Included under terms of UK Non-commercial Government License.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Lenney W, McKay AJ, Tudur Smith C, et al.; MASCOT Study Group. Management of Asthma in School age Children On Therapy (MASCOT): a randomised, double-blind, placebo-controlled, parallel study of efficacy and safety. Southampton (UK): NIHR Journals Library; 2013 Feb. (Health Technology Assessment, No. 17.4.)

Management of Asthma in School age Children On Therapy (MASCOT): a randomised, double-blind, placebo-controlled, parallel study of efficacy and safety.
Show detailsGeneral Information
This document describes the MASCOT trial and provides information about procedures for entering patients into it. The protocol should not be used as an aide-memoir or guide for the treatment of other patients; every care was taken in its drafting, but corrections or amendments may be necessary. These will be circulated to the registered investigators in the trial, but centres entering patients for the first time are advised to contact the coordinating centre (Medicines for Children Research Network Clinical Trials Unit [MCRN CTU], Liverpool [ku.gro.utcnrcm@tocsam]) to confirm they have the most up to date version. Clinical problems relating to this trial should be referred to the relevant chief investigator via the MCRN CTU.
Statement of Compliance
This study will be carried out in accordance with the World Medical Association Declaration of Helsinki (1964) and the Tokyo (1975), Venice (1983), Hong Kong (1989) and South Africa (1996) amendments and will be conducted in compliance with the protocol, MCRN CTU Standard Operating Procedures and EU Directive 2001/20/EC, transposed into UK law as the UK Statutory Instrument 2004 No 1031: Medicines for Human Use (Clinical Trials) Regulations 2004 and amendments.
As per the MCRN CTU Standard Operating Procedures no waivers from the MASCOT protocol will be granted.
Contact Details: Institutions
| Co-Sponsors: | Clinical Trials Unit: | DNA Storage Facility: |
|---|---|---|
| Keele University Research Services | Medicines for Children Clinical Trials Unit | Prof Munir Pirmohamed |
| Room DH 1.13 | (Director: Professor Paula Williamson) | Dept. Of Pharmacology & Therapeutics |
| Dorothy Hodgkin Building | Institute of Child Health | The University of Liverpool |
| Keele University | Alder Hey Children's NHS Foundation Trust | Ashton Street |
| Keele | Eaton Road | Liverpool |
| Staffordshire | Liverpool | L69 3GE |
| Tel: 01782 733 374 | L1 2 2AP | Tel: 0151 794 5549 |
| Fax: 01782 733 740 | Tel: 0151 282 4729 | Fax: 0151 794 5540 |
| University Hospital of North Staffordshire NHS Trust Research & Development Department | Fax: 0151 282 4721 | Email: ku.ca.looprevil@prinum |
| North Staffordshire Medical Institute | Email: ku.gro.utcnrcm@tocsam | |
| Hartshill Road | ||
| Hartshil | ||
| Stoke-on-Trent | ||
| ST4 7QB | ||
| Tel: 01782 554 839 | ||
| Fax: 01782 554 610 | ||
| Clinical Trial Supplies Company | ||
| Aptuit Ltd | ||
| Unit 107 | ||
| Tenth Avenue | ||
| Deeside Industrial Park | ||
| Deeside | ||
| Flintshire | ||
| CH5 2UA | ||
| Tel: 01244 84 5723 | ||
| Fax: 01244 84 5701 | ||
| Email: moc.tiutpa@nagnal.navi | ||
Details of participating sites can be found in Appendix A
Contact Details: Individuals
| Individual/s Authorised to Sign the Protocol and Protocol Amendments on behalf of the Co-Sponsors: | Chief investigator (CI): | Medical Expert who will Advise on Safety Reports in the Absence of the CI: |
|---|---|---|
| Dr Darren Clement | Professor Warren Lenney | Professor David Price |
| Research & Development Manager Research & Development Department | Consultant Paediatrician/Professor of Paediatrics | GPIAG Professor of Primary Care Respiratory Medicine |
| University Hospital of North Staffordshire NHS Trust | Research & Development Department | Dept of General Practice and Primary Care |
| Guy Hilton Research Centre | University Hospital of North Staffordshire | University of Aberdeen Foresterhill Health Centre |
| Thornburrow Drive | North Staffordshire Medical Institute | Westburn Road |
| Stoke-on-Trent | Hartshill Road | Aberdeen |
| ST4 7QB | Stoke-on-Trent | AB25 2AY |
| Tel: 01782 554 839 | ST4 7QB | Tel: 020 71931876 |
| Fax: 01782 747 319 | Tel: 01782 554839 | Aberdeen office fax: 01224 550683 |
| E-mail: ku.shn.snhu@tnemelc.nerraD | Fax: 01782 412236 | Email: gro.hcraeseryrotaripser@divad |
| Ms Judith Garside | Email: ku.shn.snhu@yennel.nerraw | |
| Research Grants and Contracts Manager | ||
| Research Services | ||
| Room DH 1.13 | ||
| Dorothy Hodgkin Building | ||
| Keele University | ||
| Keele | ||
| Staffordshire | ||
| ST5 5BG | ||
| Tel: 01782 733 374 | ||
| Fax: 01782 733 740 | ||
| E-mail: ku.ca.eleek.osu@edisrag.m.j | ||
| Head of Health Economics: | Head of Trial Management: | Head of Statistics: |
| Professor Marilyn James | Ms Helen Hickey | Dr Catrin Tudur-Smith |
| Professor of Applied Health Economics | Medicines for Children Clinical Trials Unit | Medicines for Children Clinical Trials Unit |
| Liverpool John Moores University and Liverpool Primary Care Trust Centre for Public Health | Institute of Child Health | Institute of Child Health |
| 5th Floor Kingsway House | Alder Hey Children's NHS Foundation Trust | Alder Hey Children's NHS Foundation Trust |
| Hatton Garden | Eaton Road | Eaton Road |
| Liverpool | Liverpool | Liverpool |
| L3 2AJ | L12 2AP | L12 2AP |
| Tel: 0151 231 8783 | Tel: 0151 252 5240 | Tel: 0151 794 4059 |
| Fax: 0151 231 8020 | Fax: 0151 282 4721 | Fax: 0151 282 4721 |
| Email: ku.ca.umjl@semaj.m | Email: ku.gro.utcnrcm@tocsam | Email: ku.gro.utcnrcm@tocsam |
| Health Economist: | Trial Manager: | Trial Statistician: |
| Ms Elizabeth Stokes | Miss Sophie Perry | To be appointed |
| Research Assistant in Applied Health Economics | Medicines for Children Clinical Trials Unit | Medicines for Children Clinical Trials Unit |
| Liverpool John Moores University | Institute of Child Health | Institute of Child Health |
| Centre for Public Health | Alder Hey Children's NHS Foundation Trust | Alder Hey Children's NHS Foundation Trust |
| 5th Floor Kingsway House | Eaton Road | Eaton Road |
| Hatton Garden | Liverpool | Liverpool |
| Liverpool | L12 2AP | L12 2AP |
| L3 2AJ | Tel: 0151 282 4706 | Tel: 0151 282 4706 |
| Tel: 0151 231 8783 | Fax: 0151 282 4721 | Fax: 0151 282 4721 |
| Fax: 0151 231 8020 | Email: ku.gro.utcnrcm@tocsam | Email: ku.gro.utcnrcm@tocsam |
| Email: ku.ca.umjl@sekotS.A.E | ||
| Data Manager: | ||
| Miss Emma Dyson | ||
| Medicines for Children Clinical Trials Unit | ||
| Institute of Child Health | ||
| Alder Hey Children's NHS Foundation Trust | ||
| Eaton Road | ||
| Liverpool | ||
| L12 2AP | ||
| Tel: 0151 282 4705 | ||
| Fax: 0151 282 4721 | ||
| Email: ku.gro.utcnrcm@tocsam |
Contact Details: Independent Oversight Committees
| Trial Steering Committee (TSC) | ||
|---|---|---|
| Chair | Medical Experts | Statistician |
| Dr Anne Thomson | Dr Gary Connett | Prof Chris Frost |
| Consultant in Paediatric Respiratory Medicine & General Paediatrics | Consultant in Paediatric Respiratory Medicine | Professor of Medical Statistics |
| Oxford Children's Hospital | Department of Paediatrics | Room 142b Keppel Street |
| The John Radcliffe | Southampton General Hospital | London |
| Headington | Tremona Road | WC1E 7HT |
| Oxford | Southampton | Tel: 020 7 927 2242 |
| OX3 9DU | SO16 6YD | E-mail: ku.ca.mthsl@tsorf.sirhc |
| Tel: 01865 234199 | Tel: 02380 798973 | |
| Email: ku.ca.xo.scirtaideap@nosmoht.enna | Email: ku.shn.tsews.thus@ttennoC.yraG | |
| Dr Iolo Doull | ||
| Consultant Respiratory Paediatrician | ||
| Childrens Hospital for Wales | ||
| Heath Park | ||
| Cardiff | ||
| CF14 4XW | ||
| Tel: 029 2074 3530 | ||
| Email: ku.ca.fc@jilluod | ||
| Lay Representatives | ||
| Mr & Mrs John Hilton | ||
| The Guy Hilton Asthma Trust | ||
| Lyme House | ||
| Devils Lane | ||
| Longsdon | ||
| Stoke-on-Trent | ||
| ST9 9QP | ||
| Tel: 01538 385479 | ||
| Email: moc.dlrownepotb@tsurtsyug | ||
| Independent Data & Safety Monitoring Committee (IDSMC) | ||
|---|---|---|
| Chair | Medical Expert | Statistician |
| Dr David Spencer | Dr John Alexander | Mr Andy Vail |
| Consultant in Paediatric Respiratory Medicine | Consultant Paediatrician | Senior Lecturer and Statistician |
| The Regional Cardiothoracic Centre | Paediatric Intensive Care Unit | Research and Development Department |
| The Freeman Hospital | City General Hospital | Clinical Sciences Building |
| High Heaton | Stoke-on-Trent | Salford Royal Hospitals NHS Trust |
| Newcastle upon Tyne Tyne and Wear | ST4 6QG | Stott Lane |
| NE7 7DN | Tel: 01782 552 751 | Salford |
| Email: ku.shn.yhtron.htun@2recneps.divad | Email: ku.shn.snhu@rednaxelA.nhoJ | M6 8HD |
| Tel: 0161 206 4262 | ||
| Email: ku.ca.retsehcnam@liaV.ydnA | ||
List of abbreviations
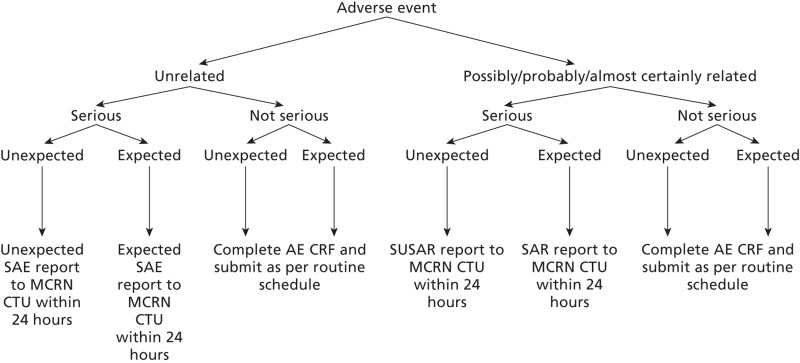
- AE
Adverse Event
- AR
Adverse Reaction
- CI
Chief Investigator
- CRF
Case Report Form
- CTU
Clinical Trials Unit
- GP
General Practitioner
- IB
Investigator's Brochure
- ICS
Inhaled Cortico-steroids
- IDSMC
Independent Data and Safety and Monitoring Committee
- IEC
Independent Ethical Committee
- IMP
Investigational Medicinal Product
- LREC
Local Research Ethics Committee
- MCRN CTU
Medicines for Children Clinical Trials Unit
- MREC
Main Research Ethics Committee
- PI
Principal Investigator
- R&D
Research & Development
- SAE
Serious Adverse Event
- SAR
Serious Adverse Reaction
- SPC
Summary of product characteristics
- SUSAR
Suspected Unexpected Serious Adverse Reaction
- TSC
Trial Steering Committee
- UAR
Unexpected Adverse Reaction
1. PROTOCOL SUMMARY
Title
Management of Asthma in School-age Children On Therapy
Phase
IV
Population
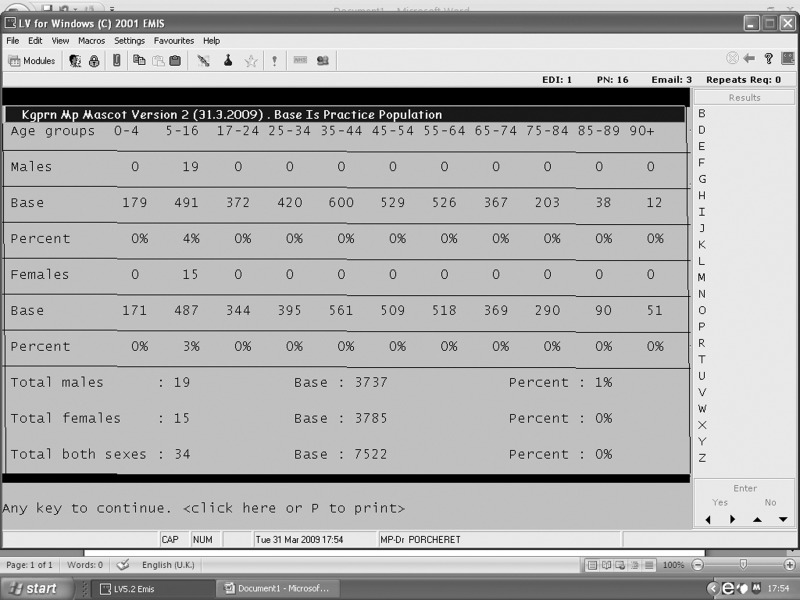
The target population will be children (aged 6–14 years) requiring frequent short-acting beta-2 agonist relief therapy ≥ 7 puffs per week and with asthma symptoms resulting in nocturnal awakening and/or compromised or reduced activity/exercise and/or those who have had exacerbations (defined as a short course of oral corticosteroids, an unscheduled GP or A&E Department visit or a hospital admission within the previous 6 months).
Number of Sites
13 secondary care and associated general practices throughout the United Kingdom. Site details are listed in Appendices A.
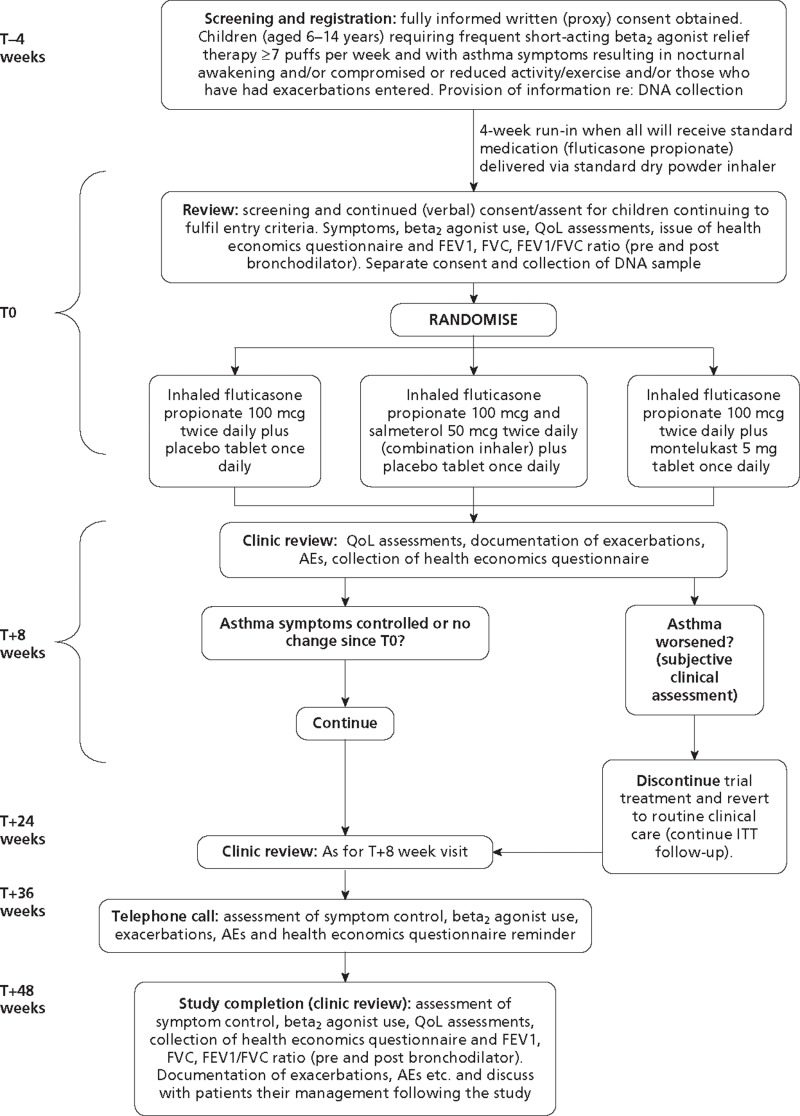
Study Duration
Total study duration for each randomised child is 52 weeks, comprising a 4-week run-in when all will be prescribed standard medication. Those continuing to fulfil eligibility criteria and giving informed consent after 4 weeks will be randomised (designated as time T0) and have follow-up reviews at T+8, T+24, T+36 and T+48 weeks.
Description of Agent/Intervention
All patients recruited into the study will undergo a 4-week run-in period when they will be provided with information about asthma and its management and prescribed the same low-dose inhaled corticosteroid, fluticasone propionate, in the dose of 100 micrograms twice daily. After 4 weeks, those that are eligible will be randomised to one of the following three regimen:
- Inhaled fluticasone propionate 100 micrograms twice daily plus placebo tablet once daily
- Inhaled fluticasone propionate 100 micrograms and salmeterol 50 micrograms twice daily (combination inhaler) plus placebo tablet once daily
- Inhaled fluticasone propionate 100 micrograms twice daily plus montelukast 5-mg tablet once daily.
The allocated treatment will be double-blinded, achieved by using identical inhalers and placebo tablets.
Objectives
Primary
The main research objective is to determine, in 6–14 year old children with asthma, uncontrolled on low-dose ICS, whether their control can be improved by adding in a long-acting beta-2 agonist (salmeterol) or a leukotriene receptor antagonist (montelukast) as measured by a reduced number of exacerbations requiring treatment with oral corticosteroids over the 48 week study period.
2. BACKGROUND INFORMATION
2.1. Introduction
Respiratory disease has recently been declared a target for improved management by the Department of Health. Although the major burden of chest diseases is in the adult population, it is accepted that the majority of adult chest diseases originates in childhood. The longitudinal studies from Aberdeen1 have shown that 60% of adults with asthma suffered their first symptoms in early childhood, continuing with these through later childhood and into adult life.
2.2. Rationale
Asthma remains the most common medical condition seen in children in primary care and the most frequent cause for medical paediatric hospital admission. It affects 1 in 8 children nationwide, approximately 50% of whom are prescribed low-dose inhaled corticosteroids (ICS). When treatment with low-dose ICS fails to control asthma symptoms, the National Guidelines2 suggest ensuring compliance, maximising inhaler technique and giving appropriate information about the disease to children and their families. Once these measures have been established and if asthma symptoms persist, the Guidelines recommend changing the treatment (Step 3 of the National Guidelines). The evidence at this step of the Guidelines is much weaker in children than it is in adults. The reasons for this are that few studies have been undertaken in children and most that have taken place have used adult-based outcomes such as lung function measurements. This is unsatisfactory because we know that as a chronic disease entity asthma in children is much more variable than in adults and between periods of symptoms, lung function is often normal. Pharmaceutical company studies have really only been conducted as part of their requirements to obtain a license to market their product. These studies have generally been of short-term duration. They have not added to clinicians' understanding of how and where to use the medications3,4. They have not necessarily selected a representative population due to their entry criteria and their intensive study requirements. Such requirements mean that ‘real-life’ compliance does not occur. In the independent National Dutch Study5 which attempted to enter patients uncontrolled on low-dose ICS, three treatment groups were employed: inhaled corticosteroids alone, inhaled corticosteroids in double the dose and inhaled corticosteroids + a long-acting beta2 agonist. There was essentially no difference in outcome measures between the three treatment groups as once again the primary outcome measure was that of lung function (FEV1). Comparing this study with a similar adult study6 both of which used lung function as the primary outcome measure, the mean FEV1 on entry into the paediatric study was approximately 89% expected for the children's heights. In the adult study the mean FEV1 on entry into the study was 74% expected. It is therefore not surprising that the paediatric study was unable to show any differences between the treatment groups.
We do not have the scientific information about how to treat children with asthma who are not well controlled on low-dose ICS therapy. It used to be recommended that when low-dose ICS were not effective their dose should be doubled. Studies in children, however, have investigated this statement and the results are not impressive7. There is no scientific evidence that when control is poor in children with asthma, the dose of the inhaled steroid should be increased. We have therefore decided not to introduce into this study a treatment limb with a higher ICS dosage. There is anecdotal information, however, from many studies undertaken within the pharmaceutical industry that when children enter a study which is controlled and double-blind in nature, up to 30% of them improve, their symptoms reduce and their lung function increases8. It is therefore surprising that approximately one third of children receiving ICS are prescribed high-dose inhaled steroid therapy (≥ 800 micrograms and unlicensed beclometasone dipropionate or equivalent) or they are commenced on ‘add-on’ therapies such as long-acting beta2 agonists (LABA) or leukotriene receptor antagonists (LTRA) in addition to low-dose ICS. Concerns about the safety of high-dose ICS have been raised in relation to growth impairment9, hypoglycaemia10 and suppression of the adrenal cortex11 resulting in warnings on prescribing from the Medicines & Healthcare Products Regulatory Agency (MHRA) in the UK12 and from the Food and Drug Administration (FDA) in the USA. It is therefore unacceptable that approximately one third of children with asthma are being treated with the above regimes. Asthma is a very common condition and the worth of these regimes has not been proven by appropriately devised paediatric studies. The National Guidelines have been developed in a ‘stepwise’ manner, the amount of medication increasing at each step if symptoms are not controlled.
However, as stated above, it may be that childhood asthma differs from that in adults. It seems that relatively poorly controlled asthma in children who exhibit frequent symptoms do not necessarily show abnormal lung function between their periods of symptoms. It is for this reason that in our study we will be concentrating on outcome measures such as exacerbations and quality of life although we will have the opportunity to measure spirometric values at the first (T0) and last (T48) visits in the randomised part of the study. It could be that an increase in medication may only be needed for a short time in children with asthma and there have been suggestions that once control is achieved children should have their add-on therapy reviewed. To incorporate such a step within the present study would make it excessively complicated and would have major implications on the number of patients included. The inclusion of such a step would make the study impractical within the UK. A study is needed which is simple, pragmatic (but placebo-controlled and double-blinded), has outcomes which will be of practical benefit to children and will provide evidence for the use of add-on medications in the most cost effective and efficient way.
Children dislike exacerbations. School attendance, daily activity and general well-being increase when asthma is well controlled. Once families understand sufficiently about asthma, inhaler technique has been evaluated and optimised, and compliance issues addressed, one of the reasons why a specific medication may be less effective could be related to the genetic make-up of the patient. In this study we will have the opportunity, through a separate consent process, to collect and store DNA specimens from saliva for later analysis of specific genetic polymorphisms in relation to asthma severity and outcome. This aspect will bring added value to the study.
2.3. Objectives
Primary Objective
To determine, in 6–14 year old children with asthma uncontrolled on low-dose ICS, whether their control can be improved by adding in a long-acting beta2 agonist (salmeterol) or a leukotriene receptor antagonist (montelukast) as measured by a reduced number of exacerbations requiring treatment with oral corticosteroids over the 48 week study period.
2.4. Potential Risks and Benefits
The medications used in this study are subject to Marketing Authorisations and are to be prescribed in accordance with their licensed indications. The management of any symptoms or exacerbations will be in accordance with usual clinical practice and a research worker, either the local principal investigator (PI) or research nurse (RN), will be available throughout the study to discuss specific issues with individuals concerned. Any concerns which cannot be satisfied at a local level will be forwarded to the chief investigator via the MASCOT Trial Coordinator based at the Medicines for Children Research Network Clinical Trials Unit (MCRN CTU). Any patient can withdraw from the study at any time with no detriment to their future care. All ethical aspects of the study will be discussed when informed written consent is obtained. Appropriate patient and family information leaflets have been developed and are discussed at the screening consultation. Patients and their families will be provided with a copy of the information sheets and their signed consent/assent forms.
Potential Risks
The potential risks of the three products (fluticasone propionate, salmeterol and montelukast) used in MASCOT are summarised individually in the tables below. For more detailed information on the potential risks, special warning and precautions for use of these medications please refer to the Summary of Product Characteristics.
Adverse events are listed below by system organ class and frequency. Frequencies are defined as: very common (≥ 1/10), common (≥ 1/100 and < 1/10), uncommon (≥ 1/1000 and < 1/100), rare (≥ 1/10,000 and < 1/1000) and very rare (< 1/10,000) including isolated reports. Very common, common and uncommon events were generally determined from clinical trial data. Rare and very rare events were generally determined from spontaneous data.
Fluticasone propionate
| System Organ Class | Adverse Event | Frequency |
|---|---|---|
| Infections & Infestations | Candidiasis of the mouth and throat | Very Common |
| Immune System Disorders | Hypersensitivity reactions with the following manifestations: | |
| Cutaneous hypersensitivity reactions | Uncommon | |
| Angioedema (mainly facial and oropharyngeal oedema) | Very Rare | |
| Respiratory symptoms (dyspnoea and/or bronchospasm) | Very Rare | |
| Anaphylactic reactions | Very Rare | |
| Endocrine Disorders | Cushing's syndrome, Cushingoid features, adrenal suppression, growth retardation in children and adolescents, decreased bone mineral density, cataract, glaucoma | Very Rare |
| Metabolism & Nutrition Disorders | Hyperglycaemia (see Flixotide SPC Section 4.4 ‘Special Warnings and Precautions for Use’) | Very Rare |
| Gastrointestinal Disorders | Dyspepsia | Very Rare |
| Musculoskeletal & Connective Tissue Disorders | Arthralgia | Very Rare |
| Psychiatric Disorders | Anxiety, sleep disorders, behavioural changes, including hyperactivity and irritability (predominantly in children) | Very Rare |
| Respiratory, Thoracic & Mediastinal Disorders | Hoarseness/dysphonia | Common |
| Paradoxical bronchospasm | Very Rare | |
| Skin & Subcutaneous Tissue Disorders | Contusions | Common |
Salmeterol
| System Organ Class | Adverse Event | Frequency |
|---|---|---|
| Infections and Infestations | Candidiasis of the mouth and throat | Common |
| Pneumonia | *#Common | |
| Bronchitis | *#Common | |
| Immune System Disorders | Hypersensitivity reactions with the following manifestations: | |
| Cutaneous hypersensitivity reactions | Uncommon | |
| Angioedema (mainly facial and oropharyngeal oedema), Respiratory symptoms (dyspnoea and/or bronchospasm), Anaphylactic reactions including anaphylactic shock | Very Rare | |
| Endocrine Disorders | Cushing's syndrome, Cushingoid features, Adrenal suppression, Growth retardation in children and adolescents, Decreased bone mineral density | Very Rare |
| Metabolism and Nutrition Disorders | Hypokalaemia | #Common |
| Hyperglycaemia | Very Rare | |
| Psychiatric Disorders | Anxiety, sleep disorders and behavioural changes, including hyperactivity and irritability (predominantly in children) | Very Rare |
| Nervous System Disorders | Headache | *Very Common |
| Tremor | Common | |
| Cardiac Disorders | Palpitations | Common |
| Tachycardia | Uncommon | |
| Cardiac arrhythmias (including atrial fbrillation, supraventricular tachycardia and extrasystoles) | Very Rare | |
| Respiratory, Thoracic and Mediastinal Disorders | Nasopharyngitis | **#Very Common |
| Throat irritation | Common | |
| Hoarseness/dysphonia | Common | |
| Sinusitis | *#Common | |
| Paradoxical bronchospasm | Very Rare | |
| Skin and Subcutaneous Tissue Disorder | Contusions | *#Common |
| Musculoskeletal and Connective Tissue Disorders | Muscle cramps | Common |
| Traumatic fractures | *#Common | |
| Arthralgia | Very Rare | |
| Myalgia | Very Rare | |
| Eye Disorders | Cataract, glaucoma | Very rare |
* Reported commonly in placebo.
** Reported very commonly in placebo.
# Reported over 3 years in a COPD study.
Montelukast
(Please note no defnition of ‘very rare’ is available for montelukast)
| Body System Class | Adverse Event | Frequency |
|---|---|---|
| Body as a whole | Abdominal pain | Common |
| Asthenia/fatigue, malaise, oedema, | Very rare | |
| Digestive System Disorders | Thirst | Common |
| Diarrhoea, dry mouth, dyspepsia, nausea, vomiting | ||
| Nervous System Disorders | Headache | Common |
| Dizziness, drowsiness, paraesthesia/hypoesthesia, seizure | Very rare | |
| Psychiatric Disorders | Dream abnormalities including nightmares, hallucinations, insomnia, paraesthesia/hypoesthesia, irritability, agitation including aggressive behaviour, restlessness, anxiety, tremor, depression, suicidal thinking and behaviour (suicidality) | Very rare |
| Musculo-Skeletal Disorders | Arthralgia, myalgia including muscle cramps | Very rare |
| Hepato-Biliary Disorders | Elevated levels of serum transaminases (ALT, AST), cholestatic hepatitis | Very rare |
| Cardiovascular Disorders | Palpitations | Very rare |
| Skin & Subcutaneous Tissue Disorders | Angiooedema, urticaria, pruritus, rash, erythema nodosum, bruising | Very rare |
| Immune System Disorders | Hypersensitivity reactions including anaphylaxis, hepatic eosinophilic infiltration | Very rare |
Known Potential Benefits
All of the medications have Marketing Authorisations and have been shown to be efficacious for children with chronic asthma when used appropriately as preventative therapy. The ultimate aims of preventative asthma treatment are the prevention of chronic symptoms, maintenance of near normal lung function and normal activity levels and prevention of recurrent acute episodes in order to maximise quality of life. The potential benefit for participants of taking these medications as part of the trial is that they will improve control of their asthma, reducing symptoms and exacerbations and meeting the goals above.
3. SELECTION OF CENTRES/CLINICIANS
Hubs will be selected upon the basis of:
- an institution with existing links with primary care teams or with the ability to engage and facilitate an effective relationship
- having at least one lead clinician with a specific interest in, and responsibility for, supervising and managing children with asthma, who is enthusiastic about participating in the study
- ensuring that sufficient time, staff and adequate facilities are available for the trial
- providing information to all supporting staff members involved with the trial or with other elements of the patient's management
- identifying that they will be able to recruit the required number of patients
- acknowledging and agreeing to conform to the administrative and ethical requirements and responsibilities of the study, including signing-up to Good Clinical Practice and other regulatory documentation
General Practices will be selected upon the basis of:
- Fully computerised prescribing records
- Willingness to use GPIAG or equivalent asthma template for routine asthma consultations to ensure high quality data when patients reviewed
- Willingness to allow MIQUEST or Apollo extraction tools to enable health resource utilisation (consultations and medications) to be collected electronically
3.1. Centre/Clinician Inclusion Criteria
- Positive Site Specific Assessment (SSA) by LREC
- Local R&D approval
- Receipt of evidence of completion of (a) and (b) by MCRN CTU
- Completion and return of ‘Signature and Delegation Log’ to MCRN CTU
3.2. Centre/Clinician Exclusion Criteria
- Not meeting the inclusion criteria listed above
4. ENDPOINTS
4.1. Primary Endpoint
The primary outcome will be the number of asthma exacerbations requiring treatment with oral corticosteroids over the 48 week study period.
4.2. Secondary Endpoint(s)
- Quality of Life as measured by the Paediatric Asthma Quality of Life Questionnaire (PAQLQ) and the Paediatric Asthma Caregivers Quality of Life Questionnaire (PACQLQ)13
- Time from randomisation to first exacerbation requiring treatment with a short course of oral corticosteroids
- School attendance
- Hospital admissions
- Amount of rescue beta2 agonist therapy prescribed
- Time from randomisation to treatment withdrawal (due to lack of efficacy or side effects)
- Lung function at 48 weeks (as assessed by spirometry)
- Cost effectiveness
- Adverse events
5. STUDY POPULATION
5.1. Inclusion and Exclusion Criteria at T–4 Weeks (Registration)
5.1.1. Inclusion Criteria
- Children with physician diagnosed asthma aged 6 years–14 years, 11months
- Those requiring frequent short-acting beta2 agonist relief therapy ≥ 7 puffs in the past seven days
- Those with symptoms of asthma (i.e. wheeze, shortness of breath but not cough alone) resulting in:
- Nocturnal wakening in the last week because of asthma symptoms and/or
- Asthma has interfered with usual activities in the last week and/or
- Those who have had exacerbations, defined as a short course of oral corticosteroids, an unscheduled GP or A&E Department visit or a hospital admission within the previous 6 months
- Fully informed written (proxy) consent and assent, where appropriate
5.1.2. Exclusion Criteria
- Children receiving long acting beta2-agonists, leukotriene receptor antagonists, regular theophylline therapy or high dose ICS > 1000 micrograms and unlicensed beclometasone dipropionate or equivalent (at the discretion of the investigator)
- Children with other respiratory diseases, cystic fibrosis, cardiac disease or immunological disorders
- Non-English speaking
5.2. Inclusion and Exclusion Criteria at T0 (Randomisation)
5.2.1. Inclusion Criteria
- Children with asthma aged 6 years–14 years
- Those requiring frequent short-acting beta2 agonist relief therapy ≥ 7 puffs in the past seven days
- Those with symptoms of asthma (i.e. wheeze, shortness of breath but not cough alone) resulting in
- Nocturnal wakening in the last week because of asthma symptoms and/or
- Asthma has interfered with usual activities in the last week
- Continuing consent/assent (where appropriate)
5.2.2. Exclusion Criteria
- Children whose asthma is controlled after the 4 week run-in, where control is defined as the absence of any symptoms of asthma (except cough alone) or where the symptoms of asthma have not interfered with usual activities in the last week
- Children receiving long acting beta2-agonists, leukotriene receptor antagonists, regular theophylline therapy or high dose ICS > 1000 micrograms and unlicensed beclometasone dipropionate or equivalent (at the discretion of the investigator)
- Children with other respiratory diseases, cystic fibrosis, cardiac disease or immunological disorders.
- Non-English speaking
5.3. Patient Transfer and Withdrawal
In consenting to the trial, patients are consented to trial treatment, follow-up and data collection. If voluntary withdrawal occurs, the patient and their parent/legal representative should be asked to allow continuation of scheduled evaluations, complete an end-of-study evaluation, and be given appropriate care under medical supervision until the symptoms of any adverse event resolve or the subject's condition becomes stable wherever relevant. Follow-up of these patients will be continued through the research nurse and lead investigator at each secondary care centre and, where this is unsuccessful, through the child's GP (if possible).
5.3.1. Patient Transfers
For patients moving from the area, every effort should be made for the patient to be followed up at another participating trial centre and for this trial centre to take over responsibility for the patient or for follow-up via GP.
A copy of the patient's Case Report Forms (CRFs) should be provided to the new site. The patient and their parent/legal representative will have to sign a new consent form at the new site and, until this occurs, the patient remains the responsibility of the original centre. The CTU should be notified in writing of patient transfers.
5.3.2. Withdrawal from Trial Intervention
Patients may be withdrawn from treatment for any of the following reasons:
- Parent/legal representative (or, where applicable, the patient) withdraws consent for treatment.
- Unacceptable adverse effects.
- Intercurrent illness preventing further treatment.
- Development of serious disease preventing further treatment or any change in the patient's condition that justifies the discontinuation of treatment in the clinician's opinion.
- Lack of efficacy.
The patient should be asked if they are willing to still have data collected as per trial schedule or, failing this, to allow routine follow-up data to be used for trial purposes. Patients who withdraw from trial treatment but are willing to allow further data collection must have a discussion with the investigator as to whether to they will be unblinded at this point or remain blind to their randomised treatment allocation until the end of their 48 week follow-up period. The decision should be based on the patient and their carers' own preferences and whether the investigator feels they need to be aware of the patient's randomised treatment allocation in order to enable appropriate follow on care.
5.3.3. Withdrawal from Trial Completely
Patients are free to withdraw consent at any time without providing a reason. Patients who wish to withdraw consent for the trial will have anonymised data collected up to the point of that withdrawal of consent included in the analyses. The patient will not contribute further data to the study and the MCRN CTU should be informed in writing by the responsible physician and a withdrawal CRF should be completed. MCRN CTU will endeavour to unblind the patient and inform their GP of their randomised treatment allocation within seven days. Data up to the time of withdrawal will be included in the analyses unless the patient explicitly states that this is not their wish.
6. RECRUITMENT, REGISTRATION AND RANDOMISATION
6.1. Recruitment
Patients who are eligible for inclusion into the trial will be identified and recruited through both primary and secondary care. There are several strategies to support the recruitment of participants into MASCOT. Participating sites can adopt either one or a combination of these approaches, depending on their local arrangements and existing pathways for managing patients in the target population.
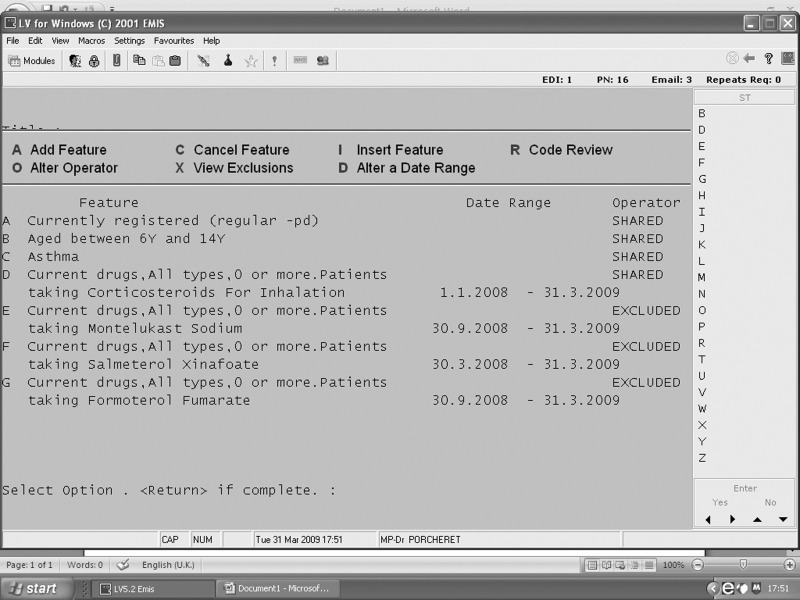
Recruitment Strategy #1
This strategy covers all primary care centres including (but not limited to) general practices and health centres, NHS walk-in centres, GP and nurse-led out of hours services and minor injury centres. Participants will be identified via General Practitioners, community-based specialist paediatric/respiratory nurses and other appropriate clinicians working within primary care. The primary care practitioners will be asked for an estimate on the number of their patients who meet the MASCOT eligibility criteria and, if they do see this patient population, they will be asked if they are willing to take part in helping to identify participants for the trial. This identification will be done by the primary care staff who will search their own patient database/s (either electronically – see Appendix C for search guidance – or manually) to find potentially eligible participants and then write to them (a standard letter will be provided), enclosing a Patient Information Sheet and instructions on how to proceed if they are interested in taking part or finding out more about the study. They will be asked either to send a reply slip back directly to the RN who would then contact them by telephone to ascertain potential eligibility and invite them to a T–4 visit OR to contact the RN by telephone/e-mail for further information. Following this initial mailout, the primary care practitioners may also follow up the letter with a telephone call or one subsequent letter.
Recruitment Strategy #2
In addition to the database searches outlined above, primary care practitioners will also conduct opportunistic recruitment and will ask any patients they identify if they are willing for their contact details to be passed to the research team. If they agree, the RN will then contact them directly to ascertain potential eligibility and invite them to a T–4 visit. Alternatively the practitioner can provide the family with a Patient Information Sheet, which gives the contact details of the research team, with advice to contact them directly if they want to find out more about the trial OR provide them with the approved MASCOT lay person poster (produced as a A5 sized handout) which also gives the contact details of the research team.
Recruitment Strategy #3
Participants will be identified via General Practitioners in primary care. The GPs will be asked for an estimate on the number of their patients who meet the MASCOT eligibility criteria. If they do see this patient population, they will be asked if they are willing to take part in the trial and to take on the role of PI. The practice staff will identify potentially eligible patients and write to them (a standard letter will be provided and printed on practice headed paper), enclosing a Patient Information Sheet and instructions on how to proceed if they are interested in taking part or finding out more about the study. They will be asked to either send a reply slip back directly to the GP who would contact them by telephone to ascertain potential eligibility and then invite them to the T–4 visit OR to contact the GP by telephone/e-mail for further information. Following this initial search, GPs will subsequently conduct opportunistic recruitment and will ask any patients they identify if they are willing for their contact details to be passed to the research team. If they agree, the RN will then contact them directly to ascertain potential eligibility and invite them to a T–4 visit.
Recruitment Strategy #4
Participants will be identified by community pharmacists. During the course of a patient's regular medication review, or whilst providing education on the use of asthma medications, pharmacists may identify patients they believe are potentially eligible for the trial. They will ask any patients who they think may be eligible if they are willing for their contact details to be passed to the research team. If they agree, the RN will then contact them to discuss the trial, ascertain potential eligibility and invite them to a T–4 visit (if appropriate). Alternatively the pharmacist can provide the family with a Patient Information Sheet, which gives the contact details of the research team, with advice to contact them directly if they want to find out more about the trial OR provide them with the approved MASCOT lay person poster (produced as a A5 sized handout) which also gives the contact details of the research team. All pharmacies agreeing to participate in this way will be fully briefed on the trial beforehand. Where it is more appropriate, pharmacists may flag a patient's potential eligibility for the trial to their GP instead of directly to the research team. The GP may then follow any of the methods listed in recruitment strategies #1 & #2 at their own discretion.
Recruitment Strategy #5
Participants will be identified via health professionals with a remit to work within schools (e.g. school nurses, health visitors). They may search their registers and databases to find potentially eligible patients. These patients will then be written to (a standard letter will be provided) enclosing a Patient Information Sheet and instructions on how to proceed if they are interested in taking part or in finding out more about the trial. Following this initial mailout, the school health team may also follow up the letter with a telephone call or one subsequent letter. Alternatively, they may identify patients who are potentially eligible during the course of their normal role. After gaining permission from the patient's parent/legal guardian, the health professional will pass their contact details to the research team. The RN will then contact the family directly to discuss the trial, ascertain potential eligibility and invite them to a T–4 visit (if appropriate).
Recruitment Strategy #6
Participants will be identified via secondary care (A&E admissions, routine OPD appointments, specialist nurse-led clinic appointments). Secondary care professionals will be approached by the MASCOT RN/LRN nurses and the PI and informed about the trial. If a patient presents who may be eligible for the trial, the medical staff treating them initially can follow one of two routes: 1) contact the local PI/RN and ask them to come and speak to the patient there and then about the trial, inviting them to attend a T–4 visit if they are potentially eligible and interested in participating OR 2) give the patient a PISC and ask for their permission to pass their contact details on to the RN who will call the patient later to discuss the trial and invite them for a T–4 visit if they are eligible.
Recruitment Strategy #7
Participants will be identified via secondary care by their usual NHS clinical team who will search the Trust databases to find potentially eligible participants. These patients will then be written to (a standard letter will be provided and printed on Trust headed paper), enclosing a PISC and instructions on how to proceed if they are interested in taking part or finding out more about the trial. They could either be asked to send a reply slip back directly to the RN who would contact them by telephone to ascertain the patient's eligibility and then invite them to the T–4 visit OR to contact the RN by telephone/e-mail for further information. Following this initial mailout, the secondary care team may also follow up the letter with a telephone call or one subsequent letter.
Recruitment Strategy #8
The trial may also be promoted via appropriate websites, magazines and newspapers to be accessed by both health professionals and the general public. Approval will be sought from the REC for any specific features or advertisements designed to promote the trial directly to the public, prior to submitting them for publication.
6.2. Screening (Registration)
A log of potential patients will be kept (the ‘Screening and Enrolment Log’), including individuals who decide not to participate in the study at the T–4 visit and ineligible referrals from primary care practitioners and secondary care clinicians. Screening will be performed of a patient's possible eligibility for the study and must be documented on the screening CRF at the T–4 visit.
Screening at T–4 (See Section 8 for T–4 assessments)
- Confirm aged 6–14 years, 11 months
- Explanation of the two different phases of the trial and understanding that eligibility for trial treatment will be reassessed at T0 visit
- Fully informed written proxy consent (and assent, where appropriate) to participate in the trial
- Assessments to determine eligibility (inc. review of medical history, symptoms, concomitant medications)
- Fluticasone propionate dispensed (open label)
- Submission of T–4 CRF to MCRN CTU within seven days of registration
- Forward copy of consent/assent forms to MCRN CTU within seven days of registration
6.3. Enrolment/Baseline (Randomisation)
Screening at T0
- A check of compliance with hand held asthma record completion
- Review of symptoms and exacerbations
- A check of concomitant medications prescribed/administered since T–4 visit
- Complete physical examination performed
- Verification that the eligibility criteria for randomisation is fulfilled
- See Section 8 for T0 assessments
Randomisation Process
- Continuing consent and assent (where appropriate) obtained verbally
- Completion of randomisation CRF and trial prescription
- Attend local pharmacy (see Table 1 for pharmacy contact details)
- Participant's treatment allocation ascertained by pharmacy using the site randomisation list
- Issue of treatment pack by pharmacy department (ensuring the patient and researcher are blinded to the allocation)
- Submission of T0 CRF to MCRN CTU within seven days of randomisation
Table 1
Pharmacy Contact Details
7. TRIAL TREATMENT/S
7.1. Introduction
This study is designed as a prospective, controlled, double-blind, multicentre, randomised clinical trial comparing whether control of asthma symptoms can be improved by adding in a long-acting beta2 agonist (salmeterol) or a leukotriene receptor antagonist (montelukast) in 6–14 year olds with asthma uncontrolled on low-dose inhaled corticosteroids (ICS).
During the four week run-in period all patients will be commenced on fluticasone propionate inhalers at 200 micrograms per day (100 micrograms twice daily). Children who remain symptomatic at the end of the run-in period will be randomised into one of three double-blinded treatment regimen:
- Inhaled fluticasone propionate 100 micrograms twice daily plus placebo tablet once daily
- Inhaled fluticasone propionate 100 micrograms and salmeterol 50 micrograms twice daily (combination inhaler) plus placebo tablet once daily
- Inhaled fluticasone propionate 100 micrograms twice daily plus montelukast 5 mg tablet once daily.
7.2. Formulation, Packaging, Labelling, Storage and Stability
A: Fluticasone propionate
Description and composition of the drug product
Product name – fluticasone propionate (brand name, Flixotide™).
Flixotide 100 micrograms Accuhaler is a multi-dose dry powder inhalation device delivering 100 micrograms of fluticasone propionate per inhalation. Participants will receive 100 micrograms twice daily, taken as one inhalation twice daily.
Flixotide has been manufactured and supplied by GlaxoSmithKline plc (GSK).
Type of container and closure system
The Flixotide Accuhaler is a moulded plastic device containing a foil strip with regularly placed blisters each containing a mixture of fluticasone propionate (100 micrograms) and lactose monohydrate. The blister strip consists of a formed foil base with a peelable foil laminate lid. Each inhaler contains 60 pre-dispensed doses of Flixotide. The inhaler device is packed in an individual cardboard container, which will be labelled for trial treatment (labels will include study acronym, EudraCT reference number, randomisation number, visit number, site number, instructions for use and storage, batch number and expiry date).
Stability and shelf life
The product should be stored at temperatures less than 30°C and should not be refrigerated or frozen. The product has a shelf life of 18 months.
B: Salmetrol + Fluticasone propionate
Description and composition of the drug product
Product name – salmeterol (brand name, Seretide™).
Seretide 50/100 micrograms Accuhaler is a multi-dose dry powder inhaler delivering 50 micrograms of salmeterol (as salmeterol xinafoate) and 100 micrograms of fluticasone propionate. Participants will receive 50 micrograms and 100 micrograms (respectively) twice daily, taken as one inhalation twice daily in a combined inhaler.
Seretide has been manufactured and supplied by GlaxoSmithKline plc.
Type of container and closure system
The Seretide Accuhaler is a moulded plastic device containing a foil strip with regularly placed blisters each containing a mixture of fluticasone propionate (100 micrograms), salmeterol (50 micrograms) and lactose monohydrate. The blister strip consists of a formed PVC base with a peelable foil laminate lid. Each inhaler contains 60 pre-dispensed doses of Seretide. The inhaler device is packed in an individual cardboard container, which will be labelled for trial treatment (labels will include study acronym, EudraCT reference number, randomisation number, visit number, site number, instructions for use and storage, batch number and expiry date).
Stability and shelf life
The product should be stored at temperatures less than 30°C and should not be refrigerated or frozen. The product has a shelf life of 18 months.
C: Montelukast
Description and composition of the drug product
Product name – montelukast (brand name, Singulair®).
Singulair Paediatric 5 mg Chewable Tablets contain montelukast sodium, which is equivalent to 5 mg montelukast. Participants will receive 5 mg once daily, taken as a single chewable tablet. The tablet is round, biconvex and 9.5 mm in diameter. Singulair also contains mannitol, microcrystalline cellulose, hydroxypropylcellulose, red ferric oxide (E172), croscarmellose, cherry flavour, aspartame and magnesium stearate.
Singulair has been manufactured and supplied by Merck Sharp and Dohme Ltd (MSD).
Type of container and closure system
The tablets will be packaged in monthly blister packs of 35 days supply, with an aluminium foil top. Three blister packs will be packaged in an outer cardboard carton and labelled for trial treatment (labels will include study acronym, EudraCT reference number, randomisation number, visit number, site number, instructions for use and storage, batch number and expiry date).
Stability and shelf life
The product should be stored at ambient temperature in the original packaging. The product has a shelf life of 24 months.
Placebo
Description and composition of the drug product
Product name – montelukast (brand name, Singulair®) matching placebo
The drug product (Singulair Paediatric 5 mg Chewable Tablets) placebo tablet is round, biconvex and 9.5 mm in diameter to match the active drug. The placebo contains mannitol, microcrystalline cellulose, hydroxypropylcellulose, red ferric oxide (E172), croscarmellose, cherry flavour, aspartame and magnesium stearate.
The drug product (Singulair) placebo has been manufactured and supplied by Merck Sharp and Dohme Ltd (MSD).
Type of container and closure system
The tablets will be packaged in monthly blister packs of 35 days supply, with an aluminium foil top. Three blister packs will be packaged in an outer cardboard carton and labelled for trial treatment (labels will include study acronym, EudraCT reference number, randomisation number, visit number, site number, instructions for use and storage, batch number and expiry date).
Stability and shelf life
The product should be stored at ambient temperature in the original packaging. The product has a shelf life of five years.
7.3. Preparation, Dosage and Administration of Study Treatment/s
Dispensing
For each randomised patient, treatment will continue for a maximum period of 48 weeks. Patients will be randomised by pharmacy using a randomisation list provided to the site by the coordinating centre. Pharmacy will ensure that the participant and the researcher are blinded to the treatment allocation. After randomisation patients will be dispensed their first treatment pack. Each treatment pack contains three months of trial medication, consisting of:
- Three inhalers (each inhaler containing 60 inhalations or 30 days treatment)
- Three blister packs (each blister pack containing 35 days treatment)
All treatments will be dispensed at the standard dose throughout the trial, unless interruption or discontinuation is warranted and agreed by the PI (see Section 7.4). The dose regimens are:
- inhaled fluticasone propionate 100 micrograms twice daily + placebo tablet once daily
- inhaled fluticasone propionate 100 micrograms and salmeterol 50 micrograms twice daily (combination inhaler) + placebo tablet once daily
- inhaled fluticasone propionate 100 micrograms twice daily + montelukast 5 mg tablet once daily.
When pharmacy dispense the trial treatments they will add their own dispensing label, which will include information such as the name and address of the hospital, the patient's name or initials, date of dispensing and instructions for use. They will also complete the information specified on the medication trial labels (i.e. patient trial number, visit number etc.).
The medications will be dispensed upon production of a valid, signed trial prescription to either the RN or directly to the patient and their carer/s as detailed below*:
T–4 study visit
One inhaler of fluticasone propionate (open label) will be dispensed for a registered participant at T–4 on receipt of a valid trial prescription. If the T–4 visit is conducted at an outreach or community site (e.g. a GP practice) and the participant is registered during the visit the RN will arrange for them to receive the study medication once it has been dispensed from pharmacy. The dispensed medication will be collected from pharmacy and securely transported by a member of the research team, ensuring temperature monitoring is conducted until it is given to the patient. The RN will arrange with the patient and their carer/s to collect the medication from the outreach site, ensuring that it is collected by the family within an agreed timeframe (no longer than three days).
T0 study visit
The participant will be randomised to a treatment arm by pharmacy. Ensuring the RN and participant remain blinded as to the treatment allocation, one three month treatment pack containing three inhalers and three monthly blister cards will be dispensed on receipt of a valid trial prescription. If the T0 visit is conducted at an outreach or community site (e.g. a GP practice) and the participant is randomised during the visit the RN will arrange for them to receive the study medication once it has been dispensed from pharmacy. The dispensed medication will be collected from pharmacy and securely transported by a member of the research team, ensuring temperature monitoring is conducted until it is given to the patient. The RN will arrange with the patient and their carer/s to collect the medication from the outreach site, ensuring that it is collected by the family before the patient runs out of their current prescription.
T+8 study visit
The participant's randomised treatment allocation will be ascertained by pharmacy. Ensuring the RN and participant remain blinded as to the treatment allocation, one three month treatment pack each containing three inhalers and three monthly blister cards will be dispensed from pharmacy on receipt of a valid trial prescription.
Where the study visit is conducted at the lead local site and the patient has access to the trial's pharmacy department, the patient and their carer/s can collect the medication at the end of the study visit as per usual clinical practice. Where the patient is seen at an outreach or community site (e.g. a GP practice) for T+8, the RN will collect the appropriate medications from the pharmacy department prior to the visit. The RN will securely transport them to the visit site, ensuring temperature monitoring is conducted, where they will be given to the patient. If the patient is not eligible to continue in the trial or wishes to withdraw from trial treatment at that point, the dispensed medications will be returned to pharmacy for destruction.
T+24 study visit
The participant's randomised treatment allocation will be ascertained by pharmacy. Ensuring the RN and participant remain blinded as to the treatment allocation, two three month treatment packs each containing three inhalers and three monthly blister cards will be dispensed from pharmacy on receipt of a valid trial prescription.
Where the study visit is conducted at the lead local site and the patient has access to the trial's pharmacy department, the patient and their carer/s can collect the prescription at the end of the study visit as per usual clinical practice. Where the patient is seen at an outreach or community site (e.g. a GP practice) for T+24, the RN will collect the appropriate medications from the pharmacy department prior to the visit. The RN will securely transport them to the visit site, ensuring temperature monitoring is conducted, where they will be given to the patient. If the patient is not eligible to continue in the trial or wishes to withdraw from trial treatment at that point, the dispensed medications will be returned to pharmacy for destruction.
*In certain circumstances, the RN may deliver the study medications to the family home. A RN may only deliver medications to a patient's home if this procedure is authorised for their site by the coordinating centre and an appropriate SOP is in place. In addition, due to geographical constraints, Norfolk & Norwich University Hospital pharmacy department will follow a separate dispensing procedure for participants who cannot be seen at the lead local site (outlined in Appendix B).
Lost or Damaged Medications
In the event that a patient loses or damages the inhaler or tablet pack they are currently using, they will move straight onto the next month's medication from the pack they were dispensed with at their last visit. The patient should contact the RN who will bring forward the date of the next visit to ensure that the patient can be dispensed their next prescription (if applicable) in sufficient time to ensure there is no break in medication. However, if the patient has no more dispensed medication, they should contact the RN immediately to discuss how to manage their treatment. If no arrangements can be put in place for the patient to collect their next medication pack from the pharmacy within an acceptable period of time, the PI will withdraw the patient from the trial at that point. The patient will return to the care of their usual medical practitioner and will be followed up as per the protocol by the research team (see Section 5.3.2).
Administration
The patient and their carer/s will be instructed in the correct use of the medications dispensed. Patients will be instructed in the proper use and care of their inhaler by the RN at T–4 and will have their technique assessed. Further guidance will be provided throughout the remainder of the trial where necessary.
The trial treatments have two different routes of administration:
- inhalation (fluticasone/salmeterol). One inhalation to be taken twice daily at regular intervals (e.g. once in the morning and once in the evening).
- oral (montelukast/placebo). One tablet is to be administered daily, to be taken in the evening. If taken in conjunction with food, montelukast should be taken one hour before or two hours after eating.
7.4. Dose Modifications
The decision to interrupt or discontinue trial therapy is at the discretion of the treating physician. Doses may be interrupted or discontinued at any point during the trial period for reasons such as unacceptable adverse effects, intercurrent illness, development of serious disease or any change in the patient's condition that the physician believes warrants a change in medication (see Section 5.3.2). Any changes must be documented in the CRF along with the justification for those changes.
7.5. Accountability Procedures for Study Treatment/s
Clinical trial supplies will only be delivered to an investigator site once the site has been initiated. This can only be completed once full ethical and regulatory approvals have been granted. This must be confirmed by the Trial Coordinator acting on behalf of the study sponsor. The size of the shipments to each site will be pre-determined based on the patient recruitment target for that individual site. The first shipment will be approximately a quarter of the total trial supplies for the site and there will be a maximum of three subsequent shipments over the two year trial period. Recruitment will be monitored centrally and drug shipment dates will be tailored accordingly to ensure that pharmacies always hold adequate supplies of trial treatment. Pharmacies will document all shipment receipts and will provide copies of this documentation to the Trial Coordinator.
Following registration into the trial of an individual participant, the following accountability procedures for clinical trial supplies at pharmacy will apply:
At T–4 the RN/PI will collect an inhaler of fluticasone propionate (open label) from pharmacy and record the receipt of this by the patient on the T–4 CRF. Pharmacy will put their dispensing label (including information such as patient name or initials, pharmacy address, telephone number and date of dispensing) on to the inhaler carton and will complete, sign and date the accountability log. A second member of the pharmacy team will counter-sign the log to document the dispensing.
At T0 the patient will be randomised and a blinded treatment pack will be dispensed by pharmacy according to their treatment allocation. Pharmacy will ensure that the participant and the researcher remain blinded to the treatment allocation. Pharmacy will put their dispensing label (including information such as patient name or initials, pharmacy address, telephone number and date of dispensing) on to the pack and will complete, sign and date the accountability log. A second member of the pharmacy team will counter-sign and date the log to document the dispensing. The RN will record the participant's randomisation number in the CRF. Upon allocation, the patient's trial number will also be recorded in their individual hand held asthma record.
At each subsequent dispensing, the patient's randomised treatment allocation will be ascertained by pharmacy and a treatment pack/s dispensed on production of a valid trial prescription. Pharmacy will ensure that the participant and the researcher remain blinded to the treatment allocation. The accountability log will be updated and signed and dated by two members of the pharmacy team. Where the prescription is dispensed to the RN for transport to another site, the RN will transport the medications securely ensuring that the temperature of the products is controlled and recorded. At all study visits from T0–T+48, unused medications (including omitted doses from the previous prescription's regimen) will be collected by the RN and returned to pharmacy for destruction.
7.6. Assessment of Compliance with Study Treatment/s
Participants will be asked to retain all used and unused trial medications and packaging and bring them to each study visit from T0–T+48. The research doctor/nurse will collect the returned supplies in order to assess compliance with the trial treatment regimen. The inhalers supplied to the participants contain dose counters which show the number of doses remaining. Once the compliance checks have been completed and recorded, the RN will deliver all returned medications to pharmacy for destruction via their local procedures.
T0 study visit
All registered participants will be asked to bring the fluticasone inhaler they were issued at T–4 to the T0 study visit. The research doctor/nurse will ask the participant and their carer/s about compliance with the treatment regime and whether any doses have been missed. At the end of the study visit, after the patient has left, the researcher will use the dose counter on the inhaler to verify the information provided by the family. The number of inhalations reported by both the participant and the dose counter will be recorded on the CRF along with the reason given for any doses missed (if applicable).
T+8 study visit
The research nurse will collect all used medications and packaging from the participant. The participant will have been issued with 12 weeks of treatment at T0 so will retain one inhaler and one monthly blister pack for use over the next four weeks.
The research nurse will ask the participant and their carer/s about compliance with the treatment regime since their last visit and whether any inhalations or tablets have been missed. At the end of the study visit, after the patient has left, the researcher will use the dose counter on the inhaler and conduct a full pill count to verify the information provided by the family. The number of doses reported by the participant and from the medication counts will be recorded on the CRF along with the reason given for any doses missed (if applicable).
T+24 study visit
The research nurse will collect all used and unused medications and packaging from the participant. They will ask the participant and their carer/s about compliance with the treatment regime since their last visit and whether any inhalations or tablets have been missed. At the end of the study visit, after the patient has left, the researcher will use the dose counter on the inhaler and conduct a full pill count to verify the information provided by the family. The number of doses reported by the participant and from the medication counts will be recorded on the CRF along with the reason given for any doses missed (if applicable).
T+36 telephone call
The research nurse will ask the participant and/or their carer/s about compliance with the treatment regime since their last visit and whether any inhalations or tablets have been missed. The number of doses reported by the participant will be recorded on the CRF along with the reason given for any doses missed (if applicable). The RN will remind the participant to bring all used and unused medications and packaging to their next study visit.
T+48 study visit
The research nurse will collect all used and unused medications and packaging from the participant. They will ask the participant and their carer/s about compliance with the treatment regime since their last visit and whether any inhalations or tablets have been missed. At the end of the study visit, after the patient has left, the researcher will use the dose counter on the inhaler and conduct a full pill count to verify the information provided by the family. The number of doses reported by the participant and from the medication counts will be recorded on the CRF along with the reason given for any doses missed (if applicable).
Early withdrawal
If a patient wishes to prematurely withdraw from trial treatment, the research nurse will collect all used and unused medications and packaging from the participant. They will ask the participant and their carer/s about compliance with the treatment regime since their last visit and whether any inhalations or tablets have been missed. The researcher will use the dose counter on the inhaler and conduct a full pill count to verify the information provided by the family. The number of doses reported by the participant and from the medication counts will be recorded on the CRF along with the reason given for any doses missed (if applicable).
7.7. Concomitant Medications/Treatments
7.7.1. Medications Permitted
Details of concomitant medications will be collected at the T–4 visit and recorded on the CRF. They will be reviewed at all subsequent study visits (clinic visits, telephone call) until T+48. The trial treatments have very few adverse interactions with other medicinal products so concomitant medications, with the exception of those listed in Section 7.7.2, are permissible at the discretion of the investigator.
7.7.2. Medications Not Permitted/Precautions Required
The following are not permitted for the duration of the trial period:
- Inhaled corticosteroids (other than the trial treatment)
- Long-acting beta2 agonists (other than trial treatment)
- Leukotriene receptor antagonists (other than trial treatment)
- All beta-blockers
- Theophylline
Caution should be exercised when prescribing CYP3A inhibitors as they may affect the efficacy of montelukast (see Singulair SPC Section 4.5 ‘Interactions with other medicinal products and other forms of interaction’). CYP3A inhibitors (e.g. ketaconazole, itraconazole) are not permitted for regular or frequent use during the trial treatment period. All prescribed CYP3A inhibitors should be documented on the Concomitant Medications CRF.
7.7.3. Data on Concomitant Medication
The dose and name of all concomitant medications should be documented on the CRF at T–4. This will be reassessed at each trial visit by the PI/RN. Any new medications introduced or any changes to current medications should be documented on the CRF.
7.8. Unblinding
Unblinding should be considered when knowledge of the treatment assignment is deemed essential for the child's care by their physician or a regulatory body. In general, unblinding of participants before they have completed their individual 48 week follow-up period should be considered when the participant has prematurely withdrawn from trial treatment or when there are compelling medical or safety reasons to do so.
N.B. If simply ceasing study treatment is a viable option for the patient's care, it should not be necessary for unblinding to occur.
7.8.1. Procedure
Emergency Unblinding
- The decision to unblind a single case should be made when knowledge of an individual's allocated treatment is required to:
- enable treatment of severe adverse event/s, or
- enable administration of another therapy that is contraindicated by the trial treatment.
- Where possible, requests for emergency or unplanned unblinding of individuals should be made via the Trial Coordinator at MCRN CTU. Agreement of the chief investigator (Professor Warren Lenney) will then be sought. Professor David Price will be consulted in the chief investigator's absence.
- Contact the central pharmacy at University Hospital of North Staffordshire NHS Trust, where unblinding codes are held:
Monday to Friday 0900 to 1700 hours Telephone: 01782 552912 Saturday 0900 to 1300 hours Ask for Senior/Clinical Trials Pharmacist, quoting MASCOT unblinding service Sunday 1000 to 1400 hours All other times Telephone: 01782 715444 (UHNS Switchboard) 07623623377 (on-call pager) Please use the switchboard number in the first instance Ask for the on-call pharmacist, quoting MASCOT unblinding service - The central pharmacy will release the allocation details of an individual patient only, documenting:
- Date information needed
- Detailed reason for unblinding
- Identity of recipient of the unblinding information
- Ensure all necessary CRFs to time of unblinding are completed and submitted to MCRN CTU (if possible, completed before unblinding is performed)
- All instances of unblinding should be recorded and reported in writing to the MCRN CTU by the local investigator, including the identity of all recipients of the unblinding information.
- Allocation should not routinely be revealed to MCRN CTU personnel.
Accidental Unblinding
All instances of inadvertent unblinding should be recorded and reported in writing to the MCRN CTU by the local investigator. Reports to include:
- Date of unblinding
- Detailed explanation of circumstances
- Recipients of the unblinding information
- Action to prevent further occurrence
Allocation should not be routinely revealed to MCRN CTU personnel.
Routine Unblinding at the End of Follow-up
At the end of their individual 48 week follow-up period, participants will be instructed to contact their GP who will be informed which treatment allocation their patient had been randomised to. Upon receipt of a T+48 visit CRF, MCRN CTU will unblind that individual and write to the patient's GP to inform them which treatment they had been prescribed. MCRN CTU will endeavour to inform the patient's GP within seven days of the T+48 visit occurring. Where the patient was managed within secondary or tertiary care for their asthma treatment prior to entering the study, the relevant clinician or specialist nurse will be informed by the MCRN CTU that the patient has completed their involvement in the trial and advised to contact the GP if they need to know what randomised treatment the patient had been taking. The participant and their guardian will be made aware of this procedure in the patient information sheet and at their final study visit. In the interim period between the end of trial treatment at T+48 and the patient's GP being informed of their treatment allocation, patients will be treated as per local standard practice.
At Trial Closure
The end of the trial will be considered as the date of the final database lock. However the trial may be closed prematurely by the Trial Steering Committee, on the recommendation of the Independent Data and Safety Monitoring Committee.
Upon trial closure the central pharmacy department at University Hospital of North Staffordshire NHS Trust will return unblinding codes to the MCRN CTU. MCRN CTU will notify local investigators in writing of unblinding information for patients under their care. A copy of this notification should be placed in the medical records and a copy retained in the site file.
7.9. Co-enrolment Guidelines
To avoid potentially confounding issues, ideally patients should not be recruited into other trials. Individuals who have participated in a trial testing a medicinal product within one month preceding screening will be ineligible for the MASCOT study. Where recruitment into another trial is considered to be appropriate and without having any detrimental effect on the MASCOT trial this must first be discussed with the coordinating centre (MCRN CTU) who will contact the chief investigator (Professor Warren Lenney).
8. ASSESSMENTS AND PROCEDURES
8.1. Schedule of Study Visits
See schedule of study procedures, Table 2. Wherever possible, all study visits after randomisation (T0) should be conducted no earlier than one week before the appropriate date (e.g. no earlier than seven weeks after randomisation for T+8). When planning a visit which is later than the appropriate date, the research team should consider the participant's remaining trial medications and ensure they do not run out prior to the visit.
Table 2
Schedule of Study Procedures
Due to geographical constraints, some participating centres sites may conduct certain study visits at ‘satellite’ sites (e.g. GP practices) in their region. Patients will be seen for study visits at these locations by the research team if they are unable to travel to their lead local centre. Patients will remain under the care of the local principal investigator for their region, who will be based at the lead site. Trial medications will be dispensed from the pharmacy department at the lead centre. For all satellite sites research governance approval will first be sought from the appropriate Trust and the main REC will also be notified.
Four Week Run-in Period (Study visit)
Patients will be screened in GP surgeries in primary care and in paediatric clinics in secondary care. Following full informed written (proxy) consent, those eligible will be registered into the study, have their inhaler technique checked and be provided with information about asthma and its management. All research centres taking part will be centrally trained and instructed in the approach to the patients and their families in an attempt to obtain uniformity. They will all be dispensed the same low-dose inhaled corticosteroid, fluticasone propionate, in the dose of 100 micrograms twice daily. They will participate in an open four week ‘run-in’ period and will complete a hand-held patient record that will provide information to aid assessment of ongoing control (see 8.2.1).
The same criteria will be used in all centres to determine whether the patient is effectively controlled or not. Poorly controlled, as defined in sections 5.1 and 5.2, will be those requiring frequent short-acting beta2 agonist relief therapy ≥ 7 puffs per week and with asthma symptoms affecting sleeping and/or usual activities in the last week and/or who have had exacerbations (defined as a short course of oral corticosteroids, an unscheduled GP or A&E Department visit or a hospital admission within the previous six months).
The purpose of this run-in period is to ensure that we are only recruiting those patients for whom control of their asthma presents a problem, rather than those for whom inhaler technique and management advice will be sufficient to provide symptomatic relief. Most run-ins lose approximately 25% patients but we anticipate that improved education and attention to compliance in this study may well make up to 50% ineligible for entry into the randomised part of the study. All patients registered will have GP data follow-up one year after registration, regardless of continuation into the main trial, which is detailed in the patient information sheet and consent form (PISC). We will collect data on things such as symptoms, exacerbations, hospital appointments, medication changes and use.
At the T–4 review, families will also be issued with a copy of the PISC requesting the collection of a DNA sample for storage and investigation at a later date (section 8.4.1). They will be invited to consent and provide a DNA sample (saliva) at their T0 clinic visit. Consent to provide a DNA sample is documented separately to that of consent for the main trial.
The next study visit (T0) will be organised with the participant and their carer/s to be in no less than 24 days time and no longer than 30 days time from T–4.
Time 0: Entry into full study (Study visit)
Following the run-in period patients will be re-assessed for study entry based upon inclusion and exclusion criteria (section 5.2). Those patients achieving the threshold criteria for T0 will be entered into the randomised part of the study.
Symptoms, exacerbations and beta2 agonist use will be ascertained by reviewing the hand held record with the patient and their carer/s. Baseline Paediatric Asthma Quality of Life Questionnaire (interviewer administered if child is 10 years of age or younger, patient administered if aged 11 years or more) and Paediatric Asthma Caregivers Quality of Life Questionnaire (carer administered) assessments will be conducted and a complete physical examination will be performed, including height and weight measurements. Spirometry will be carried out to measure the patient's FEV1, FVC and FEV1/FVC ratio (best of three before and after bronchodilator).
Each patient is then randomised by pharmacy using a randomisation list supplied centrally and dispensed their first three month treatment pack according to their treatment allocation. Treatment is to continue for eight weeks and the allocated treatment will be double-blinded, achieved by using identical inhalers and placebo tablets, with patients allocated to receive either:
- Inhaled fluticasone propionate 100 micrograms twice daily plus placebo tablet once daily
- Inhaled fluticasone propionate 100 micrograms and salmeterol 50 micrograms twice daily (combination inhaler) plus placebo tablet once daily
- Inhaled fluticasone propionate 100 micrograms twice daily plus montelukast 5 mg tablet once daily.
Following a separate consent process, a DNA specimen will be obtained (see Section 8.4.1). Individuals declining to provide DNA will not be precluded from entry into main trial.
Randomisation + 8 weeks (Study visit)
Symptoms, exacerbations and beta2 agonist use will be ascertained by reviewing the hand held record with the patient and their carer/s. The Health Economics questionnaire completed throughout the time period since the last clinic visit will be checked for completeness and removed. A new, blank questionnaire will be inserted into the hand held record to be used until the next appointment. Repeat Quality of Life Assessments will be administered (interviewer [if child is 10 years of age or younger], patient [if aged 11 years or more] and carer administered) and a symptom-directed physical examination will be performed as appropriate. Adverse events will be reported and recorded.
Those who have achieved control of their asthma symptoms will continue on the same treatment for the next 16 weeks. For those whose symptoms have not improved but are no worse, the PI/RN will discuss their willingness to continue with randomised treatment.
Those who are clinically worse may be withdrawn from randomised treatment and given alternative treatment according to clinician's advice as in routine practice. The decision to withdraw the patient from trial treatment is based on the patient's current clinical presentation and the review of information on symptoms/exacerbations etc collected in the hand held record over the preceding weeks. The decision is made at the discretion of the investigator using their informed clinical opinion. The reason for discontinuation of trial treatment must be documented on the CRF. Follow-up should be continued until the end of the trial as per the study visit schedule.
In certain circumstances, the PI/RN may conduct the T+8 study visit at the family home where it is appropriate and necessary to do so. The PI/RN must only conduct a study visit in the family home if this has been authorised for their site by the coordinating centre and appropriate lone working procedures are in place.
Randomisation + 24 weeks (Study visit)
Symptoms, exacerbations and beta2 agonist use will be ascertained by reviewing the hand held record with the patient and their carer/s. The Health Economics questionnaire completed throughout the time period since the last clinic visit will be checked for completeness and removed. Two new, blank questionnaires will be inserted into the hand held record to be used until the next study visit. Repeat Quality of Life Assessments will be administered (interviewer [if child is 10 years of age or younger], patient [if aged 11 years or more] and carer administered) and a symptom-directed physical examination will be performed as appropriate. Adverse events will be reported and recorded.
Those who have achieved control of their asthma symptoms will continue on the treatment. For those whose symptoms have not improved but are no worse, the PI/RN will discuss their willingness to continue with randomised treatment.
Those who are clinically worse may be withdrawn from randomised treatment and given alternative treatment according to clinician's advice as in routine practice. The decision to withdraw the patient from trial treatment is based on the patient's current clinical presentation and the review of information on symptoms/exacerbations etc collected in the hand held record over the preceding weeks. The decision is made at the discretion of the investigator using their informed clinical opinion. The reason for discontinuation of trial treatment must be documented on the CRF. Follow-up should be continued until the end of the trial as per the study visit schedule.
In certain circumstances, the PI/RN may conduct the T+24 study visit at the family home where it is appropriate and necessary to do so. The PI/RN must only conduct a study visit in the family home if this has been authorised for their site by the coordinating centre and appropriate lone working procedures are in place.
Randomisation + 36 weeks (Telephone call)
Symptoms, exacerbations and beta2 agonist use will be ascertained from the patient and/or their carer/s. The RN will check that they are continuing to complete the hand held record and that they have completed the inserted Health Economics questionnaire for the time period since their last clinic visit. They will be asked to remove the completed questionnaire and place it to the back of the record to avoid any confusion. The RN will remind them to begin a new Health Economics questionnaire to be used until their next appointment.
Adverse events will be reported and recorded. Those who have achieved control of their asthma symptoms will continue on the trial treatment. For those whose symptoms have not improved but are no worse, the RN will discuss their willingness to continue with randomised treatment. Those whose asthma symptoms appear to be worse will either be offered an unscheduled study appointment with a member of the research team (if possible) or advised to visit their General Practitioner to seek further medical advice. If the practitioner believes they are clinically worse the patient may be withdrawn from randomised treatment and given alternative treatment according to clinician's advice as in routine practice. The reason for discontinuation of trial treatment must be documented on the CRF. Follow-up should be continued until the end of the trial as per the study visit schedule.
Randomisation + 48 weeks (Clinic visit)
Symptoms, exacerbations and beta2 agonist use will be ascertained by reviewing the hand held record with the patient and their carer/s. The two Health Economics questionnaires completed throughout the time period since the last clinic visit will be checked for completeness and removed. Final Quality of Life assessments will be administered (interviewer [if child is 10 years of age or younger], patient [if aged 11 years or more] and carer administered) and a basic physical examination will be performed, including height and weight measurements. Further examination will be symptom led. Spirometry will be carried out to measure the patient's FEV1, FVC and FEV1/FVC ratio (best of three before and after bronchodilator). Adverse events will be reported and recorded.
Patients will be asked to provide current details for their General Practitioner (GP). They will be informed that their GP will be provided with details of which treatment they have been taking within seven days. If the patient was under the care of a different clinician for their asthma management prior to entering the study, that clinician will also be provided with details of the treatment wherever possible. The PI/RN will discuss future management with patients and their carer/s.
8.2. Procedures for assessing Efficacy
Efficacy of trial treatments will be assessed throughout the period of the study using both objective and subjective measures.
8.2.1. Hand Held Records
Hand held records will be used throughout by participants, from T–4 through to T0, and continuing until study completion (T+48) for those patients who proceed with randomisation at T0. The records are A6 sized folders, which are divided into sections relating to different aspects of a child's asthma and their management of it. They were developed by The Guy Hilton Asthma Trust and have been modified for the purposes of the MASCOT trial to collect data relevant to the trial outcomes.
There are sections in the records to capture information on daily symptoms, exacerbations, use of beta2 agonist relief therapy, management/treatment schedule and emergency contact numbers. The records can be completed by patients and/or their carer/s on a continuous basis so the information recorded will be current and accurate.
The records will be brought along to every study visit and reviewed by the PI/RN in conjunction with the patient and their carer/s. The information collected in the records will be used to assess how well participants' asthma is being controlled on the trial treatments and will be important in determining whether they should progress to the next stage of the trial. The information collected in the hand held records will be regarded as source data so at each clinic visit the completed pages will be removed from the record.
The original sheets will be sent to CTU, a copy retained in the Site File and the family will be provided with a copy for their own records (if requested).
The review of hand held records at each study visit, detailing patients' symptoms and exacerbations, will indicate how effectively their asthma is being controlled and so can be used to assess efficacy of the trial treatments.
8.2.2. Spirometry
Spirometry will be carried out at baseline (T0) and study completion (T+48) and will provide an objective measure of efficacy. Spirometry will be undertaken pre and post bronchodilator and will only be accepted if meeting American Thoracic Society (ATS)/European Respiratory Society (ERS) standards for acceptability and reproducibility. The following values will be recorded in the CRF:
- Date and time of spirometry
- Whether readings meet ATS standards for acceptability and reproducibility
- Whether bronchodilators withheld for appropriate length of time – short-acting 4 hours and long-acting 24 hours
- FEV1 pre and post 400 micrograms of salbutamol
- FVC pre and post 400 micrograms of salbutamol
8.2.3. Paediatric Asthma Quality of Life Questionnaire (PAQLQ)
The Quality of Life (QoL) scores obtained at different timepoints (T0, T + 8, T + 24 and T + 48) throughout the trial can be used as a subjective measure of efficacy. The PAQLQ, devised by Elizabeth Juniper, will measure the physical, emotional, occupational and social effects of asthma in children. There are two versions of the PAQLQ, interviewer administered for children 10 years & younger and patient administered for children 11 years & older. The RN will select the version appropriate for the individual child's age and stage of development. Children will be asked to recall information from the previous seven days and to use this when selecting their responses. The child's asthma may also affect the parents' quality of life and so an additional scale, the Paediatric Asthma Caregivers Quality of Life Questionnaire (PACQLQ), will also be used. The PACQLQ has been designed by Elizabeth Juniper to complement the PAQLQ.
The PAQLQ has been selected for use in MASCOT due to its short recall requirement and ability to detect small but clinically important changes that children experience as a result of treatment or fluctuation in their asthma. (See Section 8.5 for procedure).
8.3. Procedures for Assessing Safety
An assessment of adverse events will be undertaken at each study visit from baseline (T0) to study completion (T + 48). These reviews will be carried out by the PI or RN conducting the visit or telephone call.
Adverse event reporting is detailed fully in Section 10 (Pharmacovigilance).
8.4. Substudies
8.4.1. Genetic Study
The study will include the collection of DNA (from saliva) which will be securely stored at the University of Liverpool for pharmacogenetic analysis at a later date.
A separate consent process will be undertaken for this purpose at the T0 visit. All participants registered in the trial will be asked to provide a sample, regardless of whether they are eligible for the randomised phase. If consent and assent (where applicable) is provided at T0, the genetic sample will be collected by asking the child to spit directly into a collection kit. The kit is specifically designed for the preservation, transportation and purification of DNA from saliva and is a non-invasive, highly reliable method of DNA collection. The amount of saliva required from the participant is 2 ml so the child may have to spit more than once in order to obtain a sufficient amount of material for DNA extraction. Once the saliva has been deposited, the RN will then seal and label the container with the child's unique trial identifier number. When the kit has been sealed the sample will remain stable at room temperature. It will be sent directly to a central facility at the University of Liverpool where it will be stored for future study.
The genetic samples collected will be used in the future to help determine whether specific polymorphisms affect severity or long term prognosis of asthma and its symptoms. For the patients who enter the randomised part of the trial, the samples will also be used to explore the possibility that a difference may be seen in those children responding to long acting beta2 agonists (LABAs) or leukotriene receptor antagonists (LTRAs) dependent on specific single nucleotide polymorphisms (SNPs) within the beta2 agonist receptor or the leukotriene receptor genes. However, no specific study is planned at this time. Approval from a Research Ethics Committee will be sought before any pharmacogenetic analyses are conducted.
8.4.2. RECRUIT
It is proposed that MASCOT will involve a qualitative substudy ‘Processes in recruitment to randomised controlled trials (RCTs) of medicines for children (RECRUIT)’. RECRUIT was approved in its own right by the North West REC on 2nd March 2007 (ref 07/MRE08/6).
RECRUIT will be examining communication processes in the recruitment of participants to MASCOT with the aim of identifying strategies for subsequent trials of medicines for children to improve trial recruitment and conduct. RECRUIT will involve:
- Routine audio-recording of MASCOT discussions (consultations) between families and practitioners (trial recruiters)
- Follow-up interviews with up to eight families (parents and children, where aged seven or over) who agree to participate in MASCOT
- Follow-up interviews with up to eight families (parents and children, where aged seven or over) who decline to participate in MASCOT
- Follow-up interviews with up to eight trial recruiters involved in approaching families to take part in MASCOT
Collection of data for 1 will be facilitated by MASCOT staff who will routinely seek permission to audio-record recruitment consultations from the families whom they approach for MASCOT. Data for 2, 3 and 4 will be collected by the Research Associates (RAs) employed on RECRUIT, who will be entirely independent of MASCOT.
If permission for audio-recording is declined by a family the recruitment consultation will not be recorded. If permission is given the recruiter will activate an audio-recorder. At the end of the MASCOT recruitment consultation the recruiter will discuss RECRUIT with the family and seek their permission to pass their details to one of the RAs employed on RECRUIT, who will then make contact with families and obtain written informed consent for participation in the RECRUIT study. Recordings from families who decline RECRUIT will be erased as soon as practicable. All families who express an interest in RECRUIT but are not selected for follow-up interview will be contacted by letter to thank them and inform them that their recordings have been erased. Audio-recordings of the recruitment consultations will only be released to the RECRUIT RAs after the consent of the participants has been obtained.
All interviews for RECRUIT will be conducted by experienced RAs with proven skills in the conduct of research in sensitive settings. Any distress during the interviews will be managed with care and compassion by the RAs and participants will be free to decline to answer any questions that they do not wish to answer or to stop the interview at any point. The RAs will receive appropriate training and follow a clear protocol for managing participants whose level of distress gives cause for concern. Any such families will be supported in obtaining appropriate help. If necessary, and after discussion with the participant, the lead clinician responsible for the child's care will be informed.
To allow MASCOT to become established and avoid the initial ‘teething’ phase that most trials experience, sampling for RECRUIT will not begin until the trial has been recruiting for approximately four months. Sampling to RECRUIT (and therefore audio-recording of trial consultations) will roll from trial site to trial site in blocks of up to three months' duration, with planned suspensions if accrual to RECRUIT allows. This will help to minimise the numbers of families who are approached but not selected for RECRUIT. Concentrated sampling at particular sites in time-limited blocks, with the possibility of planned suspensions, will minimise the impact of RECRUIT on MASCOT and the risk of overburdening particular trial sites. It will also facilitate liaison with the sites and assist recruiters in routine audio-recording of consultations.
8.5. Other Assessments
Childhood asthma represents a significant economic burden to the health service, in terms of treatment and hospital admissions, and to society (the child and their carers) in terms of quality of life; lost schooling and lost time from productive employment (that is time off work caring for a sick child)14.
An economic analysis will be conducted primarily from a health service perspective but extended to examine a societal perspective by including the child and his/her carer's viewpoint. Both the child and carer's quality of life perspective can be measured using the Paediatric Asthma Quality of Life and Paediatric Asthma Caregivers Quality of Life questionnaires devised by Elizabeth Juniper. Further effects on the carer can be measured by adding additional questions for the carer concerning time lost to paid employment as a result of caring for the child suffering an asthma exacerbation.
The three interventions will be evaluated in terms of their costs and benefits.
Key costs will be use of health service resources; this will include the drugs, visits to general practitioners, home visits from primary health care workers, hospital admissions and A&E attendances. Primary care costs will be a key cost driver in this evaluation. The analysis will be extended to measure costs as they accrue to the patient and their carer. Additional questions will be administered concerning time lost to paid employment due to caring for a child with an asthma related illness. The health economics questionnaire will be lodged in the hand held record at T0, and collected from there at all data collection time points from T+8 to T+48. The data required on resources requires actual recollection of events, so patients and carers will be encouraged to complete the questionnaire on an ongoing basis.
The important measures of outcome will be exacerbations, quality of life, time off school for the child and time off work for parents and carers. The study will seek to measure outcome from both an effectiveness perspective e.g. reduction in exacerbations and reduction in visits to primary care and hospital admissions and from a utility perspective the Juniper measure of quality of life in children. Key outcome measures will be considered alongside the costs.
8.5.1. Health Economics
Health economic data will be collected on primary and secondary health care contacts and medications prescribed. Although not the primary focus of the study, it will aim to incorporate patient and societal costs in terms of time lost to school by the children and time lost to work for the parents and carers. It will include any out of pocket expenses such as personal money spent on medications and aids and appliances. It is important to determine differences in the patient pathway as a result of different regimes.
The four week run-in period can be ignored in terms of the economics as the costs will be common across all patients.
For participants entering the randomised phase, a blank Health Economics (HE) questionnaire will be inserted into their hand held record at each visit for the patient and their carer/s to complete over the following weeks up until their next appointment. This should increase the reliability and accuracy of the data collected by decreasing the family's reliance on retrospective recall of information. The family will receive a telephone call from the RN prior to their visit to remind them to complete and bring along the record and questionnaire for review at their next study appointment. During the visit, the HE questionnaire pages will be removed from the record by the RN. The original will be sent to CTU within seven days and copies made for the Site File and provided to the family (if requested). A new, blank questionnaire will then be inserted into the record for use until the next contact with the study team. At T+24 weeks an extra copy of the HE questionnaire will be inserted into the back of handheld record. At the telephone contact at T+36 weeks, patients/carers will be asked to swap the two questionnaires over and enter the start date on the new questionnaire. At T+48 both questionnaires will be collected from the hand held record.
8.5.2. Quality of Life
The Paediatric Asthma Quality of Life Questionnaire (PAQLQ) should be the first questionnaire completed during the clinic visit and should precede any discussion with the research doctor or nurse. Ideally, children should be interviewed on their own and in a quiet room where there are no distractions. Parents/carers should be instructed to wait in another room if possible, where they can complete the Paediatric Asthma Caregiver's Quality of Life Questionnaire (PACQLQ) while the child completes the PAQLQ. The child should be made to feel comfortable and relaxed but be aware that they need to complete the questionnaire carefully. Where the PAQLQ is interviewer administered (i.e. for children ten years of age and younger) then the questionnaires should be read out exactly as they appear on the form. They should not be reworded or paraphrased for the child, even if they ask for clarification. Children will be asked to base their responses on the past seven days and adults on the previous two weeks.
Two coloured cards (green and blue) will be provided with the PAQLQ, which list sets of response options appropriate to the different questions. The appropriate response card is listed with each question. The interviewer should explain both cards to the child, reading through each of the response options with the younger children and asking the older ones to read each of the responses aloud to ensure they understand them. Children should be reminded that they are only able to choose one option. The PACQLQ is in a self-administered format and carers should be instructed to follow the instructions on the questionnaire.
The research nurse should ensure that all questions have been answered. Once they have collected the completed questionnaires from the participant and their carer, they will make a copy and send the originals to CTU within seven days. The copy will be retained in the Site File. The questionnaires should, wherever possible, only be completed during the study visit .They must always be completed by the same caregiver who completed the first questionnaire and this should be the child's main carer.
8.6. Loss to Follow-up
If any of the trial patients are lost to follow up, contact will initially be attempted through the research nurse and lead investigator at each centre. If the lead investigator at the trial centre is not the patient's usual clinician responsible for their speciality care then follow-up will also be attempted through this latter clinician. Where these attempts are unsuccessful, the child's GP will be asked to contact the family and provide follow-up information to the recruiting centre. This information will be included on the patient information sheet. Wherever possible, information on the reason for loss to follow-up will be recorded.
8.7. Trial Closure
The end of the trial will be considered as the date of the final database lock. However the trial may be closed prematurely by the Trial Steering Committee, on the recommendation of the Independent Data and Safety Monitoring Committee.
9. STATISTICAL CONSIDERATIONS
9.1. Introduction
A separate and full statistical analysis plan (SAP) will be developed prior to the final analysis of the trial. The SAP will be agreed by the trial steering committee before being sent to the independent data and safety monitoring committee for comment and approval. The main features of these planned statistical analyses are included here in the main protocol.
9.2. Method of Randomisation
The randomisation code list will be generated by an MCRN CTU (who is not involved with the MASCOT study) with the software package STATA using block randomisation with variable block length. Randomisation will be stratified by Secondary Care Centre with allocation to the three treatment arms in the ratio of 1 : 1 : 1.
9.3. Outcome Measures
9.3.1. Primary
Number of asthma exacerbations requiring treatment with short courses of oral corticosteroids over 48 weeks from date of randomisation.
9.3.2. Secondary
- Quality of Life as measured by the Paediatric Asthma Quality of Life Questionnaire (PAQLQ) and the Paediatric Asthma Caregivers Quality of Life Questionnaire (PACQLQ)13
- Time from randomisation to first exacerbation requiring treatment with a short course of oral corticosteroids
- School attendance
- Hospital admissions
- Amount of rescue beta2 agonist therapy prescribed
- Time from randomisation to treatment withdrawal (due to lack of efficacy or side effects)
- Lung function at 48 weeks (as assessed by spirometry)
- Cost effectiveness
- Adverse events
9.4. Sample Size
The primary outcome ‘Number of asthma exacerbations requiring treatment with short courses of oral corticosteroids over 48 weeks’ will be modelled as a poisson random variable. The sample size for the primary outcome is estimated using the following formula as described by Friede and Schmidli (personal communication):
where nc is the number of patients in the control arm, λc is the control group rate, t is the length of follow-up and θ* the rate ratio. The formula above does not allow for overdispersion which would lead to an inflated sample size. A method of moments estimator for the dispersion parameter, where values greater than 1 indicates overdispersion, is given by:
For 1032 children who have had at least one course of oral steroid in the previous 12 months, the mean exacerbation rate per year is estimated from the UK General Practice Research Database as 1.5 per year with variance 1.02 and dispersion parameter 0.68. This is our current best estimate of exacerbation rate and dispersion parameter but may not be entirely representative of the MASCOT randomised population who will have had inhaler technique corrected. Therefore, a target sample size is estimated here with the intention of undertaking an internal blinded pilot to check parameter assumptions and adjust sample size if required. As described by Friede and Schmidli (personal communication), analogous formulae to those above based on the overall event rate across groups can be used to undertake a blinded sample size review (see section 9.5).
As there are three primary treatment comparisons, each will be tested at the two-sided significance level of 1.7% to adjust for the multiplicity and to give a study-wise 5% two-tailed significance level. To have power of 80% to detect, as significant, at least a 30% reduction in exacerbation rate (from 1.5 per year to 1.05 per year, equivalent to a rate ratio of 0.7) and allowing for a loss to follow up of 10%, 147 patients per group are required.
Thirteen main centres will participate in this study, with an anticipated total accrual for screening of around 75 patients per month across these sites, enabling recruitment of approximately 900 children over 12 months. Assuming either 50% or 75% of children to be eligible for randomisation after the 4 week run-in period would enable either 150 or 225 children to be randomised to each treatment group. The exact percentage of children who will be eligible for randomisation following the 4 week run-in period cannot be estimated yet but will be monitored closely to assess the likely impact on recruitment figures (see interim analysis section).
In summary, our preliminary target number to be randomised is 150 children per treatment group (450 total) with recruitment rates, percentage of children randomised and parameters for sample size calculations closely monitored.
Secondary outcome ‘Quality of Life’: With 150 children in each group, the power to detect, as significant, a difference of 0.5 points between treatment groups on the Juniper Paediatric Asthma Quality of Life Questionnaire, with assumed standard deviation 0.7113 is greater than 99%.
9.5. Interim Monitoring and Analyses
The estimate of overall exacerbation rate (not split by treatment group) and dispersion parameter will be checked after the first 75 children have been randomised and completed their 24 week follow-up assessment. This blinded internal pilot is anticipated to be undertaken at approximately 32 weeks after the first child is randomised. This figure has been chosen to provide adequate data for the sample size review but to ensure that the review is undertaken before the recruitment period ends. This blinded internal pilot will be reviewed by the Independent Data and Safety Monitoring Committee (IDSMC) prior to reviewing any unblinded comparative data. The initial analysis of trial data for IDSMC review is planned at 6 months after the first patient is randomised, to assess recruitment rates (including the percentage of children randomised after the 4 week run-in period) and toxicity.
Subsequent timing of the next analysis of the data will be determined on the basis of recruitment rates at the initial IDSMC meeting although it is anticipated that this will be approximately after a further 6 months. Additional interim analyses may also be triggered by a concern regarding Suspected Unexpected Serious Adverse Reactions (SUSARs).
It is noted that primary outcome data may not be available for the early interim analyses because of the time necessary (48 weeks) to follow-up participants to observe the end point. Any lack of important information will be taken into account by the IDSMC in their monitoring of the trial.
In order to estimate relative treatment effects for the primary efficacy outcome at each interim and final analysis, the Haybittle-Peto approach will be employed for 2 equally spaced interim analyses, planned after 1/3 and 2/3 of the target total number of children have been randomised and followed for 48 weeks, with 99.9% confidence intervals calculated for the difference between each pair of drugs. The final analysis will be undertaken after the final randomised child has completed 48 weeks follow-up and 95% confidence intervals will be calculated. This method has been chosen to ensure that interim efficacy results would have to be extreme before early termination is recommended in order to be convincing to the clinical community. The method also minimises controversy regarding interpretation of the results from estimation and hypothesis testing at the final analysis. No inflation factor needs to be applied to the sample size using this approach.
All interim analysis results of primary and secondary outcomes will be confidential to the IDSMC members and will not be for review by the trial management group (except the statistical team preparing the IDSMC report). The IDSMC members will make formal recommendations to the trial working group and TSC regarding the continuation of recruitment of patients into the study and will comply with a trial-specific IDSMC charter according to ICH GCP guidelines. The IDSMC may recommend to the TSC that the trial be stopped or amended if sufficient evidence emerges that one treatment is clearly indicated or contra-indicated, as considered by the IDSMC in light of the analyses presented, accounting for other emerging worldwide evidence and overall clinical relevance. The IDSMC will be asked to consider patient safety, particularly any Suspected Unexpected Serious Adverse Reactions (SUSARs) leading to death, alongside treatment efficacy when making their recommendation regarding continuation, amendment or discontinuation of the trial.
9.6. Analysis Plan
The study will be analysed and reported using the ‘Consolidated Standard of Reporting Trials’ (‘CONSORT’)15,16 and the ICH E9 guidelines.
A full and detailed statistical analysis plan will be written prior to the conduct of the final analysis according to the MCRN CTU Statistical Analysis Plan SOP. To provide a pragmatic comparison of the policies of the different treatments, primary analyses will be performed on an intention to treat basis, analysing all patients according to the treatment group originally allocated. A sensitivity analysis using the per protocol or complier average causal effect (CACE) population as appropriate will be explored to demonstrate robustness of the results. For the overall safety and tolerability assessment, the set of patients to be summarised will be defined as those subjects who received at least one dose of the study drug.
Missing data will be handled by considering the robustness of the complete case analysis to sensitivity analyses using different imputation assumptions informed by data collected on reasons for missing data. Data relating to the primary outcome (oral steroid usage) for those patients who fail to attend for the 48 week assessment visit can be obtained from their GP.
The primary outcome of number of asthma exacerbations requiring treatment with short courses of oral corticosteroids over 48 weeks will be compared between treatment groups using a Poisson regression model (adjusted for centre) with two dummy variables representing 3 treatment groups. Adjustment for overdispersion will be made if appropriate. A secondary analysis adjusting the model for other important prognostic factors (age, sex, duration of asthma, rhinitis, baseline AQLQ, baseline number of courses of oral steroids) will be explored. Statistical tests will be nominally performed at the 1.7% two-sided significance level (with corresponding 98.3% confidence interval), to give a study-wise 5% two-sided significance level (see sample size calculation). The relative exacerbation rate and confidence interval will be calculated for each pair-wise treatment comparison: A compared with B to evaluate the effect of adding in long acting beta-2 agonist (salmeterol 50 micrograms twice daily); A compared with C to evaluate the effect of adding in oral leukotriene receptor antagonist (montelukast 5 mg once daily); and B compared with C to evaluate the effect of adding in long acting beta-2 agonist (salmeterol 50 micrograms twice daily) compared with adding in oral leukotriene receptor antagonist tablet (montelukast 5 mg once daily).
For secondary outcomes statistical tests will be performed at the 5% two-sided significance level (with corresponding 95% confidence interval) unless indicated otherwise. Analyses will adjust by centre and secondary analyses adjusting for other important prognostic factors (age, sex, duration of asthma, rhinitis, baseline AQLQ, baseline number of courses of oral steroids) will be explored. For the secondary outcome quality of life, characteristics of responders and non-responders will be compared and potential biases assessed. The score on three domains of activity, symptoms and emotion measured by the Juniper Quality of Life scale, will be assessed over time and treatment groups compared using longitudinal analysis. A joint modelling approach where time to dropout is taken as the time to event outcome will also be used to explore relationships between dropout and outcome.
Time to first exacerbation requiring treatment with a short course of oral corticosteroids will be calculated for each child and compared across treatment groups using Kaplan-Meier curves and log-rank test with relative effects of treatments summarised using hazard ratios and 95% confidence intervals. The seasonality of having an asthma exacerbation episode will be explored by fitting season as a time-dependent covariate in the model for time to first exacerbation.
Time to withdrawal of randomized treatment will be calculated for each child and compared across treatment groups using Kaplan-Meier curves and log-rank test with relative effects of treatments summarised using hazard ratios and 95% confidence intervals. To examine different reasons for treatment withdrawal (competing risks of unacceptable adverse effects and inadequate asthma control) a cumulative incidence analysis will be undertaken. This approach does not assume competing risks are independent and allows the assessment of cause-specific withdrawal in the presence of other competing risks. All adverse events will be categorised appropriately and the number of patients with occurrences of each event summarised according to treatment group supplemented by calculation of confidence intervals wherever this aids interpretation.
The percentage of school days missed (transformed if appropriate) will be analysed and compared between treatment groups using analysis of variance. The number of hospital admissions will be summarised and compared between treatment groups using bootstrapping techniques which allow comparisons between groups to be based upon the mean difference while making allowance for the non-normal distribution in the calculation of confidence intervals and p-values (Metcalfe et al 200317). Lung function at 48 weeks will be compared between treatment groups using analysis of covariance (adjusted by baseline lung function). Number of doses of rescue beta2 agonist therapy prescribed over 48 weeks (transformed if appropriate) will be analysed and compared between treatment groups using analysis of variance. Blinded distribution data will be reviewed and the statistical analysis plan amended accordingly.
9.6.1. Economic analysis
Economic analysis will focus on determining the differences in the patient pathways between the three groups in terms of their costs and benefits. Analysis will therefore take a number of different forms.
Incremental Cost Effectiveness Ratios (ICER) will be calculated against the base case:
- A Inhaled fluticasone propionate 100 micrograms twice daily plus placebo tablet once daily.
The other two scenarios:
- B Inhaled fluticasone propionate 100 micrograms and salmeterol 50 micrograms twice daily (combination inhaler) plus placebo tablet once daily.
- C Inhaled fluticasone propionate 100 micrograms twice daily plus montelukast 5mg tablet once daily will be compared against the base case.
ICERs calculate the ratio of the difference in cost to the difference in outcome between the two groups. In terms of outcome, the ICER will be based on the difference in the number of exacerbations between the groups. Further ICERs based on quality of life could also be calculated.
Cost effectiveness acceptability curves (CEACs) will be calculated for each of the three regimes showing the probability that each option is cost effective at different willingness to pay thresholds.
A subsidiary economic analysis may evaluate the cost of exacerbations in terms of the average cost per exacerbation and then cost the treatment alternatives in terms of exacerbations averted. This subsidiary analysis is a useful supplement to the main analysis. Cases averted are a useful tool for presentation of the data.
10. PHARMACOVIGILANCE
10.1. Terms and Definitions
The Medicines for Human Use (Clinical Trials) Regulations 2004 (SI 2004/1031) definitions:
Adverse Event (AE)
Any untoward medical occurrence in a subject to whom a medicinal product has been administered, including occurrences which are not necessarily caused by or related to that product.
Adverse Reaction (AR)
Any untoward and unintended response in a subject to an investigational medicinal product which is related to any dose administered to that subject.
Unexpected Adverse Reaction (UAR)
An adverse reaction the nature and severity of which is not consistent with the information about the medicinal product in question set out in:
- In the case of a product with a marketing authorization, in the summary of product characteristics for that product
- In the case of any other investigational medicinal product, in the investigator's brochure relating to the trial in question.
Serious Adverse Event (SAE), Serious Adverse Reaction (SAR) or Suspected Unexpected Serious Adverse Reaction (SUSAR)
Any adverse event, adverse reaction or unexpected adverse reaction, respectively, that:
- results in death
- is life-threatening* (subject at immediate risk of death)
- requires in-patient hospitalisation or prolongation of existing hospitalisation**
- results in persistent or significant disability or incapacity, or consists of a congenital anomaly or birth defect
- Other important medical events
*‘life-threatening’ in the definition of ‘serious’ refers to an event in which the patient was at risk of death at the time of the event; it does not refer to an event which hypothetically might have caused death if it were more severe.
**Hospitalisation is defined as an inpatient admission, regardless of length of stay, even if the hospitalisation is a precautionary measure for continued observation. Hospitalisations for a pre-existing condition, including elective procedures that have not worsened, do not constitute an SAE.
***Other important medical events that may not result in death, be life-threatening, or require hospitalisation may be considered a serious adverse event/experience when, based upon appropriate medical judgment, they may jeopardise the subject and may require medical or surgical intervention to prevent one of the outcomes listed in this definition
10.2. Notes on Adverse Event Inclusions and Exclusions
10.2.1. Include
- An exacerbation of a pre-existing illness
- An increase in frequency or intensity of a pre-existing episodic event/condition
- A condition (even though it may have been present prior to the start of the trial) detected after trial drug administration
- Continuous persistent disease or symptoms present at baseline that worsens following the administration of the study/trial treatment
10.2.2. Do Not Include
- Medical or surgical procedures – the condition which leads to the procedure is the adverse event
- Pre-existing disease or conditions present before treatment that do not worsen
- Situations where an untoward medical occurrence has occurred e.g. cosmetic elective surgery
- Overdose of medication without signs or symptoms
- The disease being treated or associated symptoms/signs unless more severe than expected for the patient's condition
10.2.3. Reporting of Pregnancy
Study participants will not routinely be tested for pregnancy as part of the trial screening process. Any pregnancy which does occur during the course of the study should be reported to the MCRN CTU immediately. The investigator should discuss the risks of continuing with the pregnancy with the patient and the possible effects on the foetus if they continue on trial treatment. It is at the investigator's discretion to decide whether the individual should be instructed to stop taking study drugs. All pregnancies that occur during trial treatment, or within seven days of finishing treatment, need to be followed up until completion and reported separately.
10.3. Notes Severity/Grading of Adverse Events
The assignment of the severity/grading should be made by the investigator responsible for the care of the participant using the definitions below.
Regardless of the classification of an AE as serious or not, its severity must be assessed according to medical criteria alone using the following categories:
- Mild: does not interfere with routine activities
- Moderate: interferes with routine activities
- Severe: impossible to perform routine activities
A distinction is drawn between serious and severe AEs. Severity is a measure of intensity (see above) whereas seriousness is defined using the criteria in section 10.1, hence, a severe AE need not necessarily be a Serious Adverse Event.
10.4. Relationship to Trial Treatment
The assignment of the causality should be made by the investigator responsible for the care of the participant using the definitions in Table 3.
Table 3
Definitions of Causality
If any doubt about the causality exists the local investigator should inform the study coordinating centre who will notify the chief investigator. In the case of discrepant views on causality between the investigator and others, the MHRA will be informed of both points of view.
10.5. Expectedness
An AE whose causal relationship to the study drug is assessed by the investigator as ‘possible’, ‘probable’, or ‘almost certainly’ is an Adverse Drug Reaction.
All events judged by the investigator to be possibly, probably, or almost certainly related to the IMP, graded as serious and unexpected (see section 10.2 and SPCs for list of Expected Adverse Events) should be reported as a SUSAR.
10.6. Follow-up After Adverse Events
All adverse events should be followed until satisfactory resolution or until the investigator responsible for the care of the participant deems the event to be chronic or the patient to be stable.
When reporting SAEs and SUSARs the investigator responsible for the care of the participant should apply the following criteria to provide information relating to event outcomes: resolved; resolved with sequelae (specifying with additional narrative); not resolved/ongoing; ongoing at final follow-up; fatal or unknown.
10.7. Reporting Procedures
All adverse events should be reported. Depending on the nature of the event the reporting procedures below should be followed. All adverse events will be reported and recorded from the point that the participant provides informed consent and throughout the trial treatment period up until seven days after the patient has taken the final dose of investigational medicinal product. Any questions concerning adverse event reporting should be directed to the MCRN CTU in the first instance. A flowchart is given below to aid in determining reporting requirements.
10.7.1. Non serious ARs/AEs
All such events, whether expected or not, should be recorded on an Adverse Event Form, which should be transmitted to the MCRN CTU within seven days of the form being due.
10.7.2. Serious ARs/AEs/SUSARs
SARs, SAEs and SUSARs should be reported within 24 hours of the local site becoming aware of the event. The SAE form asks for the nature of event, date of onset, severity, corrective therapies given, outcome and causality. The responsible investigator should sign the causality of the event. Additional information should be sent within 5 days if the reaction has not resolved at the time of reporting.
The MCRN CTU will notify the MHRA and main REC of all SUSARs occurring during the study according to the following timelines; fatal and life-threatening within 7 days of notification and non-life threatening within 15 days. All investigators will be informed of all SUSARs occurring throughout the study. Local investigators should report any SUSARs and/or SAEs as required by their local Research & Development (R&D) Office.
10.8. Responsibilities – Investigator
The Investigator is responsible for reporting all AEs that are observed or reported during the study, regardless of their relationship to study product.
All SAEs must be reported immediately by the investigator to the MCRN CTU on an SAE form unless the SAE is specified in the protocol or SPC as not requiring immediate reporting. All other adverse events should be reported on the regular progress/follow-up reports.
Minimum information required for reporting
- Study identifier
- Study centre
- Patient number
- A description of the event
- Date of onset
- Current status
- Whether study treatment was discontinued
- The reason why the event is classified as serious
- Investigator assessment of the association between the event and study treatment
- The SAE form should be completed by the responsible investigator i.e. the consultant named on the ‘signature list and delegation of responsibilities log’ who is responsible for the patient's care. The investigator should assess the SAE for the likelihood that that it is a response to an investigational medicine. In the absence of the responsible investigator the form should be completed and signed by a designated member of the site trial team and faxed to the MCRN CTU immediately. The responsible investigator should check the SAE form, make changes as appropriate, sign and then re-fax to the MCRN CTU as soon as possible. The initial report shall be followed by detailed, written reports.
- Send the SAE form by fax (within 24 hours or next working day) to the MCRN CTU: Fax Number: 0151 282 4721
- The responsible investigator must notify their local R&D department of the event (as per standard local procedure).
- In the case of an SAE the subject must be followed-up until clinical recovery is complete and laboratory results have returned to normal, or until the event has stabilised. Follow-up may continue after completion of protocol treatment if necessary.
- Follow-up information is noted on another SAE form by ticking the box marked ‘follow-up’ and faxing to the MCRN CTU as information becomes available. Extra, annotated information and/or copies of test results may be provided separately.
- The patient must be identified by trial number, date of birth and initials only. The patient's name should not be used on any correspondence.
10.8.1. Maintenance of Blinding
Systems for SUSAR and SAR reporting should, as far as possible, maintain blinding of individual clinicians and of trials staff involved in the day-to-day running of the trial. Unblinding clinicians may be unavoidable if the information is necessary for the medical management of particular patients. The safety of patients in the trial always takes priority. In each report, seriousness, causality and expectedness should be evaluated for all of the trial treatments unless criteria have been fulfilled (section 7.8) and unblinding has taken place. Cases that are considered serious, unexpected and possibly, probably or almost certainly related to one of the trial therapies (i.e. possible SUSARs) would have to be unblinded at the clinical trials unit prior to reporting to the regulator.
10.9. Responsibilities – MCRN CTU
The MCRN CTU is undertaking duties delegated by the trial co-sponsors, Keele University and University Hospital of North Staffordshire NHS Trust, and is responsible for the reporting of SUSARs and other SARs to the regulatory authorities (MHRA and, if required, the research ethics committees) as follows:
- SUSARs which are fatal or life-threatening must be reported not later than 7 days after the MCRN CTU is first aware of the reaction. Any additional relevant information must be reported within a further 8 days.
- SUSARs that are not fatal or life-threatening must be reported within 15 days of the MCRN CTU first becoming aware of the reaction.
- A list of all SARs (expected and unexpected) must be reported annually.
It is recommended that the following safety issues should also be reported in an expedited fashion:
- An increase in the rate of occurrence or a qualitative change of an expected serious adverse reaction, which is judged to be clinically important;
- Post-study SUSARs that occur after the patient has completed a clinical trial and are notified by the investigator to the sponsor;
- New events related to the conduct of the trial or the development of the IMPs and likely to affect the safety of the subjects, such as:
- A serious adverse event which could be associated with the trial procedures and which could modify the conduct of the trial;
- A significant hazard to the subject population, such as lack of efficacy of an IMP used for the treatment of a life-threatening disease;
- A major safety finding from a newly completed animal study (such as carcinogenicity).
- Any anticipated end or temporary halt of a trial for safety reasons and conducted with the same IMP in another country by the same sponsor;
- Recommendations of the Data Monitoring Committee, if any, where relevant for the safety of the subjects.
Staff at the MCRN CTU will liaise with the chief investigator (or, as specified in the protocol, Professor David Price) who will evaluate all SAEs received for seriousness, expectedness and causality. Investigator reports of suspected SARs will be reviewed immediately and those that are SUSARs identified and reported to regulatory authorities and MREC. The causality assessment given by the local investigator at the hospital cannot be overruled and in the case of disagreement, both opinions will be provided with the report.
The MCRN CTU will also send an annual safety report containing a list of all SARs to regulatory authorities and MREC. Copies of the report will be sent to the principal investigator at all institutions participating in the trial.
Patient safety incidents that take place in the course of research should be reported to the National Patient Safety Agency (NPSA) by each participating NHS Trust in accordance with local reporting procedures.
11. ETHICAL CONSIDERATIONS
11.1. Ethical Considerations
The study will abide by the principles of the World Medical Association Declaration of Helsinki (1964) and the Tokyo (1975), Venice (1983), Hong Kong (1989) and South Africa (1996).
We consider the specific ethical issues relating to participation in this trial to be:
- Informed consent in a paediatric population: The parent or legal representative of the child will have an interview with the investigator, or a designated member of the investigating team, during which opportunity will be given to understand the objectives, risks and inconveniences of the trial and the conditions under which it is to be conducted. They will be provided with written information and contact details of the study nurse, from whom further information about the trial may be obtained, and will be made aware of their right to withdraw the child from the trial at any time without the child or family being subject to any detriment in the child's treatment. Children will receive information, according to their capacity of understanding, about the trial and its risks and benefits and their assent will be obtained, where appropriate.
- The taking of a placebo treatment or active treatment (fluticasone, salmeterol or montelukast): The families will be informed about the National Guidelines and that there are various choices open to patients and carers with regard to asthma treatment. It is important that the family understands that no one will know which treatment the child is receiving due to the lack of scientific information as to which choice is better. All three treatment groups are potentially effective but it is possible that one may be better for one child than another.
- DNA sampling: The samples will be labelled with the participant's trial identifier number. The purpose of undertaking genetic testing at some point in the future will be to determine whether those patients with specific polymorphisms differ in their response to particular treatments or whether specific polymorphisms affect severity or long term prognosis of asthma and its symptoms. The genetic study will be subject to a separate consent process (using a separate information sheet) to the main study and participants who refuse to take part will not be precluded from entry into MASCOT. The consent obtained will be related to genetic studies in asthma only. The DNA collected will not be used for any other genetic studies. Information about individual patients will not be available at any time but all participants will be informed of the outcome of the study and the outcome of any DNA analysis by publishing the final trial report on the public access area of the NIHR portal.
- Ineligibility of non-English speakers: To include non-English speakers in the trial would require appropriate translations of all trial documentation and correspondence provided to participants, which would need to be fully checked and validated. Unfortunately there are not the resources within the trial to adequately provide this. The design of the trial also necessitates study visits to be held in primary care settings in some regions, which do not routinely have translation services available. In addition, the study specifies a telephone call at week 36 (T+36) between the RN and the patient and/or their carer/s, which would not be possible if they were unable to communicate in the same language. For these reasons, we must therefore limit trial entry to English speakers only.
11.2. Ethical Approval
The trial protocol will be submitted for the approval of the North West Research Ethics Committee (REC). Each participating centre must also undergo site specific assessment (SSA). A copy of local NHS Research & Development (R&D) approval and of the Patient Information sheet and Consent form (PISC) on local headed paper should be forwarded to MCRN CTU before patients are recruited into the study at that site. The CTU should receive notification of positive SSA for each new centre via the main REC. This will be through the chief investigator (Prof Warren Lenney) who is the main REC applicant. Details of any amendments to the original approved version of the protocol, which have subsequently been ethically approved, are indexed in Section 18.
Proxy consent from the parent or legally acceptable representative should be obtained prior to each patient registering in the trial after a full explanation has been given of the treatment options, including the conventional and generally accepted methods of treatment. Age and stage-of-development specific Patient Information and Consent leaflets should also be implemented and patient assent obtained (where appropriate). The right of the parent/legal representative to refuse consent for the minor to participate in the trial without giving reasons must be respected. After the patient has entered the trial, the clinician must remain free to give alternative treatment to that specified in the protocol at any stage if he/she feels it to be in the best interest of the patient. However, the reason for doing so should be recorded and the patient will remain within the trial for the purpose of follow-up and data analysis according to the treatment option to which they have been allocated. Similarly, the parent/legal representative of the patient remains free to withdraw the patient at any time from the protocol treatment and trial follow-up without giving reasons and without prejudicing the further treatment of the minor.
11.3. Informed Consent Process
11.3.1. General
Informed consent is a process initiated prior to an individual agreeing to participate in a trial and continues throughout the individual's participation. Informed consent is required for all patients participating in MCRN CTU coordinated trials. In obtaining and documenting informed consent, the investigator should comply with applicable regulatory requirements and should adhere to GCP and to the ethical principles that have their origin in the Declaration of Helsinki. Informed consent should only be taken by staff who are appropriately trained to do so and who have experience in providing information to minors.
Parental and age and stage-of-development appropriate Patient Information Sheet and Consent (PISC) forms, which will have been approved by an independent ethics committee (IEC), will be issued to potentially eligible patients and their families. The PISC will describe in detail the trial procedures (for both the run-in and randomised treatment phases), the trial interventions/products and potential risks and benefits of taking part in the study. All patients and their families will receive the appropriate version of the written information and be asked to read and review it. The PISC will emphasise that participation in the trial is voluntary and that the parent or legal representative* may, without the minor being subject to any resulting detriment, withdraw them from the trial at any time by revoking the informed consent. The rights and welfare of the patient will be protected by emphasising to them that the quality of medical care will not be adversely affected if they decline to participate in this study. All parents/legally acceptable representatives and patients will be given the opportunity to ask questions and will be given sufficient time to consider trial entry before consenting. They should have the opportunity to discuss the study with their usual medical practitioner and/or family/friends prior to agreeing to participate. The consent form will request permission for the patient's General Practitioner to be informed of their registration into the trial and also permission for personnel involved in the research or from regulatory authorities to have access to the individual's medical records. A copy of the informed consent/assent document will be given to the patient and their legally acceptable representative for their records.
*A mother always has legal responsibility for her child, however a father only has legal responsibility if he is married to the mother or has acquired legal responsibility for his child in the following ways:
- For children born before 1 December 2003, unmarried fathers can get parental responsibility by:
- marrying the mother of their child or by obtaining a parental responsibility order from the court
- registering a parental responsibility agreement with the court or by an application to court
- For children born after 1 December 2003, unmarried fathers can get parental responsibility by:
- registering the child's birth jointly with the mother at the time of birth
- re-registering the birth if you are the natural father
- marrying the mother of their child or by obtaining a parental responsibility order from the court
- registering with the court for parental responsibility
11.3.2. Obtaining Informed Consent
The consent process will be carried out by an appropriate researcher identified in the trial signature and delegation log. The consent process will be conducted by a researcher with training and experience with minors. The researcher delegated to obtain informed consent will be determined on a site by site basis, depending on the experience and knowledge of the individual staff at that site. Only personnel confident and competent to do so will be able to obtain informed consent. This can include PIs, other delegated investigators and research nurses. Where informed consent is being obtained by a research nurse, the patient and their family should have access to a clinician with expertise in paediatric respiratory medicine if they have any concerns about participation or any further questions that the nurse is unable to sufficiently answer.
Upon reviewing the PISC with the patient and their parent/s or legal representative, the researcher who is obtaining consent will fully explain the research study (both the run-in and randomised treatment phases) to the patient and their parent/legal representative and answer any questions they may have. They will discuss the objectives of the study and all potential benefits and inconveniences of taking part. They will clearly outline all of the responsibilities the patient and their family will be expected to meet if they agree to participate, including attendance at study visits and compliance with trial medications. A contact point where further information about the trial may be obtained will be provided. The patient and their family will be made aware that entry into the randomised phase of the trial is contingent on their continuing to meet the eligibility criteria following the four week run-in, as well as their continuing consent/assent to participate in the trial.
Both parental consent and the patient's assent, if appropriate, will be obtained prior to any study related procedures being carried out. The researcher and the parent/legal representative of the minor must personally sign and date the form. If capable, the patient should assent and personally sign and date the assent form. Assent forms do not substitute for the consent form signed by the patient's legally acceptable representative. Where the child is unable to provide assent, this should be documented in the patient's medical notes and recorded on a copy of the age and stage of development specific PISC. The original assent form should be filed in the medical notes and copies placed in the site file and forwarded to the MCRN CTU.
The original copy of the consent/assent form will be retained in the patient's medical notes and must be available for inspection. A copy will be returned to the MCRN CTU and one will also be placed in the Site File. A further copy of the signed consent/assent form will be provided to the child's parent/legally acceptable representative along with the PISC used during the recruitment consultation.
Following the four week run-in phase, any patients continuing to meet the eligibility criteria will progress to the randomised part of the trial. Once they have been found to be eligible, prior to randomisation, the researcher will reiterate previous written and verbal explanations about the trial and answer any further questions the family may have. The patient and their parent/s or legally acceptable representative will be asked to provide verbal consent (and assent, where appropriate) for their continued participation in the trial.
11.3.3. Informed Consent for DNA Collection
Consent for obtaining DNA in the form of saliva will be discussed initially at the T–4 study visit. All participants registered in the trial will be provided with a copy of a parental and age and stage of development specific PISC, approved by an IEC and developed specifically for the sub-study. They will have the opportunity to ask any questions and to discuss the sub-study with their usual medical practitioner and/or family/friends prior to making their decision.
Consent for participation in the genetic sub-study will be obtained at the T0 visit by the researcher identified in the site signature and delegation log. They will discuss the objectives of the study and all potential benefits and inconveniences of taking part. Participants and their families will be made aware that they are consenting for the DNA to be collected and stored for analysis at a later date. It will be made clear that the DNA specimen will be used only for analysis of specific genetic polymorphisms relating to asthma severity and outcomes and the steps that will be taken to maintain the confidentiality of the data.
Both parental consent and patient assent, if appropriate, will be obtained prior to the collection of the DNA sample. The research practitioner and the parent/legal representative of the minor must personally sign and date the form. If capable, the patient should assent and personally sign and date the assent form. Assent forms do not substitute for the consent form signed by the patient's legally acceptable representative.
The original copy of the consent/assent form will be retained in the patient's medical notes and must be available for inspection. A copy will be returned to the MCRN CTU and one will also be placed in the Site File. A further copy of the signed consent/assent form will be provided to the child's parent/legally acceptable representative along with the Patient Information Sheet relating to the trial.
11.4. Study Discontinuation
In the event that the study is discontinued, children will be treated according to usual standard clinical care. Patients withdrawing early from the trial as a whole will be unblinded within seven days of the local team becoming aware of their decision. Patients who withdraw early from trial treatment but continue to allow data collection and follow-up will have a discussion with the PI or investigator as to whether they will be unblinded at that point or wait until the end of their 48 week follow-up period. The decision will be based on the patient and their carers' own preferences and whether the investigator feels they need to be aware of the patient's randomised treatment allocation in order to provide appropriate follow on care.
12. REGULATORY APPROVAL
This trial is registered with the Medicines and Healthcare products Regulatory Agency (MHRA) and has been granted a Clinical Trial Authorisation (CTA). The EudraCT number is 2008–000511–16.
13. TRIAL MONITORING
Trial monitoring is carried out to ensure that the rights and well-being of human participants are protected during the course of a clinical trial. A risk assessment is performed for each trial co-ordinated by the MCRN CTU to determine the level and type of monitoring required for specific hazards. The type of trial monitoring should be specific to the individual trial and can take the form of on-site visits or central monitoring.
13.1. Risk Assessment
In accordance with the MCRN CTU Standard Operating Procedure (TM005) this trial has undergone a risk assessment, completed in partnership between the University of Liverpool, MCRN CTU, trial co-sponsors and the chief investigator, Prof Warren Lenney. In conducting this risk assessment, the contributors considered potential patient, organisational and study hazards, the likelihood of their occurrence and resulting impact should they occur.
The outcome of the risk assessment is expressed as a percentage, assigned according to the following categories:
- Score ≤ 33% = Low risk
- Score ≥ 34 to ≤ 67% = Moderate risk
- Score ≥ 68 to ≤ 100% = High risk
The outcome of the MASCOT trial risk assessment was a score of 18.3% therefore it has been judged to be a low risk clinical trial. This level of risk has determined the approach to trial monitoring described in this section and additionally in Section 16.
13.2. Source Documents
- Source data: All information in original records and certified copies of original records of clinical findings, observations, or other activities in a clinical trial necessary for the reconstruction and evaluation of the trial. Source data are contained in source documents (original records or certified copies). (ICH E6, 1.51).
- Source document: Original documents, data, and records (e.g. hospital records, clinical and office charts, laboratory notes, memoranda, subjects diaries or evaluation checklists, pharmacy dispensing records, recorded data from automated instruments, copies or transcriptions certified after verification as being accurate copies, microfiches, photographic negatives, microfilm or magnetic media, x-rays, subject files, and records kept at the pharmacy, at the laboratories and at medico-technical departments involved in the clinical trial). (ICH E6, 1.52).
In order to resolve possible discrepancies between information appearing in the Case Report Form (CRF) and any other patient related documents, it is important to know what constitutes the source document and therefore the source data for all information in the CRF. The following data recorded in the CRF should be consistent and verifiable with source data in source documents other than the CRF (eg medical record, laboratory reports and nurses' notes).
The following parameters that will be documented in the CRF are not source data:
- Relevant medical history and diagnosis (medical notes are source documents)
- Data for evaluation of eligibility criteria (medical notes are source documents)
- Physical examinations and assessments (medical notes are source documents)
- Concomitant medications (including changes) and diagnoses (medical notes are source documents)
- Dispensing of trial medication (pharmacy records are source documents)
- Adverse events (medical notes are source documents)
For data where no prior record exists and which is recorded directly onto the trial Case Report Forms, e.g. quality of life evaluations, the Case Report Form will be considered the source document, unless otherwise indicated by the investigator. All such exemptions should be identified prior to the clinical phase of the trial.
In addition to the above, date of conducting informed consent and assent process including date of provision of patient information, individual screening study number, unique randomised trial number and the fact that the patient is participating in a clinical trial comprising three treatment arms of inhaled fluticasone propionate and placebo tablet versus inhaled fluticasone propionate and salmeterol (combination inhaler) plus placebo tablet versus inhaled fluticasone propionate and montelukast tablet should be added to the patient's medical record chronologically, i.e. when treatment is allocated to the patient. Further, study treatment allocation should also be noted in the patient's medical record after unblinding of the study (see Section 7.8).
13.3. Data Capture Methods
Trial data will be captured using paper based Case Report Forms (CRFs).
13.3.1. Case Report Forms
The study case report form (CRF) is the primary data collection instrument for the study. All data requested on the CRF must be recorded and all missing data must be explained. If a space on the CRF is left blank because the procedure was not done or the question was not asked, ‘N/D’ must be written. If the item is not applicable to the individual case, write ‘N/A’. All entries should be printed legibly in black ink. If any entry error has been made, to correct such an error, draw a single straight line through the incorrect entry and enter the correct data above it. All such changes must be initialled and dated. DO NOT ERASE OR WHITE OUT ERRORS. For clarification of illegible or uncertain entries, print the clarification above the item, then initial and date it. CRF pages will be provided in triplicate on No Carbon Required (NCR) paper and when complete, should be split into three collated sets. Originals should be sent to the MCRN CTU and the copies securely retained at site.
Screening logs should be maintained at site and submitted monthly to the MCRN CTU. The screening log will be used to record patients (in an anonymised format) who register in the trial and patients who:
- Contact the research team after receiving information about MASCOT but decline to take part after talking to the research doctor/nurse about the trial
- Were referred inappropriately by their GP, nurse or hospital clinician
- Attended the T–4 visit but declined to consent
- Consented to the trial at T–4 but were found to be ineligible
Registration and randomisation CRFs should be submitted to the MCRN CTU within seven days of patients being registered or randomised onto the study. All other routine CRFs should be completed and submitted to the CTU within seven days of the study visit occurring. SAEs, SARs and SUSARs should be reported as detailed in Section 10.
Health Economics questionnaires will be completed by the patient and their carer/s as paper records and will be collected by the RN at each study visit. They will check them with the family for completeness and query any omissions (where appropriate). The RN should retain a copy for their Site File and return the original to the CTU within seven days of the study visit occurring. A copy should also be provided to the family if requested. A Quality of Life (QoL) questionnaire will be administered at each study visit as a paper record. The above procedure and timelines should be followed (original to CTU within seven days, copies for patient site trial records and family if requested).
13.4. Data Monitoring at MCRN CTU
The MCRN CTU will review recruitment rates, withdrawals and losses to follow-up and identified problems will be reviewed by the TMG. Remedial action will be taken as necessary. Completed CRFs submitted to the CTU will be centrally monitored to ensure that data collected are consistent with adherence to the trial protocol. Data will be checked for missing or unusual values (range checks) and checked for consistency within participants over time. Discrepancies that have been raised will be queried with the RN/PI. They will be sent a data query form highlighting the discrepancy and asked to check the recorded information against the source data and either confirm or correct the recorded data as appropriate. All corrections and clarifications should be documented on the relevant data query form which must be signed off by a member of the research team who is authorised to do so on the site signature and delegation log. A copy of the completed data query form should be returned to CTU and the site's original copy should also be filed with the CRF it relates to. CTU will send reminders for any overdue or missing data queries.
13.5. Central and Clinical Site Monitoring
13.5.1. Central Monitoring
The MCRN CTU is to receive a copy of the PISC within a week of randomisation. If consent forms are not forwarded regularly by a participating centre, the Trial Coordinator will conduct a site visit to check the presence of a signed PISC in the medical notes of all registered patients.
Data submitted to the database will be centrally monitored by the CTU to ensure, as far as possible, that CRF data collected are consistent with adherence to the trial protocol. Data will be checked for missing or unusual values (range checks) and checked for consistency within participants over time. Discrepancies that have been raised will be queried. The MACRO data management system will automatically keep a log of what data has been changed, the time of each change, and the person who changed it.
The Trial Coordinator will review rates of recruitment, missing outcome data, SAEs, ADRs, study withdrawals and losses to follow-up across sites, and remedial action taken as necessary. The Trial Coordinator may arrange site visits to undertake source data verification.
Standardised paper Case Report Forms (CRFs) should be sent to the MCRN CTU promptly. The Trial Data Manager will conduct data entry checks and use automated validation checks at data entry. A site visit will be conducted if inconsistencies, unresolved queries, missing data are consistently noted at a given site.
Monthly recruitment reports will be provided by the Trial Coordinator, monitoring reasons cited for consent refusal and querying reasons for slow recruitment. The TMG is charged with providing solutions to problems where possible.
The Trial Coordinator will keep a central protocol deviation log which will be updated with all deviations reported from trial sites. If the Trial Coordinator identifies significant and/or persistent non-compliance on the part of the PI, this will be documented in the monitoring report and the MCRN CTU team will discuss any further action required. A site visit will be conducted if primary and secondary measures are consistently missing from a given site. The Trial Coordinator will be in regular contact with the PIs in order to monitor the impact that the study may have on the running of the service.
13.5.2. Site Monitoring
Site monitoring may be deemed to be necessary as a result of central data checks. In order to perform their role effectively, a member of the MCRN CTU staff (usually the Trial Coordinator) may need direct access to primary data, e.g. patient records, laboratory reports, appointment books, etc. Since this affects the patient's confidentiality, this fact is included in the Patient Information Sheet and Informed Consent Form.
13.5.3. Confidentiality
Individual participants' medical information obtained as a result of this study is considered confidential and disclosure to third parties is prohibited with the exceptions below.
Case report forms will be labelled with patient initials and a unique trial registration and/or randomisation number. DNA samples will be transferred to an external laboratory and will be identified by unique identifiers only. Medical information may be given to the participant's medical team and all appropriate medical personnel responsible for the participant's welfare.
Verification of appropriate informed consent will be enabled by the provision of copies of participants' signed informed consent/assent forms being supplied to the MCRN CTU by recruiting centres. This requires that name data will be transferred to the MCRN CTU, which is explained in the PISC. The MCRN CTU will preserve the confidentiality of participants taking part in the study and the University of Liverpool is a Data Controller registered with the Information Commissioners Office.
13.5.4. Quality Assurance and Quality Control of Data
QA includes all the planned and systematic actions established to ensure the trial is performed and data generated, documented/recorded and reported in compliance with applicable regulatory requirements. QC includes the operational techniques and activities done within the QA system to verify that the requirements for quality of the trial-related activities are fulfilled.
This trial has undergone a risk assessment, the outcome of which indicates that it is a low risk trial. As such, site visits will be conducted and source data verification performed only if indicated to be necessary as a result of central monitoring. To this end:
- The PI, RN and designated pharmacist from each centre will attend the trial launch meeting, coordinated by the MCRN CTU in conjunction with the chief investigator, which will incorporate elements of trial specific training necessary to fulfil the requirements of the protocol
- The Trial Coordinator is to verify appropriate approvals are in place prior to the initiation of a site and that relevant personnel have attended site specific training
- The internal QA process of the MCRN CTU involves routine audit of certain activities across all trials, including random checking of adherence to informed consent procedure (monitoring receipt of signed consent forms)
- The Trial Coordinator and Trial Statistician are to check safety reporting rates between centres
- The Trial Coordinator and Trial Statistician are to monitor screening, recruitment and drop out rates between centres
- The Trial Data Manager is to conduct data entry consistency checks and follow up data queries until resolved
- Independent oversight of the trial will be provided by the Data Monitoring Committee and independent members of the Trial Steering Committee
13.6. Records Retention
The investigator at each investigational site must make arrangements to store the essential trial documents, including the Investigator Site File, until the MCRN CTU informs the investigator that the documents are no longer to be retained, or for a maximum of 15 years, whichever is soonest.
In addition, the PI is responsible for the archiving of all relevant source documents so that the trial data can be compared against source data after completion of the trial (e.g. in case of inspection from authorities).The PI is required to ensure the continued storage of the documents, even if they leave the clinic/practice or retires before the end of the required storage period. Delegation should be documented in writing.
The MCRN Clinical Trials Unit undertakes to store originally completed CRFs and separate copies of the above documents for the same period, except for source documents pertaining to the individual investigational site, which are kept by the PI only.
14. INDEMNITY
MASCOT is co-sponsored by Keele University and University Hospital of North Staffordshire NHS Trust and co-ordinated by the MCRN CTU in the University of Liverpool. As this is an investigator-initiated study, The Association of the British Pharmaceutical Industry (ABPI) guidelines for patient compensation by the pharmaceutical industry do not apply. However, in terms of liability NHS Trust and Non-Trust Hospitals have a duty of care to patients treated, whether or not the patient is taking part in a clinical trial, and they are legally liable for the negligent acts and omission of their employees. With regards to the MASCOT trial, University Hospital North Staffordshire NHS Trust will provide an indemnity in respect of clinical negligence to the extent that such an indemnity is permitted by the NHS Litigation Authority's Clinical Negligence Scheme for Trusts.
For General Practitioners participating in the MASCOT trial, indemnity in respect of clinical negligence will be provided through their Primary Care Trust (if they are employed through that PCT) following approval of the trial by their Research Office. Where an independent contractor (a GP or their practice staff working under a contract for services to a Primary Care Trust), undertakes research as part of their routine clinical services, their personal professional indemnity arrangements will provide them with adequate cover for this activity for their own practice patients. GPs involved in MASCOT, who are independent contractors, will inform their indemnity providers (e.g. MDU, MPS) of their participation in the study prior to the start of recruitment.
Clinical negligence is defined as
A breach of duty of care by members of the health care professions employed by NHS bodies or by others consequent on decisions or judgments made by members of those professions acting in their professional capacity in the course of their employment, and which are admitted as negligent by the employer or are determined as such through the legal process.
This study is funded by the Health Technology Assessment programme (HTA) of the Department of Health. Contractual agreements will be in place between sponsor and collaborating sites that will incorporate financial arrangements.
15. FINANCIAL ARRANGEMENTS
15.1. Participant Payments
Patients will be paid up to £8 per visit to cover any expenses incurred as a result of travelling to the centre for their study visit. This will be monitored by collecting tickets and receipts for those travelling via public transport and asking families who have travelled to the centre by private car to complete a mileage form.
15.2. Identification Payments
A nominal sum of £25 per patient registered for the four week run-in is allocated to be paid to the relevant healthcare provider (e.g. a GP practice) for provision of administration costs.
15.3. Pharmacy Departments
The dispensing service for the trial will be provided by the pharmacy department in each of the secondary care hubs. Provision of payment to support pharmacy costs (setup, storage, dispensing, reconciliation and GCP quality assurance), totalling £200 per participating site plus an additional fee of £10 per patient randomised has been allocated.
16. TRIAL COMMITTEES
16.1. Trial Management Group (TMG)
The Trial Management Group (TMG) will comprise Prof Warren Lenney, Prof Paula Williamson, Dr Catrin Tudur-Smith, Miss Sophie Perry, Prof David Price, Prof Marilyn James, Ms Sadie Clayton, Dr Jonathan Couriel and Ms Nemonie Marriott. The TMG will be responsible for the day-to-day running and management of the trial and will meet/teleconference approximately every two months during the first year and appropriately after that.
16.2. Trial Steering Committee (TSC)
The Trial Steering Committee (TSC) will consist of an independent chairperson, Dr Anne Thomson (Consultant in Paediatric Respiratory Medicine and General Paediatrics), two independent experts in the field of respiratory paediatrics, (Dr Gary Connett and Dr Iolo Doull), a biostatistician (Prof Chris Frost) and two lay representatives (Mr John Hilton and Mrs Ro Hilton) together with members from the TMG. The role of the TSC is to provide overall supervision for the trial and provide advice to the funder and the sponsor through its independent chairperson. The ultimate decision for the continuation of the trial lies with the TSC.
16.3. Independent Data and Safety Monitoring Committee (IDSMC)
The independent Data and Safety Monitoring Committee (IDSMC) consists of an independent chairperson, Dr David Spencer (Consultant in Respiratory Paediatrics), plus two independent members: Dr John Alexander, who is an expert in the field of paediatric medicine, and Mr Andy Vail, an expert in medical statistics.
The IDSMC will be responsible for reviewing and assessing recruitment, interim monitoring of safety and effectiveness, trial conduct and external data. The IDSMC will first convene before recruitment begins and will then define frequency of subsequent meetings (at least annually). Details of the interim analysis and monitoring plans are provided in section 9.
The IDSMC will provide a written recommendation to the Trial Steering Committee concerning the continuation of the study.
17. PUBLICATION
The results from different centres will be analysed together and published as soon as possible after the close of the trial. Individual clinicians must undertake not to submit any part of their individual data for publication without the prior consent of the Trial Management Group.
The Uniform Requirements for Manuscripts Submitted to Biomedical Journals (http://www.icmje.org/) and the CONSORT guidelines14,15 will be respected. The ISRCTN allocated to this trial should be attached to any publications resulting from this trial.
BMJ guidance on authorship and contributorship (see http://bmj.com/advice/3.html) will be use to acknowledge the level and nature of contribution of key individuals in publications arising from the trial. The publication strategy shall lie under the jurisdiction of the Trial Steering Committee.
18. PROTOCOL AMENDMENTS
18.1. Version 2.0 (19/Mar/2008)
Amendments and clarifications prior to full ethical approval (v1.0 22/Jan/2008 to v2.0 19/Mar/2008).
| Page No. | Comment |
|---|---|
| Throughout | Updated version and date; correction of typographical errors |
| 11 | The text ‘fully informed written (proxy) consent’ moved from T0 to T–4 visit in trial schematic. ‘Verbal consent/assent’ added to T0 visit activities |
| 20–21 | Exclusion criteria corrected to read ‘> 1000micrograms and unlicensed beclometasone dipropionate’ |
| 23 | Clarification of procedures for recruiting via primary care to include opportunistic recruitment |
| 25 | Changed procedure for randomisation – patients are allocated to a treatment arm using a randomisation list rather than through allocation of next sequential randomised treatment pack; pharmacy team are unblinded to treatment allocation |
| 29–31 | Description of trial packaging altered and dispensing procedure updated to reflect this |
| 31 | Clarification that inhaler technique checked throughout trial; first drug shipment size changed from one third to one quarter of total allocation |
| 32 | Accountability procedures updated to reflect randomisation and dispensing procedures |
| 38 | Randomisation procedure updated |
| 38–39 | Expanded details relating to withdrawal of patients from trial treatment |
| 55 | Fluticasone was added to the list of active treatments |
| 62 | The text ‘CTA reference’ replaced by ‘EudraCT number’ |
18.2. Version 3.0 (16/May/2008)
Amendments and Clarifications (v2.0 19/Mar/2008 to v3.0 16/May/2008).
| Page No. | Comment |
|---|---|
| 15 | Clarification of reference from Summary of Product Characteristics |
| 24–25 | Change in pharmacy contact at University Hospital of North Staffordshire (Susan Thomson to Cath Jackson), Royal Aberdeen Children's Hospital (from Valerie Macgregor to Martina Freeman) and the Royal Devon & Exeter (from Kate O'Connor to Fiona Hall). Contact details amended appropriately |
| 31 | Clarification on documentation of patient randomisation number |
| 32 | Long acting beta2 agonists and leukotriene receptor antagonists (other than trial medication) added to list of concomitant medications |
| 35 | Guidance added on the window for timing of patient study visits |
| 68 | The amount available for reimbursement of patient travel expenses was changed from £10 to £8 |
| 475 | Principal investigator at NNUH changed from Professor David Price to Dr Chris Upton |
| 77–78 | South Manchester University Hospital and Wirral Universities Teaching Hospital added as lead participating sites; six GP practices in the Norfolk area added as participating sites (Appendix A) |
| 79–80 | Five participating primary care sites added to Appendix B |
| 81 | T0 pharmacy dispensing procedure for Norfolk patients changed to allow patients to be randomised away from the NNUH |
| 112 | Search codes for GP databases added as an appendix (Appendix E) |
18.3. Version 4.0 (24/Jul/2008)
Amendments and Clarifications (v3.0 16/May/2008 to v4.0 24/Jul/2008)
| Page No. | Comment |
|---|---|
| 21 | Explanation that patients who withdraw early from trial treatment but continue to allow data collection will discuss with the PI whether and when to become unblinded |
| 22 | MCRN CTU to unblind individual patients leaving the trial completely within seven days of completion/withdrawal wherever possible |
| 26 | Addition of pharmacy contact (Neil Caldwell) at Arrowe Park Hospital |
| 29–30 | Change in process of supplying IMP to patients at T–4 and T0 (from IMP being dispensed prior to visit and supplied then if eligible to being dispensed after the visit and then transported to the patient) |
| 34 | CYP3A inhibitors changed from a prohibited concomitant medication group to limited use only whilst on trial treatment |
| 34–36 | Routine unblinding procedure changed from all patients only being unblinded at the end of the trial as a whole to each participant being unblinded when they end their individual participation in the trial. Process for this described (MCRN CTU to inform GP with seven days) |
| 40 | Patients must now be asked for current GP details at the final visit |
| 41 | Clarification that European Respiratory Society (ERS) standards for spirometry will be accepted as well as ATS |
| 45 | Further guidance on completion of the PACQLQ added |
| 62 | Description of new unblinding procedure with regards to study discontinuation |
| 63 | Confirmation that MHRA authorisation has now been granted for MASCOT |
| 65 | Screening logs to be submitted monthly instead of weekly |
| 80–81 | Four GP practices in the Norfolk area added as participating sites (Appendix A) |
| 84–85 | Clarification on process of supplying IMP to Norfolk patients seen at outreach centres – to include change from IMP dispensed prior to the visit to dispensed after the visit and transported to the patient (Appendix C) |
18.4. Version 5.0 (30/Jan/2009)
Amendments and Clarifications (v4.0 24/July/2008 to v5.0 30/Jan/2009)
| Page No. | Comment |
|---|---|
| Throughout | Removal of the word ‘CONFIDENTIAL’ from the page headers |
| 3 | Change in contact details for Aptuit Ltd (from Ciaran Flanagan to Dr Ivan Langan) |
| 5 | Contact details for the MASCOT Data Manager added following the appointment of Emma Dyson |
| 29 | Correction of montelukast matching placebo tablet shelf life from 24 months to fve years |
| 71 | Nemonie Marriott to replace Zahira Maqsood as the primary care representative on the Trial Management Group |
18.5. Version 6.0 (20/May/2009)
Amendments and Clarifications (v5.0 30/Jan/2009 to v6.0 20/May/2009)
| Page No. | Comment |
|---|---|
| Throughout | Updated version and date; correction of typographical errors |
| 3–6 | Correction and updates to contact details of various individuals |
| 10 | Update in number of secondary care centres from 12 to 13 |
| 14–16 | Updates to ‘Potential Risks’ section for all three study medications (information derived from SPCs) |
| 18 | Addition of ‘Adverse Events’ as a secondary endpoint |
| 19 | Clarification of inclusion criteria #1 at both T–4 and T0 (from ‘Those requiring frequent short-acting beta2 agonist relief therapy ≥ 7 puffs per week’ to ‘Those requiring frequent short-acting beta2 agonist relief therapy ≥ 7 puffs in the past seven days’ |
| 21–22 | Additions to recruitment section including recruitment via community pharmacists and school health professionals and promotion via the media. Expansion of existing strategies to include use of a follow-up letter or telephone call and recruitment via any appropriate primary care centre |
| 23 | Update to site name (from ‘Royal Liverpool Children's Hospital’ to ‘Alder Hey Children's NHS Foundation Trust’) |
| 23 | Change in pharmacist at Royal Manchester Children's Hospital (from Judith Thornton to Carolyn Davies) and Derbyshire Children's Hospital (from Julie Vanes and Liz Bedford to Peter Fox) and updates to associated contact details |
| 27 | Clarification added that pharmacists must complete all sections on the trial medication labels prior to dispensing |
| 32 | Revision of text to show that unblinding information at completion of/withdrawal from trial treatment will be provided to the patient's GP only. Secondary care clinicians will now be instructed to contact the GP if they require this information |
| 34–35 | Addition of caveat that the RN/PI can conduct the T+8 and T+24 study visits at the patient's home, instead of clinic, in exceptional circumstances |
| 41–43 | Updates to sample size calculation formula and justifications (sample size remains unchanged) |
| 43 | Change in planned interim sample size review – now to be conducted after the first 75 children have completed 24 week follow-up |
| 44–45 | Various updates and Clarifications to the statistical analysis plan. Discussion of how secondary outcomes will be analysed |
| 58–59 | Revision of the text detailing how data queries will be documented and resolved. All data queries will be actioned using specific Data Query Forms, no changes will be made to the original CRF page/s |
| 62 | Change as to who the £25.00 participant identification payment can be made to – this now includes any appropriate healthcare provider, not just GP practices |
| 67 | Removal of the Machin et al. (1997) reference. Addition of Metcalfe et al. (2003) reference |
| 74 | Removal of Appendix B which listed ‘Satellite’ GP centres in the Greater London area affiliated to the Royal London Hospital. These are now referenced in Section 8.1 |
| 77 | Removal of Appendix D, Summary of Product Characteristics – now to be provided to sites separate from the protocol |
| 105 | Appendix E (now Appendix C) – updates to the GP Database Search Guidance |
19. REFERENCES
- 1.
- Srivastava P, Baird A, Mill A et al. Risk factors for wheeze in transition from childhood to early adulthood. Am J Resp Crit Care Med 2000;161:A917.
- 2.
- SIGN, British Guideline on the Management of Asthma. Thorax 2003;58:i1–i94. [PMC free article: PMC1766014] [PubMed: 12653493]
- 3.
- Van den Berg NJ, Ossip MS, Hederos CA et al. Salmeterol/fluticasone propionate in combination is effective and safe in children with asthma. Pediatr Pulmonol 2000;30:97–105. [PubMed: 10922131]
- 4.
- Knorr B, Matz J, Bernstein JA et al. Montelukast for chronic asthma in 6–14 year old children. JAMA 1998;279:1181–6. [PubMed: 9555757]
- 5.
- Verberne AA, Frost C, Duiverman EJ et al. (1998) Addition of salbutamol versus doubling the dose of beclomethasone in children with asthma. Am J Respir Crit Care Med 1998;158:213–19. [PubMed: 9655732]
- 6.
- Greening AP, Ind PW, Northfield M et al. Added salmeterol versus higher-dose corticosteroid in asthma patients with symptoms on existing inhaled corticosteroid. Lancet 1994;344:219–24. [PubMed: 7913155]
- 7.
- Garrett J, Williams S, Wong C et al. Treatment of acute asthma exacerbations with an increased dose of inhaled steroid. Arch Dis Child 1998;79:12–17. [PMC free article: PMC1717626] [PubMed: 9771245]
- 8.
- Personal communication – Prof Hans Bisgaard – during development of paediatric asthma studies.
- 9.
- Allen D, Mullen M, Mullen B (1994). A meta-analysis of the effect of oral and inhaled corticosteroids on growth. JACI 1994;93:967–76. [PubMed: 8006318]
- 10.
- Russell G. Inhaled corticosteroids and adrenal insufficiency. Arch Dis Child 2002;87:455–6. [PMC free article: PMC1755856] [PubMed: 12456537]
- 11.
- Crowley S. Inhaled glucocorticoids and adrenal function: an update. Paediatr Resp Rev 2003;4:153–61. [PubMed: 12758054]
- 12.
- Committee on Safety of Medicines and Medicines Control Agency. Current problems in pharmacovigilance. Drugs and Therapeutics Bulletin 2002;28:7.
- 13.
- Juniper EF, O'Byrne PM, Guyatt GH et al. Development and validation of a questionnaire to measure asthma control. Eur Respir J 1999;14:902–7. [PubMed: 10573240]
- 14.
- Newacheck PW, Halfon N. Prevalence, impact, and trends in childhood disability due to asthma. Arch Pediatr Adolesc Med 2000;154:287–93. [PubMed: 10710030]
- 15.
- Begg C, Cho M, Eastwood S, Horton R, Moher D, Olkin I, et al. Improving the quality of reporting of randomized controlled trials. The CONSORT statement. JAMA 1996;276:637–9. [PubMed: 8773637]
- 16.
- Moher D, Schulz KF, Altman D. for the CONSORT group. The CONSORT Statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. Lancet 357:1191–4. [PubMed: 11323066]
- 17.
- Metcalfe C, Thompson SG, Cowie MR, Sharples LD. The use of hospital admission data as a measure of outcome in clinical studies of heart failure. European Heart Journal 2003;24:105–112. [PubMed: 12559942]
20. APPENDICES
Appendix A. Lead Participating Sites
| Participating Site: | Professor Warren Lenney |
| Consultant Paediatrician/Professor of Paediatrics | |
| Medical Research Unit | |
| University Hospital of North Staffordshire | |
| Hartshill Road | |
| Hartshill | |
| Stoke on Trent | |
| ST4 7QB | |
| Tel: 01782 554610 | |
| Fax: 01782 412236 | |
| Email: ku.shn.snhu@yennel.nerraw | |
| Participating Site: | Dr Chris Upton |
| Consultant Paediatrician | |
| Norfolk & Norwich University Hospital | |
| Colney Lane | |
| Norwich | |
| NR4 7UY | |
| Tel: 01603 287544 | |
| Fax: 01603 286318 | |
| Email: ku.shn.hunn@notpu.sirhc | |
| Participating Site: | Dr Stephen Turner |
| Consultant Paediatrician & Clinical Senior Lecturer | |
| Royal Aberdeen Children's Hospital | |
| Westburn Road | |
| Foresterhill | |
| Aberdeen | |
| AB25 2ZG | |
| Tel: 01224 555195 | |
| Fax: 01224 551919 | |
| Email: ku.ca.ndba@renrut.w.s | |
| Participating Site: | Dr Hitesh Pandya |
| Senior Lecturer & Honorary Consultant Paediatrician | |
| Robert Kilpatrick Clinical Sciences Building | |
| Leicester Royal Infirmary | |
| Infirmary Square | |
| Leicester | |
| LE2 7LX | |
| Tel: 0116 258 5881 | |
| Fax: 0116 252 3282 | |
| Email: ku.ca.el@82ph | |
| Participating Site: | Dr Tom Hilliard |
| Consultant Paediatrician | |
| Bristol Royal Hospital for Children | |
| Upper Maudlin Street | |
| Bristol | |
| BS2 8BJ | |
| Tel: 0117 342 8693 | |
| Fax: 0117 342 8494 | |
| Email: ku.shn.thbu@draillih.mot | |
| Participating Site: | Dr Will Carroll |
| Consultant Paediatrician | |
| Derbyshire Children's Hospital | |
| Uttoxeter Road | |
| Derby | |
| DE22 3NE | |
| Tel: 01332 786826 | |
| Fax: 01332 200857 | |
| Email: ten.shn@llorrac.lliw | |
| Participating Site: | Dr Andrew Collinson |
| Consultant Paediatrician | |
| Royal Devon & Exeter NHS Foundation Trust | |
| Barrack Road | |
| Exeter | |
| EX2 5DW | |
| Tel: 01392 403694 | |
| Fax: 01392 406435 | |
| Email: ku.shn.tfedr@nosnilloC.werdnA | |
| Participating Site: | Dr Edward Simmonds |
| Consultant Paediatrician | |
| University Hospitals of Coventry & Warwickshire NHS Trust | |
| Clifford Bridge Road | |
| Coventry | |
| CV2 2DX | |
| Tel: 02476 96 7232 | |
| Fax: 02476 967248 | |
| Email: ku.shn.wchu@sdnommis.drawde | |
| Participating Site: | Dr Clare Murray |
| Consultant Respiratory Paediatrician & Clinical Senior Lecturer | |
| Royal Manchester Children's Hospital | |
| Hospital Road | |
| Pendlebury | |
| Manchester | |
| M27 4HA | |
| Tel: 0161 922 2191 | |
| Fax: 0161 922 2191 | |
| E-mail: ku.shn.cmmc@yarrum.eralc | |
| Participating Site: | Dr Jonathan Couriel |
| Consultant Respiratory Paediatrician | |
| Alder Hey Children's NHS Foundation Trust | |
| Eaton Road | |
| West Derby | |
| Liverpool | |
| L12 2AP | |
| Tel: 0151 252 5911 | |
| Fax: 0151 252 5929 | |
| Email: ku.shn.yehredla@leiruocj | |
| Participating Site: | Prof Harish Vyas |
| Consultant in PICU and Respiratory Medicine | |
| Queens Medical Centre Campus | |
| Nottingham University Hospital | |
| Derby Road | |
| Nottingham | |
| NG7 2UH | |
| Tel: 0115 9249924 (ext 64841) | |
| Fax: 0115 9420324 | |
| Email: ku.shn.hun@sayv.hsirah | |
| Participating Site: | Dr Caroline Pao |
| Consultant Paediatrician Respiratory and General Paediatrics | |
| Royal London Hospital | |
| Bart's & The London NHS Trust | |
| Whitechapel | |
| London | |
| E1 1BB | |
| Tel: 020 7733 7000 (ext. 3931) | |
| Fax: | |
| E-mail: ku.shn.nodnolehtdnastrab@oaP.eniloraC | |
| Participating Site: | Dr Clare Murray |
| Consultant Respiratory Paediatrician & Clinical Senior Lecturer | |
| University Hospital of South Manchester | |
| Southmoor Road | |
| Wythenshawe | |
| Manchester | |
| M23 9LT | |
| Tel: 0161 291 5876 | |
| Fax: 0161 291 5730 | |
| E-mail: ku.ca.retsehcnam@yarrum.eralc | |
| Participating Site: | Dr David Lacy |
| Consultant Paediatrician | |
| Wirral Universities Teaching Hospital NHS Foundation Trust | |
| Arrowe Park Hospital | |
| Arrowe Park Road | |
| Upton | |
| Wirral | |
| CH49 5PE | |
| Tel: 0151 604 7498 | |
| Fax: 0151 604 7206 | |
| Email: ku.shn.tnhw@ycaL.divaD | |
| Participating Site: | Dr Hywel Jones |
| General Practitioner | |
| The Surgery | |
| 15 Dereham Road | |
| Mattishal | |
| Dereham | |
| NR20 3QA | |
| Tel: 01362 850227 | |
| Fax:01362 858466 | |
| Email: ten.shn@senoj.lewyh | |
| Participating Site: | Dr Rob Stone |
| General Practitioner | |
| Hellesdon Medical Practice | |
| 343 Reepham Road | |
| Hellesdon | |
| Norwich | |
| NR6 5QJ | |
| Tel: 01603 486602 | |
| Fax:01 603 401389 | |
| Email: ten.shn@enots.bor | |
| Participating Site: | Dr Stephen Thurston |
| General Practitioner | |
| Wymondham Postmill Close | |
| Wymondham | |
| Norfolk | |
| NR18 0RF | |
| Tel: 01953 602118 | |
| Fax: 01953 605313 | |
| Email: ten.shn@notsruht.nehpets | |
| Participating Site: | Dr Peter Franklin |
| General Practitioner | |
| Holt Medical Practice | |
| Kelling Hospital | |
| Old Cromer Road | |
| High Kelling | |
| Holt | |
| NR25 6QA | |
| Tel:01 263 712461 | |
| Fax: 01263 713211 | |
| Email: ten.shn@nilknarf.retep | |
| Participating Site: | Dr Alasdair Duthie |
| General Practitioner | |
| The Surgery | |
| Church Plain | |
| Loddon | |
| Norfolk | |
| NR14 6EX | |
| Tel: 01508 520222 | |
| Fax: 01508 528579 | |
| Email: ten.shn@eihtud.riadsala | |
| Participating Site: | Dr Simon May |
| General Practitioner | |
| The Surgery | |
| Overstrand Road | |
| Cromer | |
| Norfolk | |
| NR27 0AJ | |
| Tel:01263 513148 | |
| Fax:01 263 515264 | |
| Email: ten.shn@yam.nomis | |
| Participating Site: | Dr Alistair Martin |
| General Practitioner | |
| Attleborough Surgery | |
| Station Road | |
| Attleborough | |
| Norfolk | |
| NR17 2AS | |
| Tel: 01953 452394 | |
| Fax: 01953 xxxx | |
| Email: ten.shn@nitram.riatsila | |
| Participating Site: | Dr Carsten Dernedde |
| General Practitioner | |
| Hoveton & Wroxham Medical Practice | |
| Stalham Road | |
| Hoveton | |
| Norfolk | |
| NR12 8DU | |
| Tel: 01603 782155 | |
| Fax: 01603 xxxx | |
| Email: ten.shn@eddenred.netsrac | |
| Participating Site: | Dr Kevin Elsby |
| General Practitioner | |
| The Market Surgery | |
| 26 Norwich Road | |
| Aylsham | |
| Norfolk | |
| NR11 6BW | |
| Tel: 01263 733331 | |
| Fax: 01263 xxxx | |
| Email: ten.shn@ybsle.niveK | |
| Participating Site: | Dr Sanjay Gheyi |
| General Practitioner | |
| Coltishall Medical Practice | |
| St Johns Close | |
| Rectory Road | |
| Coltishall | |
| Norfolk | |
| NR12 7HL | |
| Tel: 01603 737593 | |
| Fax: 01603 xxxx | |
| Email: ten.shn@iyehg.s |
Appendix B. Pharmacy Dispensing Procedure for Norfolk & Norwich University Hospital
Trial medications for all Norfolk participants, including those seen at the ten General Practitioners sites, will be stored at and dispensed from the pharmacy department at the Norfolk & Norwich University Hospital (NNUH). Trial medications will be dispensed from pharmacy at the NNUH using the following procedures:
T–4
Where the T-4 visit is conducted at an outreach centre (i.e. a GP practice), if the patient is registered in the trial the PI will write the T-4 prescription for that patient. The RN/PI will arrange with the patient to collect the study medication from the outreach centre on a day agreed with both the patient and the dispensing pharmacy department. On receipt of the prescription, pharmacy will prepare the medication for dispensing. It will be placed in a container with a temperature monitor provided centrally through the MASCOT trial. The medication will be transported via the hospital pharmacy service which delivers hospital dispensed prescriptions to GP practices within the community. Two members of the NNUH pharmacy team will sign and date the accountability log to confirm that the prescription has been dispensed. The medication will be securely transported to the outreach clinic where the patient will collect their study medication.
T0
Where the T0 visit is conducted at an outreach centre (i.e. a GP practice), if the patient is found to be eligible for randomisation and wishes to continue in the trial, the PI will write a trial prescription which will be faxed to pharmacy. The RN/PI will arrange with the patient to collect the study medication from the outreach centre on a day agreed with both the patient and the dispensing pharmacy department. The patient will be allocated their randomisation number by pharmacy as per the standard process detailed in Section 7 and an appropriate treatment pack will be prepared for dispensing. It will be placed in a container with a temperature monitor provided centrally through the MASCOT trial. The medication will be transported via the hospital pharmacy service which delivers hospital dispensed prescriptions to GP practices within the community. Two members of the NNUH pharmacy team will sign and date the accountability log to confirm that the prescription has been dispensed. The medication will be securely transported to the outreach clinic where the patient will collect their medication.
T+8 onwards
The PI/RN will ensure that pharmacy have received a signed valid prescription at least 48 hours before the medication needs to be dispensed. On receipt of the prescription, pharmacy will ascertain the patient's randomised treatment allocation and dispense the appropriate trial treatment pack/s for that patient. The pack/s will be placed in a container with a temperature monitor provided centrally through the MASCOT trial. The medication will be transported via the hospital pharmacy service which delivers hospital dispensed prescriptions to GP practices within the community. Two members of the NNUH pharmacy team will sign and date the accountability log to confirm that the prescription has been dispensed. The medication will be securely transported to the outreach clinic where the patient will be attending for their study visit that day. The medication will then be given to the patient by the RN at the end of the visit if they are eligible and willing to continue to the next part of the study. If the patient is not eligible to continue in the trial or wishes to withdraw from trial treatment at that point, the dispensed medications will be returned to pharmacy for destruction. The RN will collect any previously dispensed used/unused medications from the patient and return them to the hospital pharmacy within five working days for destruction.
Appendix C. GP Database Search Guidance
As per ‘Recruitment Strategies – Primary Care #1 and #2’ (Section 6.1), General Practitioners' databases may be searched in order to identify potentially eligible patients for the study. Below are a set of guidelines for facilitating the electronic searches. However, this is not an exhaustive guide and should be adapted to fit the database systems and procedures in use by the individual practice.
ELIGIBILITY CRITERIA SEARCH
1. Age range – 6–14 yrs 11/12 months (SHARED) – shared by all in total group (not incl or excl)
2. Asthma (H33) Any code (incls past/active)
OR children on bronchodilators and/or shorting acting corticosteroids.
No date range incl (SHARED)
3. Bronchodilaters – current prescriptions.
Try 1 script (issue) in last year (SHARED)
4*. Not eligible (exclusion) if prescribed in the previous month and used currently Leukotriene Antagonists
Select drugs: Montelukast Zafilucast/Accolate
Issue (script) 1 in the last month
(EXCLUSION)
5*. Exclusion not shared
Exclude long acting beta agonists (select beta agonist) if prescribed in the last previous month and used currently
Select drugs: Formoteral/fumerate
Seretride (combination flixotide+) Symbicort
Current: 1 script (issue) in the last month
(EXCLUSION)
6. Not shared
Exclude theophyline
Current last year
7. EXCLUSION
Cystic Fibrosis (CF) – C370
Cardiac congenital P6
Exclude P68 congenital heart disease
*Please note that this criterion can be added on as an excluder when conducting the electronic search. However, depending on the time coding methods and the individual database, it may be easier to assess this during a manual notes search after the initial electronic search has been conducted to avoid any potentially eligible patients being prematurely excluded.
TO CREATE A SEARCH ON EMIS LV
Choose ST search & statistics
Select B – patient searches
Select A – build and perform a new search
Select A – search on today's practice population i.e. currently registered pop (SHARED)
Select A – add Feature
Select 2 – AGE upper 14, lower 6 (SHARED)
Select 2 – Classification Codes, type Read Code H33,
Select A – (Asthma**) press return (answer Y to all lower codes)
Select A – no date range, A (SHARED)
Select A – add Feature
Select 7 – Drugs, when prompted ‘Search on all drugs Y/N’ enter N for No
Select B – search by drug group
Select 3 – Respiratory System Drugs
Select 3 – (corticosteroids for inhalation), press return (Y for all variants of drug group)
Press return (C current), press (A – all)
Enter date range 01/01/2008, press return, (today's date)
Press return (blank frequency)
Enter Y to continue, set operator as (SHARED)
NOW ADD IN CRITERIA FOR DRUG EXCLUSIONS
Select A – add Feature
Select 7 – Drugs, when prompted ‘Search on all drugs Y/N’ enter N for No
Select I – Ingredient or brand, type in part of the name of the drug e.g. ‘Monte’ press return
Select 1 – (montelukart sodium (G) (T)) press return, Enter – (Y to all variants), press return
Enter – (C – current) press return
Enter – (A – all)
Enter date range – (6 months ago), press return, (today's date)
Press return (blank frequency)
Enter Y to continue, set operator as B (EXCLUDE)
Select A – add Feature
Select 7 – Drugs, when prompted ‘Search on all drugs Y/N’ enter N for No
Select I – Ingredient or brand, type in part of the name of the drug e.g. ‘Salmet’ press return
Select 1 – (salmeterol xinafoate (G) (T)) press return, Enter – (Y to all variants), press return
Enter – (C – current) press return
Enter – (A – all)
Enter date range – (6 months ago), press return, (today's date)
Press return (blank frequency)
Enter Y to continue, set operator as B (EXCLUDE)
Select A – add Feature
Select 7 – drugs, when prompted ‘Search on all drugs Y/N’ enter N for No
Select I – Ingredient or brand, type in part of the name of the drug e.g. ‘Formo’ press return
Select 3 – (Formoterol Fumarate (G) (T)) press return, Enter – (Y to all variants), press return
Enter – (C – current) press return
Enter – (A – all)
Enter date range – (6 months ago), press return, (today's date)
Press return (blank frequency)
Enter Y to continue, set operator as B (EXCLUDE)
When you have entered the appropriate criteria enter Y to confirm that the features are correct (N if they are not and edit the search) always check your date range & operator status.
Save the search with an appropriate name, prefixed by ‘MASCOT’, to the directory for one off searches. Enter Y to run the search. A message in a yellow band will appear at the top of the screen when the search has completed.
To view the results go to S ‘Search results’, type MASCOT and press return. Select your search
Choose A – A table showing the distribution by age and sex.
Once you are happy with the group of patients the search has generated, via WP Word Processing module mail merge the MASCOT participant invitation letter template onto practice letter headed paper, including the patient's name & address details.
The envelope to be mailed out to the patient and their family should include:
- the participant invitation letter
- parent/guardian MASCOT Patient Information Sheet
- the age-specific MASCOT Patient information Sheet (optional)
- a stamped SAE for use when returning the reply slip to the local MASCOT team
REMEMBER – only appropriate practice staff can view identifiable patient data. MASCOT research nurses should not be accessing patient names or any data which could easily identify a patient.
- General Information
- Statement of Compliance
- Contact Details: Institutions
- Contact Details: Individuals
- Contact Details: Independent Oversight Committees
- List of abbreviations
- PROTOCOL SUMMARY
- BACKGROUND INFORMATION
- SELECTION OF CENTRES/CLINICIANS
- ENDPOINTS
- STUDY POPULATION
- RECRUITMENT, REGISTRATION AND RANDOMISATION
- TRIAL TREATMENT/S
- ASSESSMENTS AND PROCEDURES
- STATISTICAL CONSIDERATIONS
- PHARMACOVIGILANCE
- ETHICAL CONSIDERATIONS
- REGULATORY APPROVAL
- TRIAL MONITORING
- INDEMNITY
- FINANCIAL ARRANGEMENTS
- TRIAL COMMITTEES
- PUBLICATION
- PROTOCOL AMENDMENTS
- REFERENCES
- APPENDICES
- Protocol - Management of Asthma in School age Children On Therapy (MASCOT): a ra...Protocol - Management of Asthma in School age Children On Therapy (MASCOT): a randomised, double-blind, placebo-controlled, parallel study of efficacy and safety
- NPHP3 nephrocystin 3 [Homo sapiens]NPHP3 nephrocystin 3 [Homo sapiens]Gene ID:27031Gene
Your browsing activity is empty.
Activity recording is turned off.
See more...