4.1. INTRODUCTION
Withdrawal management (WM) refers to the medical and psychological care of patients who are experiencing withdrawal symptoms as a result of ceasing or reducing use of their drug of dependence.5
People who are not dependent on drugs will not experience withdrawal and hence do not need WM. Refer to the patient's assessment to determine if he or she is dependent and requires WM.
Patients who are opioid dependent and consent to commence methadone maintenance treatment do not require WM; they can be commenced on methadone immediately (see opioid withdrawal protocol for more information).
It is very common for people who complete withdrawal management to relapse to drug use. It is unrealistic to think that withdrawal management will lead to sustained abstinence. Rather, withdrawal management is an important first step before a patient commences psychosocial treatment.
Providing withdrawal management in a way that reduces the discomfort of patients and shows empathy for patients can help to build trust between patients and treatment staff of closed settings.
4.2. STANDARD CARE FOR WITHDRAWAL MANAGEMENT
Patients in withdrawal should be accommodated away from patients who have already completed withdrawal. Healthcare workers should be available 24 hours a day. Workers should include:
- A doctor who sees patients on admission and is on call to attend to the patient in case of complications;
- Nurses, who are responsible for monitoring patients in withdrawal, dispensing medications as directed by the doctor and providing the patient with information about withdrawal.
The WM area should be quiet and calm. Patients should be allowed to sleep or rest in bed if they wish, or to do moderate activities such as walking. Offer patients opportunities to engage in meditation or other calming practices.
Patients in withdrawal should not be forced to do physical exercise. There is no evidence that physical exercise is helpful for WM. Physical exercise may prolong withdrawal and make withdrawal symptoms worse.
Patients in withdrawal may be feeling anxious or scared. Offer accurate, realistic information about drugs and withdrawal symptoms to help alleviate anxiety and fears.
Do not try to engage the patient in counselling or other psychological therapy at this stage. A person in withdrawal may be vulnerable and confused; this is not an appropriate time to commence counselling.
During withdrawal some patients may become disruptive and difficult to manage. There may be many reasons for this sort of behaviour. The patient may be scared of being in the closed setting, or may not understand why they are in the closed setting. The patient may be disoriented and confused about where they are. In the first instance, use behaviour management strategies to address difficult behaviour (Table 2).
Table 2
Strategies for managing difficult behaviour.
Withdrawal symptoms vary according to the drug of dependence and severity of dependence, but often include nausea, vomiting, diarrhoea, anxiety and insomnia. Table 3 provides guidance on medications for alleviating common withdrawal symptoms.
Table 3
Symptomatic medications in withdrawal management.
4.3. WITHDRAWAL MANAGEMENT FOR OPIOID DEPENDENCE
Opioids are drugs such as heroin, opium, morphine, codeine and methadone. Opioid withdrawal can be very uncomfortable and difficult for the patient. It can feel like a very bad flu. However, opioid withdrawal is not usually life-threatening.
There are some patients who should NOT complete opioid withdrawal:
- Pregnant women: It is recommended that pregnant women who are opioid dependent do not undergo opioid withdrawal as this can cause miscarriage or premature delivery. The recommended treatment approach for pregnant, opioid dependent women is methadone maintenance treatment.
- Patients commencing methadone maintenance treatment do not need to undergo withdrawal before commencing treatment.
Opioid withdrawal syndrome
Short-acting opioids (e.g. heroin): Onset of opioid withdrawal symptoms 8-24 hours after last use; duration 4-10 days.
Long-acting opioids (e.g. methadone): Onset of opioid withdrawal symptoms 12-48 hours after last use; duration 10-20 days.
Symptoms include:
- Nausea and vomiting
- Anxiety
- Insomnia
- Hot and cold flushes
- Perspiration
- Muscle cramps
- Watery discharge from eyes and nose
- Diarrhoea
Observation and monitoring
Patients should be monitored regularly (3-4 times daily) for symptoms and complications. The Short Opioid Withdrawal Scale (SOWS, p.37) is a useful tool for monitoring withdrawal. It should be administered 1-2 times daily. Use the SOWS score to select an appropriate management strategy.
Table
Short Opioid Withdrawal Scale.
Add scores for total score:
Compare total score to table below to guide withdrawal management
Management of mild opioid withdrawal
Patients should drink at least 2-3 litres of water per day during withdrawal to replace fluids lost through perspiration and diarrhoea. Also provide vitamin B and vitamin C supplements.
Symptomatic treatment (see Table 3) and supportive care are usually sufficient for management of mild opioid withdrawal.
Management of moderate to severe opioid withdrawal
As for management of mild withdrawal, but with the addition of clonidine or opioid medications such as buprenorphine, methadone or codeine phosphate:
Opioid withdrawal management using clonidine
Clonidine is an alpha-2 adrenergic agonist. It can provide relief to many of the physical symptoms of opioid withdrawal including sweating, diarrhoea, vomiting, abdominal cramps, chills, anxiety, insomnia, and tremor. It can also cause drowsiness, dizziness and low blood pressure.
Clonidine should be used in conjunction with symptomatic treatment as required. It should not be given at the same time as opioid substitution.
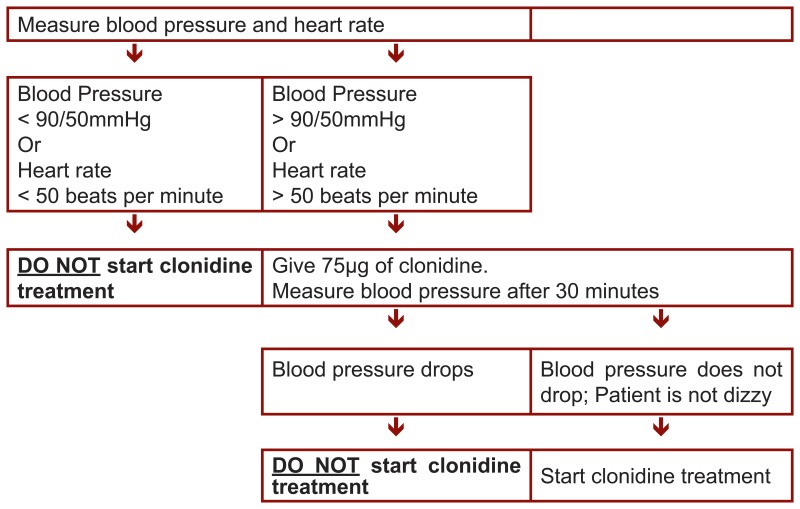
Measure the patient's blood pressure and heart rate before administering clonidine (Figure 2). Dose according to Table 4. Continue to monitor blood pressure and cease clonidine if blood pressure drops below 90/50mmHg.
Figure 2
Procedure for administering clonidine for moderate/severe opioid withdrawal.
Table 4
Clonidine dosing for moderate/severe opioid withdrawal.
Opioid withdrawal management using buprenorphine
Buprenorphine is the best opioid medication for management of moderate to severe opioid withdrawal. It alleviates withdrawal symptoms and reduces cravings.
Because of its pharmacological action (partial opiate agonist), buprenorphine should only be given after the patient begins to experience withdrawal symptoms (i.e. at least eight hours after last taking heroin).
Buprenorphine should be used with caution in patients with:
- Respiratory deficiency
- Urethral obstruction
- Diabetes
The dose of buprenorphine given must be reviewed on daily basis and adjusted based upon how well the symptoms are controlled and the presence of side effects. The greater the amount of opioid used by the patient, the larger the dose of buprenorphine required to control symptoms. A suggested dosing protocol is shown in Table 5. Symptoms that are not satisfactorily reduced by buprenorphine can be managed with symptomatic treatment as required (see Table 3).
Table 5
Buprenorphine for opioid withdrawal management.
Opioid withdrawal management using methadone
Methadone alleviates opioid withdrawal symptoms and reduces cravings. Methadone is useful for detoxification from longer acting opioids such as morphine or methadone itself.
Methadone should be used with caution if the patient has:
- Respiratory deficiency
- Acute alcohol dependence
- Head injury
- Treatment with monoamine oxidase inhibitors (MAOIs)
- Ulcerating colitis or Crohn's disease
- Severe hepatic impairment
The dose must be reviewed on daily basis and adjusted based upon how well the symptoms are controlled and the presence of side effects. The greater the amount of opioid used by the patient the greater the dose of methadone required to control withdrawal symptoms. A suggested dosing protocol is presented in Table 6. If symptoms are not sufficiently controlled either reduce the dose of methadone more slowly, or provide symptomatic treatment (see Table 3).
Table 6
Methadone for opioid withdrawal management.
To avoid the risk of overdose in the first days of treatment methadone can be given in divided doses, for example, give 30mg in two doses of 15mg morning and evening.
Opioid withdrawal management using codeine phosphate
Codeine phosphate alleviates opioid withdrawal symptoms and reduces cravings. Codeine has no effect for 2–10% of people.
Codeine phosphate should be used with caution if the patient has:
- Respiratory deficiency
- Severe hepatic impairment
The dose must be reviewed on daily basis and adjusted based upon how well the symptoms are controlled and the presence of side effects. The greater the amount of opioid used by the patient the greater the dose of codeine phosphate required to control withdrawal symptoms. A suggesting dosing protocol is shown in Table 7. Symptoms that are not satisfactorily reduced by codeine phosphate can be managed with symptomatic treatment as required (see Table 3).
Table 7
Codeine phosphate for opioid withdrawal management.
Follow-up care
Acute opioid withdrawal is followed by a protracted withdrawal phase that lasts for up to six months and is characterised by a general feeling of reduced well-being and strong cravings for opioids. This craving often leads to relapse to opioid use. To reduce the risk of relapse, patients should be engaged in psychosocial interventions such as described later in these guidelines. Patients who repeatedly relapse following withdrawal management are likely to benefit from methadone maintenance treatment or other opioid substitution treatment.
All opioid dependent patients who have withdrawn from opioids should be advised that they are at increased risk of overdose due to reduced opioid tolerance. Should they use opioids, they must use a smaller amount than usual to reduce the risk of overdose.
4.4. WITHDRAWAL MANAGEMENT FOR BENZODIAZEPINE DEPENDENCE
Benzodiazepines are central nervous system depressants. They are used to treat anxiety and sleeping disorders. When used appropriately they are very effective in treating these disorders. However, when used for an extended period of time (e.g. several weeks), dependence can develop.
Benzodiazepine withdrawal syndrome
Benzodiazepines can have short or long durations of action. This affects the onset and course of withdrawal.
Short-acting benzodiazepines include oxazepam, alprazolam and temazepam. Withdrawal typically begins 1-2 days after the last dose, and continues for 2-4 weeks or longer.
Long-acting benzodiazepines include diazepam and nitrazepam. Withdrawal typically begins 2-7 days after the last dose, and continues for 2-8 weeks or longer
Symptoms include:
- Anxiety
- Insomnia
- Restlessness
- Agitation and irritability
- Poor concentration and memory
- Muscle tension and aches
These symptoms tend to be subjective, with few observable signs.
Observation and monitoring
Patients in benzodiazepine withdrawal should be monitored regularly for symptoms and complications.
The severity of benzodiazepine withdrawal symptoms can fluctuate markedly and withdrawal scales are not recommended for monitoring withdrawal. Rather, the healthcare worker should regularly (every 3-4 hours) speak with the patient and ask about physical and psychological symptoms. Provide reassurance and explanation of symptoms as necessary.
Management of benzodiazepine withdrawal
The safest way to manage benzodiazepine withdrawal is to give benzodiazepines in gradually decreasing amounts. This helps to relieve benzodiazepine withdrawal symptoms and prevent the development of seizures.
The first step in benzodiazepine withdrawal management is to stabilise the patient on an appropriate dose of diazepam. Calculate how much diazepam is equivalent to the dose of benzodiazepine that the patient currently uses, to a maximum of 40mg of diazepam (Table 8).
Table 8
Calculating diazepam equivalent doses.
This dose of diazepam (up to a maximum of 40mg) is then given to the patient daily in three divided doses. Even if the patient's equivalent diazepam dose exceeds 40mg, do not give greater than 40mg diazepam daily during this stabilisation phase.
Allow the patient to stabilise on this dose of diazepam for 4-7 days. Then, for patients taking less than the equivalent of 40mg of diazepam, follow the low-dose benzodiazepine reducing schedule (Table 9). For patients taking the equivalent of 40mg or more of diazepam, follow the high-dose benzodiazepine reducing schedule (Table 10).
Table 9
Low-dose benzodiazepine reducing schedule.
Table 10
High-dose benzodiazepine reducing schedule.
The length of time between each dose reduction should be based on the presence and severity of withdrawal symptoms. The longer the interval between reductions, the more comfortable and safer the withdrawal. Generally, there should be at least one week between dose reductions.
Generally, benzodiazepine withdrawal symptoms fluctuate; the intensity of the symptoms does not decrease in a steady fashion as is the case with most other drug withdrawal syndromes. It is not recommended to increase the dose when symptoms worsen; instead, persist with the current dose until symptoms abate, then continue with the dose reduction schedule.
Symptomatic treatment can be used in cases where residual withdrawal symptoms persist (Table 3).
Follow-up care
Withdrawal management alone is unlikely to lead to sustained abstinence from benzodiazepines. The patient should commence psychosocial treatment as described in these guidelines.
Patients may have been taking benzodiazepines for an anxiety or other psychological disorder; following withdrawal from benzodiazepines, the patient is likely to experience a recurrence of these psychological symptoms. Patients should be offered psychological care to address these symptoms.
4.5. WITHDRAWAL MANAGEMENT FOR STIMULANT DEPENDENCE
Stimulants are drugs such as methamphetamine, amphetamine and cocaine. Although these drugs vary in their effects, they have similar withdrawal syndromes.
Stimulant withdrawal syndrome
Symptoms begin within 24 hours of last use of stimulants and last for 3-5 days.
Symptoms include:
- Agitation and irritability
- Depression
- Increased sleeping and appetite
- Muscle aches
People who use large amounts of stimulants, particularly methamphetamine, can develop psychotic symptoms such as paranoia, disordered thoughts and hallucinations. The patient may be distressed and agitated. They may be a risk of harming themselves or others. These symptoms can be managed using anti-psychotic medications and will usually resolve within a week of ceasing stimulant use.
Observation and monitoring
Patients withdrawing from stimulants should be monitored regularly. Because the mainstay of treatment for stimulant withdrawal is symptomatic medication and supportive care, no withdrawal scale has been included.
During withdrawal, the patient's mental state should be monitored to detect complications such as psychosis, depression and anxiety. Patients who exhibit severe psychiatric symptoms should be referred to a hospital for appropriate assessment and treatment.
Management of stimulant withdrawal
Patients should drink at least 2-3 litres of water per day during stimulant withdrawal. Multivitamin supplements containing B group vitamins and vitamin C are recommended. Symptomatic medications should be offered as required for aches, anxiety and other symptoms.
Management of severe agitation
A minority of patients withdrawing from stimulants may become significantly distressed or agitated, presenting a danger to themselves or others.
In the first instance, attempt behavioural management strategies as shown in Table 2 (page 33). If this does not adequately calm the patient, it may be necessary to sedate him or her using diazepam. Provide 10-20ng of diazepam every 30 minutes until the patient is adequately sedated. No more than 120mg of diazepam should be given in a 24-hour period. The patient should be observed during sedation and no more diazepam given if signs of respiratory depression are observed.
If agitation persists and the patient cannot be adequately sedated with oral diazepam, transfer the patient to a hospital setting for psychiatric care.
Follow-up care
Acute stimulant withdrawal is followed by a protracted withdrawal phase of 1-2 months duration, characterised by lethargy, anxiety, unstable emotions, erratic sleep patterns and strong cravings for stimulant drugs. These symptoms may complicate the patient's involvement in treatment and should be taken into account when planning treatment.
The preferred treatment for stimulant dependence is psychological therapy that focuses on providing patients with skills to reduce the risk of relapse (see Part 5: Psychosocial approaches to drug dependence treatment).
4.6. WITHDRAWAL MANAGEMENT FOR ALCOHOL DEPENDENCE
Alcohol withdrawal can be very difficult for the patient. In rare cases, alcohol withdrawal can be life-threatening and require emergency medical intervention. Hence, it is extremely important to assess patients for alcohol dependence and monitor alcohol dependent patients carefully.
Alcohol withdrawal syndrome
Alcohol withdrawal symptoms appear within 6-24 hours after stopping alcohol, are most severe after 36 – 72 hours and last for 2 – 10 days.
Symptoms include:
- Anxiety
- Excess perspiration
- Tremors, particularly in hands
- Dehydration
- Increased heart rate and blood pressure
- Insomnia
- Nausea and vomiting
- Diarrhoea
Severe withdrawal may involve complications:
- Seizures
- Hallucinations
- Delirium
- Extreme fluctuations in body temperature and blood pressure
- Extreme agitation
Observation and monitoring
Patients should be monitored 3-4 times daily for symptoms and complications. The Alcohol Withdrawal Scale (AWS, p.49) should be administered every four hours for at least three days, or longer if withdrawal symptoms persist. A patient's score on the AWS should be used to select an appropriate management plan from below.
Table
Alcohol Withdrawal Scale.
Compare score to table below for suggested management
Management of mild alcohol withdrawal (AWS score 1-4)
Patients should drink 2-4 litres of water per day during withdrawal to replace fluids lost through perspiration and diarrhoea. Multivitamin supplements and particularly vitamin B1 (thiamine) supplements (at least 100mg daily during withdrawal) should also be provided to help prevent cognitive impairments9 that can develop in alcohol dependent patients.
Provide symptomatic treatment (see Table 3) and supportive care as required.
Management of moderate alcohol withdrawal (AWS score 5-14)
As for management of mild alcohol withdrawal, with diazepam as in Table 11.
Table 11
Diazepam for management of moderate alcohol withdrawal.
If the protocol in Table 11 does not adequately control alcohol withdrawal symptoms, provide additional diazepam (up to 120mg in 24 hours). Monitor the patient carefully for excessive sedation. Once symptoms are controlled, follow the protocol as above.
Management of severe alcohol withdrawal (AWS score 15+)
As for management of mild alcohol withdrawal, but patients in severe alcohol withdrawal also require diazepam sedation. This may involve very large amounts of diazepam, many times greater than would be prescribed for patients in moderate alcohol withdrawal.
Give 20mg diazepam by mouth every 1-2 hours until symptoms are controlled and AWS score is less than 5. Monitor the patient regularly during this time for excessive sedation.
In rare cases, alcohol dependent patients may experience severe complications such as seizures, hallucinations, dangerous fluctuations in body temperature and blood pressure, extreme agitation and extreme dehydration. These symptoms can be life-threatening. As above, provide 20mg diazepam every 1-2 hours until symptoms are controlled. Be aware that very large doses of diazepam may be needed for this. In cases of severe dehydration, provide intravenous fluids with potassium and magnesium salts.
Follow-up care
Withdrawal management rarely leads to sustained abstinence from alcohol. After withdrawal is completed, the patient should be engaged in psychosocial interventions such as described in Section 5.
Patients with cognitive impairments as a result of alcohol dependence should be provided with ongoing vitamin B1 (thiamine) supplements.
4.7. WITHDRAWAL MANAGEMENT FOR INHALANT DEPENDENCE
Inhalant dependence and withdrawal is poorly understood. Some people who use inhalants regularly develop dependence, while others do not. Among heavy users, only some will experience withdrawal symptoms.
Inhalant withdrawal syndrome
Inhalant withdrawal symptoms can begin anywhere between a few hours to a few days after ceasing inhalant use. Symptoms may last for only 2-3 days, or may last for up to two weeks.
Symptoms include:
- Headaches
- Nausea
- Tremors
- Hallucinations
- Insomnia
- Lethargy
- Anxiety and depressed mood
- Irritability
- Poor concentration
Observation and monitoring
Patients withdrawing from inhalants should be observed every three-four hours to assess for complications such as hallucinations, which may require medication.
Management of inhalant withdrawal
Patients should drink 2-3 litres of water per day while in withdrawal. Provide a calm, quiet environment for the patient. Offer symptomatic medication as required for symptoms such as headaches, nausea and anxiety (Table 3).
Follow-up care
For up to a month after ceasing inhalant use, the patient may experience confusion and have difficulty concentrating. This should be taken into consideration in planning treatment involvement.
4.8. WITHDRAWAL MANAGEMENT FOR CANNABIS DEPENDENCE
Cannabis withdrawal syndrome
The cannabis withdrawal syndrome is typically mild, but can be difficult for the patient to cope with. Symptoms last between one and two weeks.
Symptoms include:
- Anxiety and a general feeling of fear and dissociation
- Restlessness
- Irritability
- Poor appetite
- Disturbed sleep, sometimes marked by vivid dreams
- Gastrointestinal upsets
- Night sweats
- Tremor
Observation and monitoring
Patients should be observed every three to four hours to assess for complications such as worsening anxiety and dissociation, which may require medication.
As cannabis withdrawal is usually mild, no withdrawal scales are required for its management.
Management of cannabis withdrawal
Cannabis withdrawal is managed by providing supportive care in a calm environment, and symptomatic medication as required (Table 3).
There is some evidence that lithium carbonate may be an effective medication for cannabis withdrawal management. However, until further research has established the efficacy of the medication for this purpose, it is not recommended for use in closed settings.
Follow-up care
The preferred treatment for cannabis dependence is psycho-social care. Patients who have been using large amounts of cannabis may experience psychiatric disturbances such as psychosis; if necessary, refer patients for psychiatric care.
Footnotes
- 5
The term ‘withdrawal management’ (WM) has been used rather than ‘detoxification’. This is because the term detoxification has many meanings and does not translate easily to languages other than English.
- 9
Known as Wernicke's Encephalopathy.
Publication Details
Copyright
All rights reserved.
Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel: +41 22 791 2476; fax: +41 22 791 4857; e-mail: tni.ohw@sredrokoob). Requests for permission to reproduce WHO publications, in part or in whole, or to translate them – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: tni.ohw@snoissimrep). For WHO Western Pacific Regional Publications, request for permission to reproduce should be addressed to Publications Office, World Health Organization, Regional Office for the Western Pacific, P.O. Box 2932, 1000, Manila, Philippines, fax: +632 521 1036, e-mail: tni.ohw.orpw@snoitacilbup
Publisher
World Health Organization, Geneva
NLM Citation
Clinical Guidelines for Withdrawal Management and Treatment of Drug Dependence in Closed Settings. Geneva: World Health Organization; 2009. 4, Withdrawal Management.