Labs may be obtained if necessary, including a complete blood cell count (CBC), type and cross match, and coagulation studies, though should not delay treatment of an active bleed. Imaging such as x-ray or computed tomography have no role in the urgent or emergent management of active epistaxis.
Treatment / Management
Start with a primary survey and address the airway, ensure the airway is patent. Next, assess for hemodynamic compromise. Obtain large-bore intravenous access in patients with severe bleeding and obtain labs. Reverse blood clotting as necessary, if there is a concern with medication use.[7][8][9]
All patients with moderate to severe nose bleeding should have two large-bore intravenous lines and infusion of crystalloid. The monitoring of oxygen and hemodynamic stability is vital.
Treatment for anterior bleeding can be started with direct pressure for at least 10 minutes. Have the patient apply constant direct pressure by pinching the nose over the cartilaginous tip (instead of over the bony areas) for a few minutes to try to control the bleed. If that is ineffective, vasoconstrictors such as oxymetazoline or thrombogenic foams or gels can be employed. It is important to remove all clot with suction before any attempt at treatment is made. The reasons are twofold: 1) Clot will prevent any medication from reaching the vessel itself and 2) if packing becomes necessary, the clot can be pushed into the nasopharynx and aspirated. If topical treatments are unsuccessful, proceed with nasal examination to identify and cauterize the vessel with silver nitrate. If this too is unsuccessful, anterior nasal packing is necessary. This can be performed with absorbable packing material such as surgicel or fibrillar, or with devices such as anterior epistaxis balloons, or nasal tampons (Rapid Rhino). If silver nitrate is used to cauterize a septal blood vessel, only use it on one side of the septum to prevent septal perforation. Thermal coagulation is painful and should rarely be attempted in an emergent setting.
Traditional petrolatum gauze can be used if one does not have access to balloons or tampons.
If none of this is successful, the bleeding may be from the posterior or superior nasal cavity. Symptoms can include active bleeding from both nostrils or active bleeding present in the posterior pharynx. Longer (7.5cm) nasal tampons are available that provide some more posterior pressure and can be employed in this situation. Formal posterior nasal packing should only be performed by experienced personnel as it requires admission and telemetry monitoring, and sometimes intubation. It is associated with higher rates of complications like pressure necrosis, infection, or hypoxia, and may trigger a nasal-cardiac reflex (sudden bradycardia after nasal packing - if this occurs, remove the pack immediately). Foley catheters can be used by experienced personnel to tamponade a posterior bleed. If a posterior pack is placed, a formal petrolatum gauze anterior pack must be placed as well to create a closed, tamponaded space in the nasopharynx.
If all of these measures are unsuccessful, the patient should be intubated for airway protection and interventional radiology consulted emergently for embolization. If this service is unavailable, operative ligation of the sphenopalatine and ethmoid arteries can be performed in the operating room by an otolaryngologist.
Differential Diagnosis
- Nasal tumor
- DIC
- Hemophilia
- Von Willebrand disease
- Rhinitis
- Foreign body in the nose
- Drug toxicity (Warfarin, NSAIDs)
Postoperative and Rehabilitation Care
Once the bleeding is controlled, it is important to arrange timely follow-up (within one week) with their primary care physician or an otolaryngologist. If any packing has been placed, this must remain undisturbed for 3-5 days before removal. Patients should begin an anti-staphylococcal antibiotic to prevent toxic shock syndrome. Underlying causes must be addressed before discharge (tight blood pressure control with goal SBP <120 mm Hg, reveral of any coagulopathy, etc.), and patients should use topical nasal saline in both nares to keep the packs moist and facilitate removal.
Pearls and Other Issues
Patients with anterior nosebleeds can be discharged if the bleeding is controlled and hemodynamic stability is observed for at least one hour in the emergency department (ED), as well as having all predisposing factors medically optimized. Follow up with an otolaryngologist or their primary physician should occur in one week and they should begin nasal saline three times daily. If non-biodegradable packing is used, patients should return to the ED or ENT for packing removal in three to five days. If a patient, including pediatric patients, require posterior packing, admission is required to monitor for complications, particularly cardiac arrhythmias. All anticoagulants should ideally be discontinued but must be reversed or withheld to achieve the lowest dose acceptable if discontinuation is not possible.
Application of topical saline sprays or ointments to the nasal mucosa to ensure moisturization of the nasal mucosa can help to prevent recurrent epistaxis. Patients should also be advised to avoid hot foods, strenuous activity, blowing nose, or digital manipulation of the nose on discharge.
Enhancing Healthcare Team Outcomes
The care of nose bleeding is best performed by an interprofessional team. Most patients initially present to the emergency room and the triage nurse should be fully aware of the importance of admitting patients with a significant bleed. While most anterior nosebleeds can be arrested with digital pressure, a follow-up appointment is recommended in patients with repeat episodes. Even though nurses may not perform invasive procedures to stop the bleeding, they can be very effective in instructing patients how to properly compress the nose with fingers, which in most cases can arrest the bleeding.
Nasal packing is another option but the packing must be in place for three to five days, and repeated insertions and removals of various packs will only exacerbate the bleeding. Drug-induced nosebleeds may require a reversal of the INR and admission. The pharmacist should ensure that the patient does not restart the NSAID or other anticoagulant while the bleeding is active. A hematologist consult is recommended to deal with patients with coagulopathy. In rare cases, embolization or cauterization may be required to stop a nose bleed. If the bleeding is posterior and/or severe, an ENT consultation is necessary. In some cases, the invasive radiologist may be required to perform embolization to stop the bleeding. Nurses should monitor the oxygen and hemodynamic status of all patients with moderate to severe nose bleeds. These patients should have intravenous access with the transfusion of crystalloids. The team members should communicate with each other to ensure that the patient is receiving the acceptable standard of care treatment.
References
- 1.
- Fishman J, Fisher E, Hussain M. Epistaxis audit revisited. J Laryngol Otol. 2018 Dec;132(12):1045. [PubMed: 30674370]
- 2.
- Send T, Bertlich M, Eichhorn KW, Ganschow R, Schafigh D, Horlbeck F, Bootz F, Jakob M. Etiology, Management, and Outcome of Pediatric Epistaxis. Pediatr Emerg Care. 2021 Sep 01;37(9):466-470. [PubMed: 30624421]
- 3.
- Kitamura T, Takenaka Y, Takeda K, Oya R, Ashida N, Shimizu K, Takemura K, Yamamoto Y, Uno A. Sphenopalatine artery surgery for refractory idiopathic epistaxis: Systematic review and meta-analysis. Laryngoscope. 2019 Aug;129(8):1731-1736. [PubMed: 30613985]
- 4.
- INTEGRATE (UK National ENT research trainee network) on its behalf: Mehta N, Stevens K, Smith ME, Williams RJ, Ellis M, Hardman JC, Hopkins C. National prospective observational study of inpatient management of adults with epistaxis - a National Trainee Research Collaborative delivered investigation. Rhinology. 2019 Jun 01;57(3):180-189. [PubMed: 30610832]
- 5.
- Clark M, Berry P, Martin S, Harris N, Sprecher D, Olitsky S, Hoag JB. Nosebleeds in hereditary hemorrhagic telangiectasia: Development of a patient-completed daily eDiary. Laryngoscope Investig Otolaryngol. 2018 Dec;3(6):439-445. [PMC free article: PMC6302722] [PubMed: 30599027]
- 6.
- Ramasamy V, Nadarajah S. The hazards of impacted alkaline battery in the nose. J Family Med Prim Care. 2018 Sep-Oct;7(5):1083-1085. [PMC free article: PMC6259556] [PubMed: 30598962]
- 7.
- Joseph J, Martinez-Devesa P, Bellorini J, Burton MJ. Tranexamic acid for patients with nasal haemorrhage (epistaxis). Cochrane Database Syst Rev. 2018 Dec 31;12(12):CD004328. [PMC free article: PMC6517002] [PubMed: 30596479]
- 8.
- Wong AS, Anat DS. Epistaxis: A guide to assessment and management. J Fam Pract. 2018 Dec;67(12):E13-E20. [PubMed: 30566119]
- 9.
- Santander MJ, Rosenbaum A, Winter M. Topical tranexamic acid for spontaneous epistaxis. Medwave. 2018 Dec 10;18(8):e7372. [PubMed: 30550535]
Disclosure: Ayesha Tabassom declares no relevant financial relationships with ineligible companies.
Disclosure: Julia Dahlstrom declares no relevant financial relationships with ineligible companies.
Figures
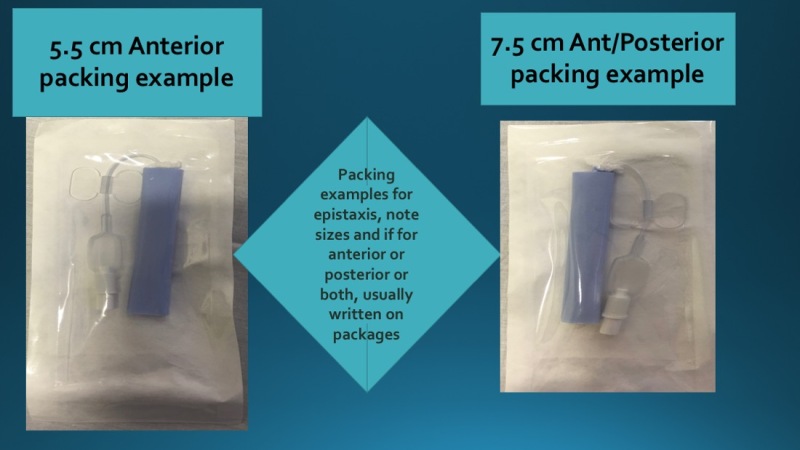
Epistaxis management supplies that may be needed for packing such as Rapid Rhino examples, Anterior and Posterior packing Contributed by Tammy J. Toney-Butler, AS, RN, CEN, TCRN, CPEN
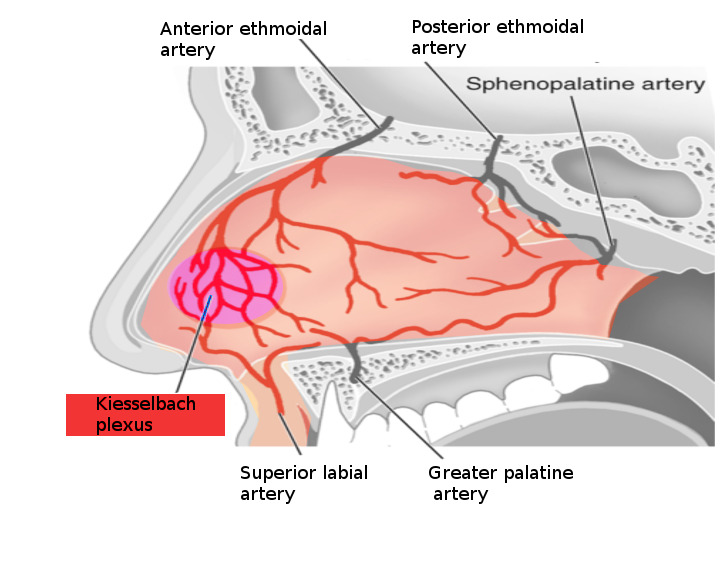
Nose bleed vessels Image courtesy S Bhimji MD