NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-.
ABSTRACT
Diabetic foot ulcers (DFU) are associated with significant impairment of quality of life, increased morbidity and mortality, and are a huge drain on health care resources. In Western countries, the annual incidence of foot ulceration in the diabetic population is around 2%. DFUs develop as a consequence of a combination of factors, most commonly peripheral neuropathy (loss of the gift of pain), peripheral arterial disease (PAD), and some form of unperceived trauma. Recent studies emphasize the very high prevalence of foot ulceration in people with diabetes on dialysis as a consequence of end-stage renal disease. The mortality in this patient group is higher than for most forms of cancer. All patients with diabetes should have an annual screen to identify their foot ulcer risk status: those with any risk factors require specific foot care education as well as regular contact with a health care professional, usually a podiatrist. DFUs should heal if there is an adequate arterial inflow, infection is aggressively managed, and pressure is removed from the wound and its margins. In the management of plantar neuropathic ulcers, offloading is critical and all efforts must be made to enhance patient understanding of the need for offloading. Antibiotic usage should be guided by clinical signs of infection and microbiologic analysis of deep tissue specimens: evidence now exists to show that oral antibiotics are equally efficacious as intravenous in treating most cases of osteomyelitis in the diabetic foot. Most adjunctive therapies have little evidence to support their use although recent trials suggest efficacy for a number of topical therapies including LeucoPatch (3C patch) and sucrose octasulphate; and negative pressure wound therapy has also been shown to be helpful in certain cases. There is currently no indication for hyperbaric oxygen usage, whereas recent studies suggest that topical oxygen therapies help wound healing. Charcot neuroarthropathy (CN) should be easily preventable: most important is to treat any neuropathic patient with a warm swollen foot as having CN until proven otherwise. For complete coverage of all related areas of Endocrinology, please visit our on-line FREE web-text, WWW.ENDOTEXT.ORG.
INTRODUCTION
At the beginning of the 21st Century, diabetic foot problems, although eminently preventable, represent one of the commonest causes of hospital inpatient admission in Western countries. In 2005, the International Diabetes Federation realized the global importance of diabetic foot disease and chose to focus their campaign during the whole year on raising awareness with a worldwide campaign to “put feet first” and highlight the common problem of amputation amongst diabetic patients throughout the world. To coincide with World Diabetes Day 2005 (November 14, birth date of Frederick Banting), the Lancet elected to dedicate a whole issue to diabetic foot problems (1).
In this chapter, the global term “diabetic foot” refers to the variety of pathological conditions that might affect the feet in patients with diabetes. Foot ulcers are defined as lesions involving a skin break with loss of epithelium: they can extend into the dermis and deeper layers sometimes involving bone and muscle. Amputation is defined as “the removal of a terminal, non-viable portion of the limb”. The lifetime risk of a person with diabetes developing a foot ulcer (DFU) has been estimated to be as high as 34% (2).
The suffering of affected individuals and the cost of DFUs are both equally staggering. Those individuals with DFUs usually have other complications of diabetes including nephropathy: data from the UK and the USA confirmed that the outlook for those people with foot complications who are on dialysis is very poor with a high mortality risk (1-3). Data from our group confirm that those people with diabetes who have had an amputation and who are on dialysis have a 75% two-year mortality; the majority of these were of cardiovascular etiology. Data such as these are worse than most malignant diseases, with the possible exception of lung and pancreas. There is therefore an urgent need for preventative strategies to reduce the incidence of foot complications amongst those with diabetes. With respect to costs, in 2008 Rogers et al (4) reported that in the US $18 billion was spent on the care of DFUs and US $11.7 billion on lower extremity amputations. More recently, data from the UK in 2019 suggest that a conservative estimate of the annual cost of diabetic foot problems exceeds UK £900 million which represents approximately 1% of the total budget of the National Health Service (5).
The importance of regular diabetic foot care in very high-risk patients is emphasized by an observational study from Arizona where the State decided to remove routine podiatry from high-risk patients to reduce their health budget. This led to an annual saving of US $351,000 but the cost of this action measured by increased hospitalization, length of stay, and amputations was $16.7 million (6).
This chapter will include a discussion on the epidemiology of foot problems including foot ulceration, amputations, and Charcot neuroarthropathy (CN). The etiopathogenesis will then be described and aspects of management of neuropathic, neuroischemic, and infected DFUs considered. The question of how to address primary and secondary prevention of diabetic foot problems will then be discussed followed by a section on Charcot neuroarthropathy. For more detailed discussion, the reader is referred to review articles on these topics (2,7-9).
EPIDEMIOLOGY OF THE DIABETIC FOOT
The study of the epidemiology of diabetic foot disease has been beset by numerous problems relating to both diagnostic tests used, and population selected. However, there is little doubt that foot complications are common. In the UK, the North West Diabetes Foot Care Study (a community-based study of over 15,000 people) reported that the annual incidence of foot problems amongst the population with diabetes was just under 2% (10), with similar results having been reported from the Netherlands. Similarly, when discussing amputations, the figures vary widely again due to diagnostic criteria as well as regional differences. It must be remembered that many individuals at diagnosis of type 2 diabetes have significant neuropathy: in the United Kingdom Prospective Diabetes Study, for example, 13% of patients at diagnosis had neuropathy of sufficient severity to put them at risk for foot ulceration (7).
With respect to ethnicity, studies from the UK suggest that foot ulcers and amputations appear to be less common in Asians of Indian sub-continental origin and Afro-Caribbean men. In contrast, reports from the USA suggest that amputation rates are more common amongst African-Americans with diabetes than amongst white Americans. Similarly, ulceration is much more common in Hispanic Americans and native Americans than in non-Hispanic whites (2). More recently, reviews have confirmed the importance of healthcare inequities in diabetic foot disease: race, ethnicity, socioeconomic status, and geography are powerful mediators of risk for DFU and lower-extremity amputation (2,11).
ETIOPATHOGENESIS OF DIABETIC FOOT ULCERATION
The foot does not break down spontaneously and in this section, the many warning signs that the feet are at risk of breakdown will be discussed. This was recognized by Elliott Joslin almost 90 years ago when he stated that “diabetic gangrene is not heaven-sent but is earth-borne” (12). It was previously believed that neuropathy, vascular disease, and infection were the main causes of ulceration: it is now recognized that infection occurs as a consequence of ulceration, and is not a cause thereof. There are many contributory factors to foot ulceration, the most important of which are diabetic neuropathy and peripheral arterial disease (PAD). These and other causative factors are listed in table 1.
Table 1.
Risk Factors for Foot Ulceration
| Peripheral neuropathy Somatic Autonomic |
| Peripheral arterial disease Proximal and/or distal disease |
| Past history of foot ulcers/amputation |
| Other long-term complications End-stage renal disease (especially on dialysis) Post-transplant (including pancreas/kidney transplant) Visual loss |
| Plantar callus |
| Elevated foot pressures |
| Foot deformity |
| Edema |
| Ethnic background |
| Poor social background |
More common contributory factors shown in bold.
Diabetic Neuropathy
Although the association between both somatic and autonomic neuropathy and foot ulceration has been recognized for many years, it is only in the last 20 years that prospective studies have confirmed these assumptions (2,8,10). It has been reported that the risk of developing the first foot ulcer is seven-fold higher in those with moderate to severe sensory loss compared with non-neuropathic diabetic individuals (13). Additionally, poor balance and instability as a consequence of loss of proprioception have been confirmed and are also likely contributory factors not only to foot ulceration, but also to Charcot neuroarthropathy (CN) (2,7,14,15).
Sympathetic autonomic neuropathy in the lower extremity leads to reduced sweating and dry skin that is prone to crack and fissure, and as well, in the absence of PVD, to increased blood flow, arterio-venous shunting, and the warm foot.
As will be discussed later, simple clinical tests may be used to identify the high-risk neuropathic foot (16). Most important in the identification of the high-risk neuropathic foot is good clinical observation and removal of the shoes and socks, with careful inspection of the feet as part of the routine follow up of all patients with diabetes.
Peripheral Arterial Disease (PAD)
A two-center study of causal pathways to foot ulceration reported that peripheral ischemia was a causal component in the pathway to ulceration in 35% of cases (17). In many Western countries, there has been an increase in the percentage of foot ulceration in which ischemia is a contributory factor (18). It is well recognized that patients with diabetes are more prone to distal arterial disease, which may be associated with a poorer outcome.
A detailed discussion of PAD in diabetes is outside the scope of this chapter and readers are directed to reviews on this topic (19, 20). A large follow-up study from Australia has confirmed that the strongest predictors of development of PAD in type 2 diabetes include microvascular complications (particularly macroalbuminuria and photocoagulation for retinopathy (21)).
Other Risk Factors
Of all the risk factors for foot ulceration (table 1), the most important is a past history of ulceration and/or amputation (2). In some series, the annual recurrence rate is up to 50%.
Other Long-term Complications
Those with other late complications particularly nephropathy, have an increased ulcer risk. Visual disturbance as a consequence of retinopathy is a confirmed risk factor; it is easy to understand why this should be. Those patients with sensory loss, particularly large fiber dysfunction, have poor balance and rely on vision as a secondary protective factor. Thus, those who have had for example extensive laser therapy and also have loss of proprioception, are at great risk of foot injury particularly when walking on uneven surfaces and in the hours of darkness.
A strong association between end-stage renal disease and foot ulceration has been emphasized in a number of studies. The temporal association between the start of dialysis treatment and foot ulceration was first confirmed by Game et al (22). A study comprising patients from both the US and the UK subsequently reported a very high prevalence of foot pathology in patients on dialysis, with 46% of patients having past or present foot ulceration and 18% were already amputees (23). The same group later confirmed that being on dialysis is an independent risk factor for foot ulceration in patients with diabetes (3,24). As noted above, preliminary data from the same group suggests that those patients who have already undergone amputation and who are on dialysis have a two-year mortality of up to 75%.
It must also be remembered that patients post-renal transplant or even post-simultaneous pancreas-kidney (SPK) transplant remain at very high risk of developing foot complications. There have been a number of reports of both foot ulceration and Charcot neuroarthropathy occurring in patients post-SPK (25). Theoretically, such subjects are “non-diabetic” but they remain at high risk because they invariably have a dense sensorimotor and autonomic peripheral neuropathy. They should remain under annual review and be coded as ‘diabetes in remission’.
Plantar Callus
Plantar callus forms under weight-bearing areas as a consequence of the dry skin (autonomic neuropathy), insensitivity, and repetitive moderate stress from high foot pressures. Callus itself acts as a foreign body and can cause ulceration in the insensate foot.
Elevated Foot Pressures
Numerous studies have confirmed the contributory role that abnormal plantar pressures play in the pathogenesis of foot ulceration (1, 2, 7). Most studies used sophisticated techniques such as pedobarography to assess foot pressures, but these are not required in day-to-day clinical practice.
Foot Deformities
A combination of motor neuropathy, cheiro-arthropathy, and altered gait pressures is thought to result in the “high-risk” neuropathic foot with clawing of the toes, prominent metatarsal heads, high arch, and small muscle wasting.
Demographics
In Western countries, the male sex has been associated with a 1.6-fold increased risk of foot ulcers (10). There is an increased risk of foot ulceration with increasing age and duration of diabetes.
THE PATHWAY TO FOOT ULCERATION IN DIABETES
As discussed and outlined in Figure 1, the pathway to ulceration is indeed complex and involves an interaction of numerous factors. Whereas none of the factors listed in the last section will alone result in ulceration, it is the interaction and combination of risk factors working together that leads to skin breakdown. In the prospective study of Reiber et al, 63% of all foot ulcers resulted from a combination of neuropathy, deformity, and trauma: in Western countries, the commonest cause of trauma is ill-fitting footwear (17). It must be remembered that as those with neuropathy have reduced sensory input, they will commonly be unable to feel the fit of a shoe until the pressure from the shoe is quite high. Thus, people with neuropathy frequently choose shoes that are too small. All such individuals should be advised to have their feet measured prior to the purchase of any “off the shelf” footwear.
Other simple examples of two risk factors working together in the pathway to ulceration are neuropathy and mechanical trauma (a common scenario is a neuropathic individual with a foreign body in the shoe), neuropathy and thermal trauma (holidays are particularly dangerous), and neuropathy and chemical trauma (such as inappropriate use of over-the-counter chemical corn treatments which should never be used in those with neuropathy).
In summary, whereas neuropathy was present in four out of five cases of new foot ulcers in the Reiber study (17), as noted above, the combination of neuropathy and ischemia is becoming more common in Western countries, and neuro-ischemic ulcers are the commonest type seen in 2023 in diabetic foot clinics.
FOOT ULCERATION
DFUs are common, associated with much morbidity and even mortality but should be eminently preventable. It used to be believed that diabetic foot ulcers were difficult to heal: this is not true: a foot ulcer will heal if it is permitted to do so and this requires attention to three factors-
A That there is adequate arterial inflow to the foot.
B That any infection is appropriately and aggressively managed.
C That all pressure is removed from the wound and its margins.

Figure 1.
Pathways to Diabetic Foot Ulceration.
Despite increased knowledge of the pathogenesis and treatment of diabetic foot ulcers in recent years, it is still the third point, offloading the wound, that is poorly adhered to by health care professionals. Many forget that those with a neuropathic or neuroischemic ulcer have “lost the gift of pain”. That pain is a gift which is only realized when it is lost, as first described by Dr Paul Brand when studying leprosy (28). However, before going into more detail on management, it is important to classify wounds appropriately in order to guide therapeutic management.
CLASSIFICATION OF DIABETIC FOOT WOUNDS
Accurate and concise ulcer description and classification systems are required to improve multidisciplinary collaboration and communication, as well as for aiding treatment choices. For many years, the Meggitt-Wagner grading system was regarded as the gold standard. One problem with this system is that the ischemic status of the wound is not included. Thus, a number of new classification systems for diabetic foot wounds have been proposed and validated over the last 20 years. A commonly used system in the United States is the University of Texas Wound Classification System (29). This incorporates the Meggitt-Wagner grades but also enables the practitioner to stage the wound with respect to the presence or absence of infection and/or ischemia (Figure 2). In a comparative prospective study across two Centers, one in the UK and one in the US, the University of Texas Classification System was shown to be superior to the Meggitt-Wagner system at predicting outcomes (30). However, this study also showed that the traditional Meggitt-Wagner system was itself generally accurate in predicting outcomes.
Most recently, the WIFI (Wound Ischemia, Foot Infection) classification was introduced and is the most commonly used today in the USA, particularly in vascular clinics. This was developed and validated as a method to assess three variables – the wound, level of ischemia and the presence and severity of foot infection – to predict the risk of amputation (Figure 3)
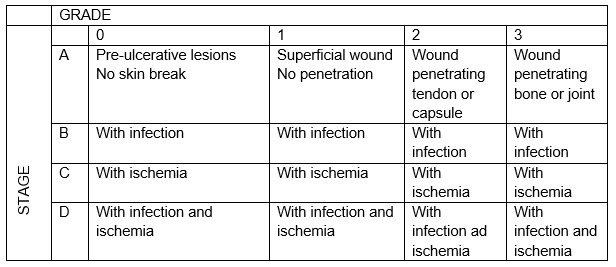
Figure 2.
The University of Texas Wound Classification System.

Figure 3.
WIFI system. Wound, Ischemia, and Foot Infection (WIfI) Classification of Limb Threating diabetic foot disease, tissue loss, ischemia, and infection frequently overlap. However, one is frequently more dominant than the other at different times in the life cycle of an acute-on-chronic event. Here, the amount of tissue loss, ischemia, and foot infection can be ordinally graded to help predict outcome and assist in communicating a plan of action. aA higher score on the WIfI scale is associated with lower extremity amputation and morbidity and can be used to determine the need for revascularization. WIfI scores of 1, 2, 3, and 4 were associated with 1-year amputation rates of 0%, 8%, 11%, and 38%, respectively. Figure from JAMA 2023 Jul 3;330(1):62-75 with permission.
EVALUATION OF THE DIABETIC FOOT ULCER
Clinical evaluation of the foot wound should include a detailed description of the site, size, and depth of the wound. The neuropathic and vascular status of the wound should then be assessed (for details see below). In general, neuropathic ulcers typically occur in the warm but insensate foot, often under pressure bearing areas, and are surrounded by callus. In contrast, ischemic wounds tend to occur in the cool, poorly perfused foot, and are often at lateral fifth metatarsal head regions or the medial first metatarsal head regions. In a predominantly ischemic wound, callus tissue is uncommon. In a neuroischemic wound, the morphology will depend upon the predominance of each of these two pathologies. The correct identification of the degree of ischemia is of the utmost importance when evaluating a wound. If the foot is cool with impalpable pulses, then non-invasive Doppler ultrasound studies are indicated. Conventional methods of assessing tissue perfusion in the peripheral circulation may not be entirely reliable in patients with diabetes. For example, the Ankle Brachial Pressure Index, which is routinely used to screen for PAD in individuals without diabetes, may well be falsely elevated in the those with diabetes because of medial arterial calcification. Toe pressure indices may therefore be more reliable.
Peripheral Arterial Disease
A detailed discussion of vascular procedures is outside the scope of this review, although any person being considered for radiological or surgical procedures will require arteriography. Care must be taken in the use of certain contrast media in patients with chronic renal disease. A detailed discussion of the use of bedside investigations to diagnose PAD in people with diabetes is provided in the recently published guidelines by Fitridge et al (31).
Is Infection Present?
The correct diagnosis of infection in the diabetic foot wound is critical as it is often the combination of untreated infection and PAD that lead to amputation in the diabetic foot. A systematic review that was updated in 2020 still recommend that the diagnosis of infection requiring treatment is a clinical one (32). However, appropriate tissue specimens should be sent to the microbiological laboratory for culture and sensitivity. Superficial swabs are of little use: deep tissue specimens or if osteomyelitis is suspected, bone biopsies are recommended (32) .
A high index of suspicion for the presence of osteomyelitis is essential when assessing the diabetic foot wound. The “probe to bone” (PTB) is often used to diagnose osteomyelitis although there has been much discussion about its accuracy. A systematic review concluded that the PTB test can accurately diagnose osteomyelitis in high-risk patients, and rule out osteomyelitis in low-risk patients (33).
Role of Plain X-Ray in Diagnosing Osteomyelitis
The plain radiograph remains the commonest first radiological investigation of an acutely presenting diabetic foot problem. Despite this, it may be dismissed because of relatively low sensitivity for acute osteomyelitis, with literature over the last 10 years concentrating on CT scanning, MR scanning, and nuclear medicine studies (particularly Gallium Citrate, labelled leucocyte scans and recently PET, PET-CT, SPECT-CT and PET-MR). These latter studies are of limited availability and are expensive, and some carry a high radiation burden. They have their own sensitivity and specificity problems and may not be available in a timely manner. The initial sensitivity of the plain radiograph for acute osteomyelitis is improved by serial studies at one to two-week intervals, during which time therapy for presumed osteomyelitis may be instigated for clinical reasons and whilst awaiting the results of further “high tech” imaging (if still required). The plain radiographic findings could then be considered of high sensitivity and specificity, but with a two-week lag, both for diagnosis and for response to treatment. Appropriate clinical information for the reporting radiologist must include that the patient is diabetic, whether the foot is neuropathic, whether an ulcer is present and if so, its precise anatomical location, and whether it probes to bone. The radiologist should be aware that most sites of acute osteomyelitis in the diabetic foot occur in the floor of an ulcer that probes to bone and that if the foot is neuropathic there may be acute fractures without a history of trauma or acute Charcot neuroarthropathy may be present.
Whilst periosteal reaction is an early feature of osteomyelitis, it is not commonly seen around the small bones of the foot, and if present, is most often seen around metatarsals, and may be due to fracture rather than osteomyelitis.
The hallmark plain radiographic feature of osteomyelitis in the diabetic foot is focal loss of bone density, almost invariably adjacent to the floor of an ulcer. Whilst sometimes described as bone destruction, it is initially bone de-mineralization that causes this appearance, which can reverse on successful treatment, with radiographic re-appearance of the apparently destroyed bone (Figure 4). Obtaining the radiographic view most likely to demonstrate the bone in the floor of an ulcer is therefore an important consideration, often overlooked now that requests are electronic and radiographic views are selected from limited drop-down menus. For example, toe-tip ulcers and ulcers on the dorsum of the inter-phalangeal joints require lateral toe views - best obtained using dental radiographs if available; the inferior surfaces of metatarsal heads are best demonstrated on sesamoid views; the heel requires both lateral and axial views. As a general rule, radiographs tangential to the bone surface at the site of suspected osteomyelitis are ideal, in addition to the standard radiographs of the region. A dedicated team of radiographers familiar with these requirements will improve the relevance and quality of the resultant radiographs.
Plain radiology remains an important investigation in the diagnosis and management of diabetic foot osteomyelitis, but it needs to be of high quality, with appropriate views, and regularly repeated to fulfil its potential.

Figure 4.
Acute presentation with an ulcer at the tip of the great toe, probing to bone. The terminal phalangeal tuft does show some irregularity (left panel). B) two weeks later there is marked bone demineralization consistent with osteomyelitis (middle panel). C) After 2 months of treatment there has been partial remineralization of the bone but with an underlying pathological fracture (right panel).
MANAGEMENT OF DIABETIC FOOT ULCERS
The principles of management of different types of foot ulcers will be discussed in brief in this section. The University of Texas Wound Classification System (Figure 2) will be used throughout.
Neuropathic Plantar Ulcers (UT 1A, 1B, 2A, 2B)
As noted above, neuropathic ulcers tend to occur under pressure areas, particularly at the plantar surface of the forefoot. Other recognized sites include the dorsal areas of the toes, particularly the distal inter-phalangeal joint if there is clawing of the toes. In patients with marked deformities such as those caused by Charcot neuroarthropathy, ulcers may occur at other pressure points, particularly in the plantar mid-foot due to, for example, a dropped cuboid bone. When lecturing on the management of neuropathic diabetic foot problems, one is often asked “what can one put on the wound to heal it?”. The answer is invariably that one should be asking “what should one take off the foot to help heal the ulcer?”. Thus, the management of a plantar neuropathic foot ulcer that is not infected is firstly sharp debridement of the ulcer down to bleeding healthy tissue with removal of all callus tissue over the wound and the edge, and secondly, the removal of pressure from the wound while the person is walking. Pain sensation normally protects wounds from further damage causing the non-neuropathic individual to limp. Any subject with a plantar ulcer who walks into the clinic without limping must, by definition, have loss of pain sensation. A neuropathic individual with a plantar ulcer will therefore walk on the ulcer as there is no warning symptom to inform him or her otherwise. Techniques for removing pressure include the use of casts (either removable or irremovable), boots, half shoes, sandals and felted foam dressings. The total contact cast (TCC) is regarded as the gold standard. Studies that randomize patients to an irremovable TCC, a removable cast walker (RCW), or other offloading devices invariably confirm that healing is fastest in the irremovable device (2,7). Although RCWs and irremovable casts (such as the TCC) offload equally well in the gait laboratory, the irremovable device is always associated with more rapid healing in clinical practice. The problem is that those with neuropathic foot ulcers have lost the sensory cue that tells them not to walk on their active ulcer. Studies suggest that individuals are compliant with wearing the offloading RCW during the day, but feel that home is safer and therefore tend to put slippers on, or even walk barefoot at home. A subsequent trial has confirmed that if the RCW is rendered irremovable by wrapping with scotch cast for example, then the outcome is that there is no difference in healing rates between the TCC and the RCW rendered irremovable (34) . Most people with simple neuropathic foot ulcers (UT grades 1A, 2A, 1B, 2B) generally heal in less than three months although of course this does vary with ulcer size. There is no contraindication to casting neuropathic individuals with mild foot infections (UT grades 2A, 2B). It is recommended that after the wound is healed, offloading should continue for a further four weeks to enable the scar tissue to firm up.
Wound dressings are important to keep the ulcer clean, but the placement of a large dressing on a wound may lead the person to a false sense of security by believing that dressing an ulcer is curative. Nothing could be further from the truth in the neuropathic ulcer. Unfortunately, there is little evidence from randomized controlled trials (RCTs) that any dressing is superior to another. Indeed, Jeffcoate et al (35) randomized people to one of three dressings and could find no difference in outcome according to dressing used: the only difference was in cost. Thus, without an evidence-base, there is no indication to use some of the newer more expensive dressings.
Neuro-ischemic Ulcers
A neuro-ischemic ulcer is one occurring in a foot of a person who has both a neuropathic deficit and impaired arterial inflow: these would be classified UT 1C, 2C in the absence of infection, or 1D, 2D or 3D in the presence of infection. Such individuals warrant full vascular investigation as described above, and referral to the vascular surgery team. The principles of treatment are similar to those for neuropathic ulcers, and it has been confirmed that offloading can safely be used in non-infected neuro-ischemic ulcers under a weight-bearing area. However, antibiotics should be used if there is any suspicion of infection and casting only used with extreme caution in such cases (36). There is now evidence that one dressing, sucrose octasulphate, can improve the healing rates of neuroischemic ulcers in diabetic patients (for further details, see below under adjunctive treatments). With respect to the effectiveness of revascularization of the ulcerated foot in those with neuro-ischemic lesions, results showed that major outcomes following endovascular or open bypass surgery were similar amongst studies (37).
Management of Diabetic Foot Infections
Appropriate wound debridement and offloading together with antibiotics are important in the management of the infected neuropathic foot ulcer, although there are few data from randomized trials to guide the prescriber (32). There is however no evidence that clinically non-infected neuropathic ulcers warrant treatment with antibiotics. With respect to the choice of antibiotic therapy, the reader is directed to the helpful 2012 Infectious Diseases Society of America Clinical Practice Guideline (38). Commonly used broad-spectrum antibiotics include Clindamycin, Cephalexin, Ciprofloxacin, and the Amoxycillin – Clavulanate potassium. Oral antibiotics usually suffice for mild infections, whereas more severe infections including cellulitis and osteomyelitis require intravenous antibiotic usage initially. Care should also be taken to optimize glycemic control, as hyperglycemia impairs leucocyte function.
The above statements on antibiotics refer to initial treatment: after starting with such broad-spectrum antibiotics, when the results of cultured deep tissue specimens are available, antibiotic therapy should be targeted at the likely primary infective organisms. Finally, with respect to duration of antibiotics, there are no data available from randomized trials to help guide the practitioner. Antibiotics should be continued until clinical signs of infection have resolved, but there is no indication to continue antibiotics beyond this period of time and certainly no indication to continue until the wound has healed. A recent review has identified the challenges facing us due to the increasing threat of multidrug-resistant pathogens (39) .
Osteomyelitis
Diagnosis of osteomyelitis has been discussed above both relating to the PTB test and also the use of plain radiographs. Although the treatment of osteomyelitis has traditionally been surgical, there is increasing evidence from case series and a RCT, that osteomyelitis localized to one or two bones, such as digits, may successfully be treated with antibiotics alone (40, 41). A randomized trial from Spain showed that antibiotics alone were not inferior to localized surgery (41). Again, with respect to duration of antibiotic therapy for osteomyelitis, there is no evidence-base to guide us though a recent trial suggests that six weeks’ antibiotic therapy for non-surgically treated diabetic foot osteomyelitis may be sufficient: traditionally, up to three months has been recommended (42). Lastly, many were surprised to read the results of the OVIVA (Oral Vs Intravenous Antibiotics) study (43) which randomized patients with osteomyelitis to oral vs intravenous antibiotics and showed no superiority of either delivery modality. These observations will certainly challenge the approach to osteomyelitis management in the future. A detailed updated review on infection management has been published by the American Diabetes Association in 2020 (44) .
Adjunctive Treatments
Adjunctive therapies are those which might be considered for complex diabetic foot wounds which fail to heal after 8-12 weeks of standard of care as discussed in the above sections. In recent years, many new such therapies, including skin substitutes, oxygen and other gases, products designed to correct abnormalities of wound biochemistry and cell biology associated with impaired wound healing, applications of cells, bioengineered skin and others, have been proposed to accelerate wound healing in the diabetic foot. Some years ago, an internationally conducted systemic review concluded that there was little published evidence from appropriately designed clinical trials to justify the use of such newer therapies (45).
However, there has been a renaissance in diabetic foot care with many RCTs of new therapies published since 2018 including topical therapies and oxygen-based treatments (46). A number of well-designed RCTs were published in 2018. The first proven therapy for neuro-ischemic ulcers, sucrose octasulfate dressings, was reported in the Explorer study (47). In the active group, 48% of wounds were closed after 20 weeks compared to 30% in the control dressing group (p<0.002). In the same issue of Lancet Diabetes Endocrinology, Game and colleagues reported the positive effect of the Leucopatch (3C Patch) device (a disc containing autologous platelets, leucocytes and fibrin) when applied to the surface of hard-to-heal foot ulcers (48).
Although, as noted above, the International Working Group on the Diabetic Foot (IWGDF) systematic review in 2016 (45) could not support the use of many of the therapies outlined above, this had changed by 2020 when three trials of placenta-derived products were considered (49). Although none was blinded, these were judged to be of low risk of bias as outcomes were assessed in a blinded manner. The first studied a cryo-preserved amniotic membrane allograft (50), the second an umbilical cord product (51), and the third a dehydrated amniotic membrane allograft (52): each showed significantly faster healing in the active treated group versus standard of care. Further details of all these studies referred to above can be found in the most recent American Diabetes Association (ADA) compendium on evidence-based management of complex diabetic foot wounds (53).
Hyperbaric and Topical Oxygen in the Diabetic Foot
HBO has been promoted as an effective treatment in diabetic foot wounds over many years (8). However, early RCTs have been criticized because of the small numbers of patients enrolled, and methodological and reporting inadequacies. A well designed and blinded RCT was conducted in Sweden some years ago suggesting the benefit of HBO in chronic neuro-ischemic infected foot ulcers with no possibility of revascularization (54). More recently, there have been two negative studies including a large retrospective cohort trial (55) and a multi-center Canadian study that showed no benefits of HBO whatsoever in any patient group (56). Thus, at present, the use of HBO in any diabetic foot wound has few data to support its efficacy and the multi-center trial from the Netherlands was also negative (57). The use of HBO in diabetic foot wounds was the topic of a recent debate (58).
There has been increasing interest in the use of topical oxygen-based therapies in wound healing in recent years. Whereas the latest studies of HBO have been negative, there have been interesting developments in the use of devices delivering topical oxygen. There is now evidence that both continuous (59) and cyclical (60) topical wound therapy may improve wound healing rates. A number of more recent studies now support the use of cyclical topical oxygen therapy (TWO2) (53) including some ‘real world’ data (61) and a number of meta-analyses and systematic reviews, the most recent of which has just been published (62). Thus, there is a body of evidence to support the use of TWO2 in the management of hard-to-heal diabetic foot ulcers that fail to respond to standard of care.
Negative Pressure Wound Therapy (NPWT)
The application of NPWT is believed to accelerate healing through reducing edema, removal of exudate, increased perfusion, self-proliferation, and the formation of granulation tissue (63). RCTs have suggested efficacy in rates of wound healing and reduced amputations, with the application of NPWT in both post-surgical and non-surgical chronic non-healing ulcers (64,65). A systematic review confirmed that there was some evidence to support the use of NPWT in post-operative wounds (49).
ADA Standards of Care and IWDGF Guidelines 2023
The ADA publishes its standards of care and clinical practice guidelines each January in Diabetes Care. In 2023 (66), those adjunctive therapies for foot ulceration recommended and supported by level A evidence (based on large, well-designed randomized controlled trials or well-done meta-analyses of randomized controlled trials) included: negative-pressure wound therapy, placental membranes, bioengineered skin substitutes, several acellular matrices, autologous fibrin and leukocyte platelet patches, and topical oxygen therapy. The IWDGF guidelines are renewed every four years, and in 2023, for adjunctive therapies for foot ulceration, recommended, with variable levels of strength and certainty of evidence, that the following might be considered (67): - regular sharp debridement (strength of recommendation: strong), sucrose-octasulfate impregnated dressings, hyperbaric oxygen in neuro-ischemic or ischemic diabetes-related foot ulcers, topical oxygen therapy, the autologous leucocyte, platelet and fibrin patch (Leucopatch or 3C Patch), placental derived products and Negative Pressure Wound Therapy (only as an adjunct therapy to standard of care for the healing of postsurgical diabetes-related foot wounds).
CHARCOT NEUROARTHROPATHY (CN)
Charcot neuroarthropathy, although uncommon, is a potentially devastating late complication of diabetic neuropathy (68). Although the exact mechanisms resulting in the development of CN remain unclear, much progress has been made in our understanding of the etiopathogenesis of this disorder over the last two decades. CN occurs in a well-perfused foot with both somatic and autonomic neuropathy: the patient presenting with acute CN tends to be slightly younger than is usual for those presenting with foot ulcers. A history of trauma may be present though may be missed because of the severe sensory loss. Although, in its pathogenesis, there are many unanswered questions, improved understanding in recent years of the role of inflammatory pathways might lead to new pharmacologic approaches in the acute phase of the condition. The outcomes in terms of management of CN have been generally poor because of ignorance that leads to delayed diagnosis.
Most important in the management of this condition is recognition of the acute Charcot foot. Any patient with known neuropathy who presents with a warm, swollen foot of unknown causation should be presumed to have acute CN until proven otherwise. Contrary to earlier reports, many patients may present with painful, difficult to describe symptoms in the affected foot despite significant neuropathy.
In its early stages, all investigations may be normal, including the foot x-ray. The role of the radiologist in the diagnosis of acute and chronic CN is discussed in the next section.
Role of Radiologist in in Diagnosing CN
As with acute osteomyelitis (see above), the initial radiographs in acute CN may appear (almost) normal, though it is common for soft tissue swelling to be present and radiographically visible, usually over the dorsum of the foot. It is consequently imperative that both the clinician and the radiologist are aware of the possibility of this condition being present. The first more specific radiographic feature is bone demineralization, usually subchondral or periarticular, around the joint(s) involved by the acute CN process (in contrast to acute osteomyelitis, where it is related to the ulcer location). Focal peri-articular fractures may then develop (Figure 5). If CN is suspected, despite non-diagnostic initial radiographs, then the options are to treat as acute CN (see below) and perform serial radiographs at one-to-two-week intervals until the diagnosis is confirmed or no longer clinically suspected, or treat similarly whilst arranging urgent radiological investigation with a more sensitive test (whilst repeating the radiographs if the further tests are delayed). CT scanning may show small avulsion fractures around midfoot articulations that are invisible on plain radiographs, with minimal increase in the sensitivity and specificity over the plain radiograph, but MR scanning (to include fat suppressed sequences) is better, demonstrating soft tissue edema, bone marrow edema and/or ligamentous disruption. If the MR scan shows no marrow signal abnormality in the foot, acute CN is unlikely. Where the appearances or clinical presentation are complex, with both osteomyelitis and acute CN being suspected, Indium labelled white cell scans and PET/CT have a role, though both can be false positive for osteomyelitis in the presence of acute CN. In infection, MR may demonstrate soft tissue abscesses or sinus tracks that may extend to the (infected) bone surface.
In chronic inactive CN, plain radiographs demonstrate the features of joint distension, destruction, dislocation, disorganization, debris, increased bone density (sclerosis) and deformity. On MR scanning, marrow edema of acute CN is replaced by low signal from sclerosis of the bone. Acute osteomyelitis superimposed on chronic CN produces a mixed picture requiring careful clinical-radiological review.
Diagnosis of acute Charcot neuroarthropathy remains a synthesis of high clinical awareness, clinical findings and radiological findings. The latter should always include serial plain radiography and, where necessary, MR scans.
An overview of imaging in the Charcot foot is available online (69).

Figure 5.
Acute Charcot neuroarthropathy. There is widening of the interosseous distance between the medial cuneiform and 2nd metatarsal (arrowheads), indicating disruption of the Lis-Franc ligament and a subtle flake fracture fragment (arrow).
Management of Charcot Neuroarthropathy
The treatment of CN depends upon the stage during which it is diagnosed. The essence of treatment in the acute phase remains non-weight bearing immobilization in a total contact or below-knee cast. Duration of treatment will depend upon response and it is recommended to continue casting until the temperature differential between the active and non-affected foot is down to approximately 1.5°C. As for the foot ulcer, it is recommended that treatment in a cast be continued for up to 4 weeks after the temperature differential has settled. At present, there are no proven medical or pharmacological approaches other than casting that have been shown to improve outcome. The management of advanced CN with bone deformity requiring reconstructive surgery is beyond the scope of this chapter and the reader is referred to a detailed review (70).
PREVENTION OF FIRST AND RECURRENT ULCERS
Prevention will only be successful with the early identification of those patients who have risk factors for foot ulceration. In the 1990s, the concept of the “annual review” was developed, and all those with diabetes should, at whatever stage, be screened for evidence of complications at least annually. The principle aim of such a review is to identify those with early signs of complications and institute appropriate management to prevent progression. The “Comprehensive Diabetic Foot Examination” (CDFE), was developed by a taskforce of the American Diabetes Association (ADA) that was charged with describing what should be included in the annual review for those at risk of foot complications (16). As noted above, the most important aspect of the annual foot review is the removal of shoes and socks with very careful inspection of both feet including between toes. Many neuropathic feet can be identified by this simple clinical observation, looking for features such as small muscle wasting, clawing of the toes, prominence of the metatarsal heads, distended dorsal foot pains (a sign of sympathetic autonomic neuropathy), dry skin, and callus formation. The key components of the diabetic foot annual examination are displayed in table 2.
The ADA Taskforce recommended that for evidence of neuropathy, that the perception of pressure using the 10g monofilament should be used at four sites in each foot (16). An additional test which might include a vibrating 128 Hz tuning fork or others outlined in table 2 should also be used to confirm any abnormality.
For the vascular assessment, foot pulse palpation is most important. Again, as noted above, the ankle brachial index may be falsely elevated in many people with diabetic neuropathy and therefore listening to the Doppler signal may be more helpful as may be a more detailed non-invasive vascular assessment.
More recently, other simple devices for clinical screening have been described. The simplest of all is the “Ipswich Touch Test” developed by Rayman et al in Ipswich, UK. This test simply assesses the ability of the patient to perceive the touch of a finger on the toes (71). The Vibratip which is a battery-operated disposable vibrating stylus can also be used to assess vibration sensation (72), and this has the advantage of using a forced-choice methodology. Both of these tests have been validated in clinical studies (71, 72).
Table 2.
Key Components of the Diabetic Foot Exam. Adapted from Boulton (16)
| Inspection Evidence of past/present ulcers? Foot shape? Prominent metatarsal heads/claw toes Hallux valgus Muscle wasting Charcot deformity Dermatological? Callus Erythema Sweating Dystrophic nails |
| Neurological 10g monofilament at 4 sites on each foot + 1 of the following: Vibration using 128 Hz tuning fork Pinprick sensation Ankle reflexes Vibration perception threshold |
| Vascular Foot pulses Ankle Brachial Index, if indicated Doppler wave forms, if indicated |
Prevention of Diabetic Foot Ulcers
Surprisingly, there is no evidence from RCTs to confirm the efficacy of preventative foot care education either in the prevention of first foot ulcers or of recurrent foot ulceration (73). This, however, should be interpreted as lack of evidence rather than evidence of no effect. For those patients with no foot ulcer history found to have any of the risk factors listed above or in table 2, they require education in foot self-care and regular podiatric attention.
With respect to secondary prevention, a RCT that looked at the effect of a foot care education program in those with a history of foot ulcers could provide no evidence that such a program of targeted education led to clinical benefit when compared to the usual care (74). It seems likely that those with a history of foot ulcers have such predominant physical abnormalities (e.g., foot deformity, loss of sensation, etc.) that education alone in self-foot care management is insufficient to prevent recurrent ulceration. It may be the combination of foot care education and an intervention that the individual can perform may be more effective. Lavery and colleagues, in studies supported by other RCTs demonstrated in an RCT that patients with a history of neuropathic foot ulcers who were randomized for self-foot temperature monitoring did demonstrate a reduced recurrent ulceration rate. All patients in the active group received foot care education and were provided with a skin thermometer which they used twice a day to check the temperatures of both feet. Those patients who discovered increased unilateral foot temperatures were advised to stop walking and see their health care professional. In the active group there was a highly significant reduction in recurrent foot ulceration (75): however, not all subsequent studies have confirmed this observation (76).
Important in the prevention of foot complications in diabetes is the team approach: members of the team commonly include the diabetes specialists, orthopedic and vascular surgeons, podiatrists, nurse educators, physiotherapists, pedorthists, and others. A study from one district in the UK was able to confirm a 62% reduction in major amputations over an 11-year follow-up period: this decrease occurred after the establishment of such a multi-disciplinary diabetic foot care team (77).
One of the impacts of the recent Covid-19 pandemic has been an explosion in the use of telemedicine and remote monitoring in the care of the diabetic foot (78). A number of studies are currently ongoing looking at “smart technology” in the prevention of recurrent diabetic foot ulcers. These include the use of sensors in socks or shoes to detect pressure change and also various devices to measure differentials in skin temperature: each of these might alert patients in the pre-ulcerative phase with the hope of preventing the actual ulcer from developing. It has now clearly been confirmed that a temperature differential of 2.2C between the feet using remote at home monitoring in patients at high risk of plantar ulceration is a strong predictor of ulcer development (79). Similarly, intelligent pressure sensing insole systems can reduce the incidence of plantar ulcers in those with a past history of ulceration (80). However, face to face consultations remain crucial in the screening for PAD and neuropathy in people with diabetes.
The Foot in Remission
As a recurrence is so common after the healing of neuropathic or neuro-ischemic foot ulcers, it has been suggested that those with a history of foot ulcers should be described as having “a foot in remission” rather than healed. This might better communicate risk of recurrence not only to the patient, but also other healthcare professionals (8). It is hoped that, as in cancers, aggressive treatment during the active disease together with a focus on improving care in “remission” can help to maximize patients’ function and of course improve quality of life (8,26) .
CONCLUSIONS
Although there has been much progress in our understanding of the etiopathogenesis and management of diabetic foot disorders over the last 30 years, much of what we use in clinical practice today still lacks an evidence-base. This is particularly true for example for dressings. The International Working Group on the Diabetic Foot has reported on the details required in the planning and reporting of intervention studies in the prevention and management of diabetic foot lesions (81). Details of the necessary trial design, conduct, and reporting should be taken into account when assessing published studies on interventions in the diabetic foot. Most important of all however in the management of patients with diabetic foot disorders, is to remember that the patient has frequently lost the “gift of pain” that protects most of us from developing significant foot problems but, when absent, can lead to devastating consequences.
REFERENCES
- 1.
- Boulton AJM, Vileikyte L, Ragnarson-Tennvall G, Apelqvist J. The global burden of diabetic foot disease. Lancet 2005; 366: 1719-24. [PubMed: 16291066]
- 2.
- Armstrong DG, Tan TW, Boulton AJM, Bus SA. Diabetic foot ulcers: a review. JAMA 2023; 330: 62-75. [PMC free article: PMC10723802] [PubMed: 37395769]
- 3.
- Lavery LA, Hunt NA, Ndip A, et al. Impact of chronic kidney disease on survival after amputation in individuals with diabetes. Diabetes Care 2010; 33: 2365-2369. [PMC free article: PMC2963496] [PubMed: 20739688]
- 4.
- Rogers LC, Lavery LA, Armstrong DG. The right to bear legs. J Am Podiatr Med Assoc 2008; 98: 166-168. [PubMed: 18348977]
- 5.
- Kerr M, Barron E, Chadwick P, et al. The cost of diabetic foot ulcers and amputations to the National Health Service in England. Diabetic Med 2019; 36: 995-1002. [PubMed: 31004370]
- 6.
- Skrepnek GH, Mills JL, Armstrong DG. Foot-in-Wallet Disease: tripped up by “cost-saving” reductions? Diabetes Care 2014; 37: 196-197. [PubMed: 25147261]
- 7.
- Boulton AJM. The diabetic lower limb – a forty-year journey: from clinical observation to clinical Science. Diabetic Medicine 2019; 36:1539-1549. Doi
.org/10.1111/dme.13901. [PubMed: 30659650] - 8.
- Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence. New Engl J Med 2017; 376: 2367-2375. [PubMed: 28614678]
- 9.
- Zhang Y, Lazzarini PA, McPhail SM, et al. Global disability burdens of diabetes-related lower-extremity complications in 1990 and 2016. Diabetes Care 2020; 43: 964-974. Doi: .10.2337/dc19-1614 [PubMed: 32139380] [CrossRef]
- 10.
- Abbott CA, Carrington AL, Ashe H, et al. The North-West Diabetes Foot Care Study: incidence of, and risk factors for new diabetic foot ulceration in a community-based patient cohort. Diabetic Med 2002; 19: 377-384. [PubMed: 12027925]
- 11.
- McDermott K, Fang M, Boulton AJM et al. Etiology, Epidemiology and Disparities in the Burden of Diabetic Foot Ulcers. Diabetes Care 2023; 46: 209-221. Doi: .10.2337/dci22-0043 [PMC free article: PMC9797649] [PubMed: 36548709] [CrossRef]
- 12.
- Joslin EP. The menace of diabetic gangrene. N Engl J Med 1934; 211: 16-20.
- 13.
- Young MJ, Breddy JL, Veves A, et al. The prediction of diabetic neuropathic foot ulceration using vibration perception thresholds: a prospective study. Diabetes Care 1994; 17: 557-560. [PubMed: 8082524]
- 14.
- Brown SJ, Handsaker JC, Bowling FL, et al. Diabetic peripheral neuropathy compromises balance during daily activities. Diabetes Care 2015; 38: 1116-22. [PubMed: 25765355]
- 15.
- Handsaker JC, Brown SJ, Bowling FL, et al. People with diabetic peripheral neuropathy display a decreased stepping accuracy during walking: potential implications for risk of tripping. Diabet Med 2016; 33: 644-649. [PubMed: 26172114]
- 16.
- Boulton AJM, Armstrong DG, Albert SF, et al. Comprehensive foot examination and risk assessment: a report of the taskforce of the Foot Care Interest Group of the American Diabetes Association, with endorsement by the American Association of Clinical Endocrinologists. Diabetes Care 2008; 31: 1679-1685. [PMC free article: PMC2494620] [PubMed: 18663232]
- 17.
- Reiber GE, Vileikyte L, Boyko EJ, et al. Causal pathways for incident lower-extremity ulcers in patients with diabetes from two settings. Diabetes Care 1999; 22: 157-162. [PubMed: 10333919]
- 18.
- Prompers L, Huijberts M, Apelqvist J, et al. High prevalence of ischemia, infection and serious comorbidity in patients with diabetic foot disease in Europe. Baseline results from the Eurodiale study. Diabetologia 2007; 50: 18-25. [PubMed: 17093942]
- 19.
- Hinchliffe RJ, Forsythe RO, Apelqvist J, et al. Guidelines on the diagnosis, prognosis and management of peripheral artery disease in patients with foot ulcers and diabetes. Diabetes Metab Res Rev 2020; 36 (suppl 1): e3276.doi.10.1002/dmrr.3276 [PubMed: 31958217] [CrossRef]
- 20.
- Forsythe RO, Hinchliffe RJ. Management of critical limb ischemia in the patient with diabetes. J Cardiovasc Surg (Torino) 2016; 57: 273-281. [PubMed: 26632661]
- 21.
- Mohammedi K, Woodward M, Hirakawa Y, et al. Microvascular and macrovascular disease and risk for major peripheral arterial disease in patients with type 2 diabetes. Diabetes Care 2016; 39: 1796-1803. [PubMed: 27456835]
- 22.
- Game FL, Chipchase SY, Hubbard R, et al. Temporal association between the incidence of foot ulceration and the start of dialysis in diabetes mellitus. Nephrol Dial Transplant 2006; 21: 3207-3210. [PubMed: 16877485]
- 23.
- Ndip A, Lavery LA, Lafontaine J, et al. High levels of foot ulceration and amputation risk in a multiracial cohort of diabetic patients on dialysis therapy. Diabetes Care 2010; 33: 878-880. [PMC free article: PMC2845045] [PubMed: 20067975]
- 24.
- Ndip A, Rutter MK, Vileikyte L, et al. Dialysis treatment is an independent risk factor for foot ulceration in patients with diabetes and stage 4 or 5 chronic kidney disease. Diabetes Care 2010; 33: 1811-1866. [PMC free article: PMC2909067] [PubMed: 20484126]
- 25.
- Barrado FC, Kuypers DK, Matricali GA. Charcot neuroarthropathy after simultaneous pancreas-kidney transplantation: risk factors, prevalence and outcome. Clin Transplant 2015; 29: 712-719. [PubMed: 26033225]
- 26.
- Vileikyte L, Pouwer F, Gonzalez JS. Psychosocial research in the diabetic foot: are we making progress? Diabetes Metab Res Rev 2020; 36 (suppl 1) e3257.doi.10.1002/dmrr3257 [PubMed: 31850665] [CrossRef]
- 27.
- Gonzalez JS, Vileikyte L, Ulbrecht JS, et al. Depression predicts first but not recurrent diabetic foot ulcers. Diabetologia 2010; 53: 2241-2248. [PubMed: 20556354]
- 28.
- Boulton AJM. Diabetic Neuropathy: is pain God’s great gift to mankind? Semin Vasc Surg 2012; 25: 61-65. [PubMed: 22817853]
- 29.
- Armstrong DG, Lavery LA, Harkless LB. Validation of a diabetic wound classification system. The contribution of depth, infection, and ischemia to risk of amputation. Diabetes Care 1998; 21: 855-859. [PubMed: 9589255]
- 30.
- Oyibo S, Jude EB, Tarawneh I, et al. A comparison of two diabetic foot ulcer classification systems: the Wagner and the University of Texas wound classification system. Diabetes Care 2001; 24: 84-88. [PubMed: 11194247]
- 31.
- Fitridge R, Chuter V, Mills JL et al. . The 2023 intersocietal IWGDF, ESVS, SVS guidelines on peripheral arterial disease in patients with diabetes and a foot ulcer. www
.iwgdfguidelines.org. 2023 - 32.
- Senneville E, Lipsky BA, Abbas ZG, et al. Diagnosis of infection in the foot in diabetes: a systematic review. Diabetes Metab Res Rev 2020; 36 (suppl 1): e3281.doi:.10.1002/dmrr3281 [PubMed: 32176440] [CrossRef]
- 33.
- Lam K, van Asten SA, Nguyen T, et al. Diagnostic accuracy of probe to bone to detect osteomyelitis in the diabetic foot: a systematic review. Clin Infect Dis 2016 63: 944-948. [PubMed: 27369321]
- 34.
- Katz IA, Harlan A, Miranda-Palma B, et al. A randomized trial of two irremovable offloading devices in the management of plantar neuropathic diabetic foot ulcers. Diabetes Care 2005; 28: 555-559. [PubMed: 15735187]
- 35.
- Jeffcoate WJ, Price PE, Phillips CJ, et al. Randomized controlled trial of the use of three dressing preparations in the management of chronic ulceration of the foot in diabetes. Health Technol Assess 2009; 13: 1-86. [PubMed: 19922726]
- 36.
- Nabuurs-Fransen MH, Sleegers R, Huijberts HS, et al. Total contact casting of the diabetic foot in daily practice: a prospective follow-up study. Diabetes Care 2005; 28: 243-247. [PubMed: 15677773]
- 37.
- Hinchliffe RJ, Brownrigg JR, Andros G, et al. Effectiveness of revascularization of the ulcerated foot in patients with diabetes and peripheral artery disease: a systematic review. Diabetes Metab Res Rev 2016; 32 (suppl 1): 136-144. [PubMed: 26342204]
- 38.
- Lipsky BA, Berendt AR, Cornia PB, et al. 2012 Infectious Diseases Society of America clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clin Infect Dis 2012; 54: e132-173. [PubMed: 22619242]
- 39.
- Ertugrul B, UcKay I, Schoni M, Peter-Riesch B, Lipsky BA. Management of diabetic foot infections in the light of recent literature and new international guidelines. Expert Rev Anti-Infect Ther 2020; Feb 19 Epub. [PubMed: 32052672]
- 40.
- Game FL, Jeffcoate WJ. Primary non-surgical management of osteomyelitis of the foot in diabetes. Diabetologia 2008; 51: 962-967. [PubMed: 18385975]
- 41.
- Lázaro-Martinez JL, Aragón-Sánchez J, Garcia-Morales C. Antibiotics versus conservative surgery for treating diabetic foot osteomyelitis: a randomized comparative trial. Diabetes Care 2014; 37: 789-795. [PubMed: 24130347]
- 42.
- Tone A, Nguyen S, Devemy F, et al. Six-week versus twelve-week antibiotic therapy for non-surgically treated diabetic foot osteomyelitis: a multicentre open-label controlled randomized study. Diabetes Care 2015; 38: 302-307. [PubMed: 25414157]
- 43.
- Li HK, Rombach I, Zambellas R, et al. OVIVA Trial collaborators. Oral Vs IntraVenous Antibiotics for bone and joint infection. N Engl J Med 2019; 380: 425-436. [PMC free article: PMC6522347] [PubMed: 30699315]
- 44.
- Boulton AJM, Armstrong DG, Hardman MJ, et al. Diagnosis and management of diabetic foot infections. Arlington (VA). American Diabetes Association 2020. [PubMed: 32105420]
- 45.
- Game FL, Apelqvist J, Attinger C, et al. Effectiveness of interventions to enhance healing of chronic ulcers of the foot in diabetes: a systematic review. Diabetes Metab Res Rev 2016; 32 (suppl 1): 154-168. [PubMed: 26344936]
- 46.
- Edmonds ME. A renaissance in diabetic foot care: new evidence-based treatments. Lancet Diabet Endocrinol 2018; 6: 837-838. [PubMed: 30243804]
- 47.
- Edmonds ME, Lázaro-Martinez JL, Alfayate-Garcia JM, et al. Sucrose octasulfate dressing versus control dressing in patients with neuroischemic diabetic foot ulcers (Explorer): an international, multicenter, double-blind, randomized controlled trial. Lancet Diabetes Endocrinol 2018; 6: 186-196. [PubMed: 29275068]
- 48.
- Game F, Jeffcoate W, Tarnow L, et al. LeucoPatch system for the management of hard-to-heal diabetic foot ulcers in the UK, Denmark, and Sweden: an observer-masked, randomized controlled trial. Lancet Diabetes Endocrinol 2018; 6; 870-878. [PubMed: 30243803]
- 49.
- Rayman G, Vas P, Dharariya K, et al. International Working Group on the Diabetic Foot (IWGDF). Guidelines on use of interventions to enhance healing of chronic foot ulcers in diabetes (IWGDF 2019 update). Diabetes Metab Res Rev 2020; 36 (suppl 1): 3283. [PubMed: 32176450]
- 50.
- Lavery LA, Fulmer J, Shebetka KA, et al. Grafix Diabetic Foot Ulcer Study Group. The efficacy and safety of Grafix for the treatment of chronic diabetic foot ulcers: results of a multi-centre, controlled, randomized, blinded, clinical trial. Int Wound J 2014; 11: 554-560. [PMC free article: PMC7951030] [PubMed: 25048468]
- 51.
- Tettelbach W, Cazzell S, Sigal F, et al. A multicentre prospective randomized controlled comparative parallel study of dehydrated human umbilical word (EpiCord) allograft for the treatment of diabetic foot ulcers. Int Wound J 2019; 16: 122-130. [PMC free article: PMC7380046] [PubMed: 30246926]
- 52.
- Tettelbach W, Cazzell S, Reyzelman AM, Sigal F, Caporusso JM, Agnew PS. A confirmatory study on the efficacy of dehydrated human amnion/chorion membrane dHACM allograft in the management of diabetic foot ulcers: a prospective, multicentre, randomized, controlled study of 110 patients from 14 wound clinics. Int Wound J 2019; 16: 19-29. [PMC free article: PMC7379535] [PubMed: 30136445]
- 53.
- Boulton AJM, Armstrong DG, Löndahl M, et al. New Evidence-Based Therapies for Complex Diabetic Foot Wounds. Arlington (VA) May 2022: American Diabetes Association. [PubMed: 35763580]
- 54.
- Löndahl M, Katzman P, Nilsson A, et al. Hyperbaric oxygen therapy facilitates healing of chronic foot ulcers in patients with diabetes. Diabetes Care 2010; 33: 998-1003. [PMC free article: PMC2858204] [PubMed: 20427683]
- 55.
- Margolis DJ, Gupta J, Hoffstad O, et al. Lack of effectiveness of hyperbaric oxygen therapy for the treatment of diabetic foot ulcer and the prevention of amputation: a cohort study. Diabetes Care 2013; 36: 1961-1966. [PMC free article: PMC3687310] [PubMed: 23423696]
- 56.
- Fedorko L, Bowen JM, Jones W, et al. Hyperbaric oxygen therapy does not reduce indications for amputation in patients with diabetes with non-healing ulcers of the lower limb: a prospective, double-blind, randomized controlled clinical trial. Diabetes Care 2016; 39; 392-399. [PubMed: 26740639]
- 57.
- Santema KTB, Stoekenbroek RM, Koelemay MJW, et al. Hyperbaric oxygen therapy in the treatment of ischemic lower-extremity ulcers in patients with diabetes: results of the DAMO2CLES multicenter randomized controlled trial. Diabetes Care 2018; 41: 112-119. [PubMed: 29074815]
- 58.
- Löndahl M, Boulton AJM. Hyperbaric oxygen: useless or useful? A debate. Diab Metab Res Rev 2020 Mar;36 Suppl 1:e3233. doi: .10.1002/dmrr.3233 [PubMed: 31927787] [CrossRef]
- 59.
- Niederauer MQ, Michalek JE, Liu Q, et al. Continuous diffusion of oxygen improves diabetic foot ulcer healing when compared with a placebo control: a randomized, double-blind, multicenter study. J Wound Care 2018; 27 (suppl 9): S30-S45. [PubMed: 30207844]
- 60.
- Frykberg RG, Franks PJ, Edmonds ME, et al. A multinational, multicenter, randomized, double-blinded, placebo-controlled trial to evaluate the efficacy of cyclical topical wound oxygen therapy (TWO2) in the treatment of chronic diabetic foot ulcers: the TWO2 study. Diabetes Care 2020; 43: 616-624. [PubMed: 31619393]
- 61.
- Yellin JI, Gaebler JA, Zhou FF, et al. Reduced hospitalizations and amputations in patients with diabetic foot ulcers treated with cyclical pressurized topical wound oxygen therapy: real-world outcomes. Adv Wound Care (New Rochelle). Online ahead of print on 6 December 2021 [PMC free article: PMC9527050] [PubMed: 34714167]
- 62.
- Carter MJ, Frykberg RG, Oropallo A, et al. Efficacy of topical oxygen therapy in healing chronic diabetic foot ulcers: systematic review and meta-analysis. Adv Wound Care 2023, Apr; 12 (4): 177-186. doi: .10.1089/wound.2022.0041 [PMC free article: PMC9885545] [PubMed: 35593010] [CrossRef]
- 63.
- Isaac AL, Armstrong DG. Negative pressure wound therapy and other new therapies for diabetic foot ulceration: the current state of play. Med Clin North Amer 2013; 97: 899-909. [PubMed: 23992900]
- 64.
- Armstrong DG, Lavery LA. Negative pressure wound therapy after partial diabetic foot amputation: a multicenter, randomized controlled trial. Lancet 2005; 366: 1704-1710. [PubMed: 16291063]
- 65.
- Blume PA, Walters J, Payne W, et al. Comparison of negative pressure wound therapy using vacuum-assisted closure with advanced moist wound therapy in the treatment of diabetic foot ulcers: a multicenter, randomized controlled trial. Diabetes Care 2008; 31: 631-636. [PubMed: 18162494]
- 66.
- El Sayed NA, Aleppo G, Aroda VR, et al. Retinopathy, Neuropathy and Foot Care: Standards of Care in Diabetes – 2023. Diabetes Care 2023; 46 (Suppl 1): S203-S215. doi: .10.2337/dc23-S012 [PMC free article: PMC9810462] [PubMed: 36507636] [CrossRef]
- 67.
- Chen P, Vilorio NC, Dhatariya K, et al: Guidelines on interventions to enhance healing of foot ulcers in people with diabetes (IWGDF 2023 update). Diab Metab Res Rev 2023; May 25; 3644 doi: .10.1002/dmrr.3644 [PubMed: 37232034] [CrossRef]
- 68.
- Jeffcoate WJ. Charcot foot syndrome. Diabetic Med 2015; 32: 760-770. [PubMed: 25818542]
- 69.
- Ergen FB, Sanverdi SE, Oznur A. Charcot foot in diabetes and an update on imaging. Diabetic Foot Ankle 2013; 4: .10.3402/dfa.V4i0.21884 [PMC free article: PMC3837304] [PubMed: 24273635] [CrossRef]
- 70.
- Shen W, Wukich D. Orthopedic surgery and the diabetic Charcot foot. Med Clin North Am 2013; 97; 873-882. [PubMed: 23992898]
- 71.
- Rayman G, Vas PR, Baker N, et al. The Ipswich Touch Test: a simple and novel method to identify inpatients with diabetes at risk of foot ulceration. Diabetes Care 2011; 34: 1517-1518. [PMC free article: PMC3120164] [PubMed: 21593300]
- 72.
- Bowling FL, Abbott CA, Harris WE. A pocket-sized disposable device for testing the integrity of sensation in the outpatient setting. Diabet Med 2012; 29: 1550-1552. [PubMed: 22672290]
- 73.
- Dorresteijn JA, Valk GD. Patient education for preventing diabetic foot ulceration. Diabetes Metab Res Rev 2012; 28 (suppl 1): 101-106. [PubMed: 22271733]
- 74.
- Lincoln NB, Radford KA, Game FL, et al. Education for secondary prevention of foot ulcers in people with diabetes: a randomized controlled trial. Diabetologia 2008; 51 1954-1961. [PubMed: 18758747]
- 75.
- Lavery LA, Higgins KR, Lanctot DR, et al. Preventing diabetic foot ulcer recurrence in high-risk patients: use of temperature monitoring as a self-assessment tool. Diabetes Care 2007; 30: 14-20. [PubMed: 17192326]
- 76.
- Aan de Stegge WB, van Netten JJ, Bus SA. Does the skin heat up before it breaks down in diabetic foot ulceration? Diabete Metab Res Rev 2023, 08 Feb 2023. [PubMed: 36752702]
- 77.
- Krishnan S, Nash F, Baker N, et al. Reduction in diabetic amputations over eleven years in a defined UK population: benefits of multidisciplinary teamwork and continuous prospective audit. Diabetes Care 2008; 31: 99-101. [PubMed: 17934144]
- 78.
- Boulton AJM. Diabetic Foot Disease during the Covid-19 pandemic. Medicina 2021; Jan 22; 57 (2): 97. [PMC free article: PMC7912054] [PubMed: 33499251]
- 79.
- Frykberg RG, Gordon IL. Reyzelman AM, et al. Feasibility and efficacy of a smart mat technology to predict development of diabetic plantar ulcers. Diabetes Care 2017; 40: 973-980.doi: .10.2337/dc16-2294 [PubMed: 28465454] [CrossRef]
- 80.
- Abbott CA, Chatwin KE, Foden P, et al. Innovative intelligent insole system reduces diabetic foot ulcer recurrence at plantar sites: a prospective, randomized, proof-of-concept study. Lancet Digit Health 2019; Oct 1 (6): e308-e318. [PubMed: 33323253]
- 81.
- Jeffcoate WJ, Bus SA, Game FL, et al. Reporting standards of studies and papers on the prevention and management of foot ulcers in diabetes: required details and markers of good quality. Lancet Diabetes Endocrinol 2016; 4: 781-788. [PubMed: 27177729]
- ABSTRACT
- INTRODUCTION
- EPIDEMIOLOGY OF THE DIABETIC FOOT
- ETIOPATHOGENESIS OF DIABETIC FOOT ULCERATION
- THE PATHWAY TO FOOT ULCERATION IN DIABETES
- FOOT ULCERATION
- CLASSIFICATION OF DIABETIC FOOT WOUNDS
- EVALUATION OF THE DIABETIC FOOT ULCER
- MANAGEMENT OF DIABETIC FOOT ULCERS
- CHARCOT NEUROARTHROPATHY (CN)
- PREVENTION OF FIRST AND RECURRENT ULCERS
- CONCLUSIONS
- REFERENCES
- Diagnosis and treatment of diabetic foot infections.[Plast Reconstr Surg. 2006]Diagnosis and treatment of diabetic foot infections.Lipsky BA, Berendt AR, Deery HG, Embil JM, Joseph WS, Karchmer AW, LeFrock JL, Lew DP, Mader JT, Norden C, et al. Plast Reconstr Surg. 2006 Jun; 117(7 Suppl):212S-238S.
- Poorly designed research does not help clarify the role of hyperbaric oxygen in the treatment of chronic diabetic foot ulcers.[Diving Hyperb Med. 2016]Poorly designed research does not help clarify the role of hyperbaric oxygen in the treatment of chronic diabetic foot ulcers.Mutluoglu M, Uzun G, Bennett M, Germonpré P, Smart D, Mathieu D. Diving Hyperb Med. 2016 Sep; 46(3):133-134.
- Review Diabetic neuropathy and foot complications.[Handb Clin Neurol. 2014]Review Diabetic neuropathy and foot complications.Boulton AJ. Handb Clin Neurol. 2014; 126:97-107.
- A Meta-Analysis of the Outcomes of Metatarsal Head Resection for the Treatment of Neuropathic Diabetic Foot Ulcers.[Adv Wound Care (New Rochelle)....]A Meta-Analysis of the Outcomes of Metatarsal Head Resection for the Treatment of Neuropathic Diabetic Foot Ulcers.Yammine K, Kheir N, Assi C. Adv Wound Care (New Rochelle). 2021 Feb; 10(2):81-90. Epub 2020 Sep 29.
- Review Systematic reviews of wound care management: (3) antimicrobial agents for chronic wounds; (4) diabetic foot ulceration.[Health Technol Assess. 2000]Review Systematic reviews of wound care management: (3) antimicrobial agents for chronic wounds; (4) diabetic foot ulceration.O'Meara S, Cullum N, Majid M, Sheldon T. Health Technol Assess. 2000; 4(21):1-237.
- The Diabetic Foot - EndotextThe Diabetic Foot - Endotext
Your browsing activity is empty.
Activity recording is turned off.
See more...
