NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
NHLBI Obesity Education Initiative Expert Panel on the Identification, Evaluation, and Treatment of Obesity in Adults (US). Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. Bethesda (MD): National Heart, Lung, and Blood Institute; 1998 Sep.
A. Overview
The presence of overweight and obesity in a patient is of medical concern because it increases the risk for several diseases, particularly cardiovascular diseases (CVDs) and diabetes mellitus (see Chapter 2.C.) and it increases all-cause mortality. Treatment of the overweight and obese patient is a two-step process: assessment and management. Assessment requires determination of the degree of obesity and absolute risk status. Management includes both weight control or reducing excess body weight and maintaining that weight loss as well as instituting other measures to control associated risk factors. The aim of this guideline is to provide useful advice on how to achieve weight reduction and maintenance of a lower body weight. Obesity is a chronic disease, and both the patient and the practitioner need to understand that successful treatment requires a life-long effort.
B. Assessment and Classification of Overweight and Obesity
1. Assessment of Overweight and Obesity
- Determination of total body fat. Overweight is defined as a body mass index (BMI) of 25 to 29.9 kg/m2. Obesity is defined as an excess of total body fat that is documented by a BMI of ≥30 kg/m2. Several methods are available for determining or calculating total body fat: total body water, total body potassium, bioelectrical impedance, and dual-energy X-ray absorptiometry.
Evidence Statement
Measures of body fat give reasonably equivalent values for following overweight or obese patients during treatment. Evidence Category D.
Rationale: Even though accurate methods to assess body fat exist, measuring body fat content by these techniques is often expensive and is not readily available clinically. Although bioelectrical impedance devices are becoming more readily available, they lose accuracy in severely obese persons and are of limited usefulness for tracking changes in total body fat in persons losing weight. Thus, bioelectrical impedance offers no significant advantage over BMI in the clinical management of patients. No trial data exist to indicate that one measure of fatness is better than any other for following overweight and obese patients during treatment. No studies have been published to compare the effectiveness of different measures for evaluating changes in body fat during weight reduction. BMI provides a more accurate measure of total body fat than relying on weight alone. It has an advantage over percent above ideal weight (e.g., based on the Metropolitan Life Insurance Tables). Ideal body weight tables were developed primarily from white, higher socioeconomic status populations and have not been documented to accurately reflect body fat content in the public at large. In addition, separate tables are required for men and women. The weight tables also are based on mortality outcomes and do not necessarily predict morbidity. BMI is recommended as a practical approach for the clinical setting. BMI provides an acceptable approximation for assessment of total body fat for the majority of patients [525–527]. However, simply measuring body weight is a practical approach to follow weight changes.
RECOMMENDATION
Practitioners should use the BMI to assess overweight and obesity. Body weight alone can be used to follow weight loss and to determine efficacy of therapy. Evidence Category C.
Rationale: The panel concentrated on tools available in the office, i.e., weight, height and the BMI. BMI is a practical indicator of the severity of obesity, and it can be calculated from existing tables. BMI is a direct calculation based on height and weight, regardless of gender. The limitations of BMI as a measure of total body fat, nonetheless, must be recognized. For example, BMI overestimates body fat in persons who are very muscular and can underestimate body fat in persons who have lost muscle mass (e.g., the elderly).
The BMI is calculated as follows:
BMI = weight (kg)/height squared (m2)
To estimate BMI from pounds and inches use:
[weight (pounds)/ height (inches)2] × 703 [528]
(1 lb = 0.4536 kg)
(1 in = 2.54 cm = 0.0254 m)
A simple BMI chart is provided in Appendix V. A patient should be weighed with shoes off and clad only in a light robe or undergarments.
- Determination of degree of abdominal obesity. The presence of excess fat in the abdomen, out of proportion to total body fat, is an independent predictor of risk factors and morbidity. Relatively accurate measures of total abdominal fat can be made by magnetic resonance imaging [529] or computed tomography [500, 530]. These methods, however, are expensive and not readily available for clinical practice. Research with these techniques, nonetheless, has shown that the waist circumference correlates with the amount of fat in the abdomen, and thus is an indicator of the severity of abdominal obesity. In this document the term “waist” circumference is used instead of “abdominal” circumference because it more accurately describes the anatomical site of measurement.
Evidence Statement
Waist circumference is the most practical anthropometric measurement for assessing a patient's abdominal fat content before and during weight loss treatment. Computed tomography and magnetic resonance imaging are both more accurate but are impractical for routine clinical use. Evidence Category C.
Rationale: Fat located in the abdominal region is associated with greater health risks than that in peripheral regions, e.g., the gluteal-femoral area [155–159, 429, 430]. Abdominal fat is described as having three compartments: visceral, retroperitoneal, and subcutaneous [529, 531, 532]. Several studies suggest that the visceral fat component of abdominal fat is the most strongly correlated with risk factors; [160, 161, 533, 534] other studies, however, indicate that the subcutaneous component is the most highly correlated with insulin resistance [529, 535, 536]. Therefore, the relative contributions of different components of abdominal fat to overall risk remain to be determined with certainty. Nonetheless, the presence of increased total abdominal fat appears to be an independent risk predictor when the BMI is not markedly increased [537]. Therefore, waist or abdominal circumference, as well as BMI, should be measured not only for the initial assessment of obesity, but also as a guide to the efficacy of weight loss treatment.
The waist-to-hip ratio (WHR) also has been used in a number of epidemiologic studies to show increased risk for diabetes, coronary artery disease, and hypertension [500]. However, waist circumference has been found to be a better marker of abdominal fat content than is WHR [85]. Whether WHR imparts any independent information about disease risk beyond waist circumference is uncertain, but between the two, the waist circumference appears to carry greater prognostic significance. Therefore, in clinical practice, abdominal fat content should be assessed and followed by measuring waist circumference.
RECOMMENDATION
The waist circumference should be used to assess abdominal fat content. Evidence Category C.
2. Classification of Overweight and Obesity
- According to BMI. The primary classification of obesity is based on the measurement of BMI. This classification is designed to relate BMI to risk of disease. It should be noted that the relation between BMI and disease risk varies among individuals and among different populations. Therefore, the classification must be viewed as a broad generalization. Individuals who are very muscular may have a BMI placing them in an overweight category when they are not overly fat. Also, very short persons (under 5 feet) may have high BMIs that may not reflect overweight or fatness. In addition, susceptibility to risk factors at a given weight varies among individuals. Some individuals may have multiple risk factors with mild obesity, whereas others may have fewer risk factors with more severe obesity. It should also be noted that the risk levels shown for each increment in risk are relative risks; that is, relative to risk at normal weight. They should not be equated with absolute risk which is determined by a summation of risk factors. No randomized controlled trial studies exist that support a specific system for classification that establishes the degree of disease risk for patients during weight loss or weight maintenance. The classification is based on observational and prospective epidemiological studies.
Instructions for Measuring Waist Circumference, According to NHANES III Protocol
To define the level at which waist circumference is measured, a bony landmark is first located and marked. The subject stands and the examiner, positioned at the right of the subject, palpates the upper hip bone to locate the right iliac crest. Just above the uppermost lateral border of the right iliac crest, a horizontal mark is drawn, then crossed with a vertical mark on the midaxillary line. The measuring tape is placed in a horizontal plane around the abdomen at the level of this marked point on the right side of the trunk. The plane of the tape is parallel to the floor and the tape is snug, but does not compress the skin. The measurement is made at a normal minimal respiration (see Figure 5).
REF: U.S. Department of Health and Human Services, PHS. NHANES III Anthropometric Procedures Video. U.S. Government Printing Office Stock Number 017-022-01335-5. Washington, D.C.: U.S. GPO, Public Health Service; 1996 [538].
RECOMMENDATION
The BMI * should be used to classify overweight and obesity and to estimate relative risk for disease compared to normal weight. Evidence Category C.
Pregnant women who, on the basis of their prepregnant weight, would be classified as obese may encounter certain obstetrical risks. However, the inappropriateness of weight reduction during pregnancy is well recognized [44]. Hence, this guideline specifically excludes pregnant women.
Rationale: Overweight and obesity are classified by BMI (see Table IV-1).
Calculating BMI is simple, rapid, and inexpensive. The classification can be applied generally to adults. See Appendix III for comments about obesity and its classification in children. The basis for this BMI classification scheme stems from observational and epidemiologic studies which relate BMI to risk of morbidity and mortality [11, 81–83, 131, 155, 278, 539–541]. For example, relative risk for CVD increases in a graded fashion with increasing BMI in all population groups, although absolute risk in obese versus nonobese persons depends on the summed contribution of all risk factors.
Evidence Statement
The same BMI cutpoints (see Table IV-1) can be used to classify the level of overweight and obesity for adult men and adult nonpregnant women, and generally for all racial/ethnic groups. Evidence Category C.
Rationale: Clinical judgment must be used in interpreting BMI in situations in which it may not be an accurate indicator of total body fat. Examples are the presence of edema, high muscularity, muscle wasting, or for very short people. The relationship between BMI and body fat content varies somewhat with age, sex, and possibly ethnicity because of differences in factors such as composition of lean tissue, sitting height, and hydration state [526, 542]. For example, older persons often have lost muscle mass and have more fat for a given BMI than younger persons, women may have more fat for a given BMI than men, and persons with clinical edema may have less fat for a given BMI than persons without edema. Nevertheless, these differences generally do not markedly influence the validity of BMI cutpoints either for classifying individuals into broad categories of overweight and obesity or for monitoring weight status of individuals in clinical settings [526].
- According to waist circumference. Although waist circumference and BMI are interrelated, waist circumference provides an independent prediction of risk over and above that of BMI. Waist circumference measurement is particularly useful in patients who are categorized as normal or overweight on the BMI scale. At BMIs ≥ 35, waist circumference has little added predictive power of disease risk beyond that of BMI. It is therefore not necessary to measure waist circumference in individuals with BMIs ≥ 35.
Evidence Statement
Sex-specific cutoffs for waist circumference can be used to identify increased risk associated with abdominal fat in adults with a BMI in the range of 25 to 34.9 kg/m2. An increase in waist circumference may also be associated with increased risk in persons of normal weight. Evidence Category C.
Waist circumference cutpoints can generally be applied to all adult ethnic or racial groups. On the other hand, if a patient is very short (under 5 feet) or has a BMI above the 25 to 34.9 kg/m2 range, waist cutpoints used for the general population may not be applicable. Evidence Category D.
Rationale: A high waist circumference is associated with an increased risk for type 2 diabetes, dyslipidemia, hypertension, and CVD in patients with a BMI in a range between 25 and 34.9 kg/m.2 82 Monitoring changes in waist circumference over time may be helpful, in addition to measuring BMI, since it can provide an estimate of increased abdominal fat even in the absence of a change in BMI. Furthermore, in obese patients with metabolic complications, changes in waist circumference are useful predictors of changes in CVD risk factors [537]. The waist circumference at which there is an increased relative risk is defined as follows:
High Risk
Men > 102 cm ( > 40 in)
Women > 88 cm ( > 35 in)
To evaluate health risks, it is not necessary to measure waist circumference in patients with a BMI ≥ 35 kg/m2; the measurement usually will be greater than the cutpoints given above, and waist measurements lose their predictive power at very high BMIs.
There are ethnic and age-related differences in body fat distribution that modify the predictive validity of waist circumference as a surrogate for abdominal fat [526]. These variations may partly explain differences between ethnic or age groups in the power of waist circumference or WHR to predict disease risks [429, 543].
In some populations, waist circumference is a better indicator of relative disease risk than is BMI; examples include Asian-Americans or persons of Asian descent living elsewhere [51, 273, 544]. Waist circumference also assumes greater value for estimating risk for obesity-related disease at older ages. Table IV-2 incorporates both BMI and waist circumference in the classification of overweight and obesity, and provides an indication of disease risk.
RECOMMENDATION
For adult patients with a BMI of 25 to 34.9 kg/m2, sex-specific waist circumference cutoffs should be used in conjunction with BMI to identify increased disease risk. Evidence Category C.
C. Assessment of Risk Status
The patient's risk status should be assessed by determining the degree of overweight or obesity based on BMI, the presence of abdominal obesity based on waist circumference, and the presence of concomitant CVD risk factors or comorbidities. Some obesity-associated diseases and risk factors place patients in a very high risk category for subsequent mortality. These diseases will require aggressive modification of risk factors in addition to their own clinical management. Other obesity-associated diseases are less lethal, but still require appropriate clinical therapy. Obesity also has an aggravating influence on several cardiovascular risk factors. Identifying these risk factors is required as a guide to the intensity of clinical intervention.
1. Determination of relative risk status based on overweight and obesity parameters
Table IV-2 defines relative risk categories according to BMI and waist circumference. It is important to note that these categories denote relative risk, not absolute risk. They relate to the need to institute weight loss therapy, and do not directly define the required intensity of risk factor modification. The latter is determined by estimation of absolute risk based on the presence of associated disease or risk factors.
2. Identification of patients at very high absolute risk
The following disease conditions or target organ damage in hypertensive patients denote the presence of very high absolute risk that triggers the need for intense risk factor modification as well as disease management. For example, the presence of very high absolute risk indicates the need for aggressive cholesterol-lowering therapy [142].
2.a. Established coronary heart disease (CHD)
2.a.1. History of myocardial infarction
2.a.2. History of angina pectoris (stable or unstable)
2.a.3. History of coronary artery surgery
2.a.4. History of coronary artery procedures (angioplasty)
2.b. Presence of other atherosclerotic diseases
2.b.1. Peripheral arterial disease
2.b.2. Abdominal aortic aneurysm
2.b.3. Symptomatic carotid artery disease
2.c. Type 2 diabetes
2.d. Sleep apnea (For more information, see Appendix IV.)
3. Identification of other obesity-associated diseases
Obese patients are at increased risk for several conditions that require detection and appropriate management, but that generally do not lead to widespread or life-threatening consequences. These include:
3.a. Gynecological abnormalities
3.b. Osteoarthritis
3.c. Gallstones and their complications
3.d. Stress incontinence
Management options of risk factors for preventing CVD, diabetes mellitus, and other chronic diseases are described in detail in other reports. For details on the management of serum cholesterol and other lipoprotein disorders, refer to the National Cholesterol Education Program's Second Report of the Expert Panel on the Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel II/ATP II) (1993) [142]. For the treatment of hypertension, the National High Blood Pressure Education Program recently issued the Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VI) (1997) [545]. For the most recent recommendations about type 2 diabetes from the American Diabetes Association, see the ADA Clinical Practice Recommendations (1998) [546]. Finally, smoking cessation is strongly recommended in obese smokers, with particular attention to methods that diminish the weight gain associated with cessation (see pages 91–92). For strategies and recommendations for supporting and delivering effective smoking cessation intervention, see the Agency for Health Care Policy and Research's Clinical Practice Guidelines on Smoking Cessation [547].
Although obese patients are at increased risk for gallstones, this risk increases even more during periods of rapid weight reduction.
4. Identification of cardiovascular risk factors that impart a high absolute risk
Patients can be classified as being at high absolute risk for obesity-related disorders if they have three or more of the multiple risk factors listed below. The presence of high absolute risk increases the intensity of cholesterol-lowering therapy [142] and blood pressure management [545].
4.a. Cigarette smoking
4.b. Hypertension—
A patient is classified as having hypertension if systolic blood pressure is ≥ 140 mm Hg or diastolic blood pressure is ≥ 90 mm Hg, or if the patient is taking antihypertensive agents.
4.c. High-risk low-density lipoprotein cholesterol—
A high-risk LDL-cholesterol is defined as a serum concentration of ≥160 mg/dL. A borderline high-risk LDL-cholesterol (130 to 159 mg/dL) together with two or more other risk factors also confers high risk.
4.d. Low high-density lipoprotein cholesterol—
A low HDL-cholesterol is defined as a serum concentration of < 35 mg/dL.
4.e. Impaired fasting glucose (IFG)—
The presence of clinical type 2 diabetes (fasting plasma glucose of ≥ 126 mg/dL or 2 hours postprandial plasma glucose of ≥ 200 mg/dL) is a major risk factor for CVD, and its presence alone places a patient in the category of very high absolute risk (see above). IFG (fasting plasma glucose 110 to 125 mg/dL) is considered by many authorities to be an independent risk factor for cardiovascular (macrovascular) disease, justifying its inclusion among risk factors contributing to high absolute risk. Although including IFG as a separate risk factor for CVD departs from the ATP II and JNC VI reports, its inclusion in this list may be appropriate. IFG is well established as a risk factor for type 2 diabetes.
4.f. Family history of premature CHD—
A positive family history of premature CHD is defined as definite myocardial infarction or sudden death at or before 55 years of age in the father or other male first-degree relative, or at or before 65 years of age in the mother or other female first-degree relative.
4.g. Age
4.g.1. Male ≥ 45 years
4.g.2. Female ≥ 55 years (or postmenopausal)
Methods for estimating absolute risk status for developing CVD based on these risk factors are described in detail in the ATP II and JNC VI reports. The intensity of intervention for high blood cholesterol or hypertension is adjusted depending on the absolute risk estimated by these factors. Approaches to therapy for cholesterol disorders and hypertension are described in the ATP II and JNC VI, respectively.
5. Other risk factors
Other risk factors deserve special consideration for their relation to obesity. When these factors are present, patients can be considered to have incremental absolute risk above that estimated from the preceding risk factors. Quantitative risk contributions are not available for these risk factors, but their presence heightens the need for weight reduction in obese persons.
5.a. Physical inactivity—
A lack of physical activity imparts an increased risk for both CVD and type 2 diabetes. Physical inactivity enhances the severity of other risk factors, but it also has been shown to be an “independent” risk factor for all-cause mortality or CVD mortality [411, 548]. Although physical inactivity is not listed as a risk factor that modifies the intensity of therapy required for elevated cholesterol or blood pressure, increased physical activity is indicated for management of these conditions (see the ATP II and JNC VI). Increased physical activity is especially needed in obese patients because it promotes weight reduction and favorably modifies obesity-associated risk factors. Conversely, the presence of physical inactivity in an obese person warrants intensified efforts to remove excess body weight, because physical inactivity and obesity both heighten disease risks.
5.b. High triglycerides—
Obesity is commonly accompanied by elevated serum triglycerides. The relationship between high triglycerides and CHD is complex. Triglyceride-rich lipoproteins may be directly atherogenic. In addition, elevated serum triglycerides are the most common manifestation of the atherogenic lipoprotein phenotype (high triglycerides, small LDL particles, and low HDL-cholesterol levels) [142, 549]. Moreover, in the presence of obesity, high serum triglycerides are commonly associated with a clustering of metabolic risk factors known as the metabolic syndrome (atherogenic lipoprotein phenotype, hypertension, insulin resistance and glucose intolerance, and prothrombotic states). Thus, in obese patients, elevated serum triglycerides are a marker for increased cardiovascular risk. According to current guidelines (ATP II and JNC VI), the presence of high triglycerides does not modify the intensity of cholesterol or blood pressure-lowering therapy. Their presence in obese patients, however, calls for an intensified effort to achieve weight reduction and increase physical activity. Both will reduce the various risk factors characteristic of the metabolic syndrome, and thus should reduce overall cardiovascular risk as well as decrease the risk for type 2 diabetes.
According to the ATP II guidelines [142], triglyceride levels are classified as follows:
Patients with very high triglycerides are at increased risk for acute pancreatitis and must undergo immediate triglyceride-lowering therapy.
D. Evaluation and Treatment Strategy
When physicians encounter patients in the clinical setting, the opportunity exists for identifying overweight and obesity and accompanying risk factors and for initiating treatment for both the weight and the risk factors, as well as chronic diseases such as CVD and type 2 diabetes. When assessing a patient for treatment of overweight and obesity, consider the patient's weight, waist circumference, and the presence of risk factors. The strategy for the evaluation and treatment of overweight patients is presented in Figure 6 (Treatment Algorithm). This algorithm applies only to the assessment for overweight and obesity and subsequent decisions based on that assessment. It does not reflect any initial overall testing for other conditions and diseases that the physician may wish to do. Approaches to therapy for cholesterol disorders and hypertension are described in ATP II and JNC VI, respectively. In overweight patients, control of cardiovascular risk factors deserves equal emphasis as weight loss therapy. Reductions of risk factors will reduce the risk for cardiovascular disease whether or not efforts at weight loss are successful. The panel recognizes that the assessment for overweight and obesity may take place as part of an overall health assessment; however, for clarity, the algorithm focuses only on the evaluation and treatment of overweight and obesity. Each step (designated by a box) in this process is reviewed in this section and expanded upon in subsequent sections.
| Category | Serum Triglyceride Levels |
|---|---|
| Normal triglycerides | Less than 200 mg/dL |
| Borderline-high triglycerides | 200 to 400 mg/dL |
| High triglycerides | 400 to 1,000 mg/dL |
| Very high triglycerides | Greater than 1,000 mg/dL |
Box 1: “Patient Encounter”
A patient encounter is defined as any interaction between a health care practitioner (generally a physician, nurse practitioner or physician's assistant) that provides the opportunity to assess a patient's weight status and provide advice, counseling, or treatment.
Box 2: “History of Overweight or Recorded BMI ≥ 25”
The practitioner must seek to determine whether the patient has ever been overweight. While a technical definition is provided, a simple question such as “Have you ever been overweight?” will accomplish the same goal. Questions directed towards weight history, dietary habits, physical activities, and medications may provide useful information about the origins of obesity in particular patients.
Box 3: “BMI Measured in Past 2 Years”
For those who have not been overweight, a 2-year interval is appropriate for the reassessment of BMI. While this time span is not evidence-based, it is believed to be a reasonable compromise between the need to identify weight gain at an early stage and the need to limit the time, effort, and cost of repeated measurements.
Box 4: “Measure Weight, Height, Waist Circumference; Calculate BMI”
Weight must be measured so that the BMI can be calculated. Most charts are based on weights obtained with the patient wearing undergarments and no shoes. BMI can be manually calculated (kg/[height in meters]2), but is more easily obtained from a nomogram (see Appendix V). Waist circumference is important because evidence suggests that abdominal fat is a particularly strong determinant of cardiovascular risk in those with a BMI of 25 to 34.9 kg/m2. Increased waist circumference can also be a marker of increased risk even in persons of normal weight. The technique for measuring waist circumference is described on page 58. A nutrition assessment will also help to assess the diet and physical activity habits of overweight patients.
Box 5: “BMI ≥ 25, OR Waist Circumference > 88 cm(F) or > 102 cm(M)”
These cutpoints divide overweight from normal weight and are consistent with other national and international guidelines. The relation between weight and mortality is J-shaped, and evidence suggests that the right side of the “J” begins to rise at a BMI of 25. Waist circumference is incorporated as an “or” factor because some patients with BMI lower than 25 will have disproportionate abdominal fat, and this increases their cardiovascular risk despite their low BMI (see page 61). These abdominal circumference values are not necessary for patients with a BMI ≥ 35 kg/m2.
Box 6: “Assess Risk Factors”
Risk assessment for CVD and diabetes in a person with evident obesity will include special considerations for the history, physical examination, and laboratory examination. Of greatest urgency is the need to detect existing CVD or end-organ damage. Since the major risk of obesity is indirect (obesity elicits or aggravates hypertension, dyslipidemias, and diabetes, which cause cardiovascular complications), the management of obesity should be implemented in the context of these other risk factors. While there is no direct evidence demonstrating that addressing risk factors increases weight loss, treating the risk factors through weight loss is a recommended strategy. The risk factors that should be considered are provided on pages 63–65. With regard to age, please see commentary on pages 90–91.
Box 7: “BMI ≥ 30, OR ([BMI 25 to 29.9 OR Waist Circumference > 88 cm(F) or > 102 cm(M)] AND ≥ 2 risk factors)”
The panel recommends that all patients meeting these criteria attempt to lose weight. However, it is important to ask the patient whether or not they want to lose weight. Those with BMIs between 25 and 29.9 kg/m2 who have one or no risk factors should work on maintaining their current weight rather than embark on a weight reduction program. The panel recognizes that the decision to lose weight must be made in the context of other risk factors (e.g., quitting smoking is more important than losing weight) and patient preferences.
Box 8: “Clinician and Patient Devise Goals”
The decision to lose weight must be made jointly between the clinician and patient. Patient involvement and investment is crucial to success. The patient may choose not to lose weight but rather to prevent further weight gain as a goal. The panel recommends as an initial goal the loss of 10 percent of baseline weight, to be lost at a rate of 1 to 2 lb/week, establishing an energy deficit of 500 to 1,000 kcal/day. (See pages 71–72.) For individuals who are overweight, a deficit or 300 to 500 kcal/day may be more appropriate, providing a weight loss of about 1/2 lb/week. Also, there is evidence that an average of 8 percent of weight can be lost in a 6-month period. Since the observed average 8 percent weight loss includes people who do not lose weight, an individual goal of 10 percent is reasonable. After 6 months, most patients will equilibrate (caloric intake balancing energy expenditure) and will require adjustment of energy balance if they are to lose more weight. (See pages 72–73.)
The three major components of weight loss therapy are dietary therapy, increased physical activity, and behavior therapy. (See pages 73–82.) Lifestyle therapy should be tried for at least six months before considering pharmacotherapy. In addition, pharmacotherapy should be considered as an adjunct to lifestyle therapy in patients with a BMI ≥ 30 with no concomitant obesity-related risk factors or diseases, or for patients with a BMI ≥ 27 with concomitant obesity-related risk factors or diseases. The risk factors or diseases considered important enough to warrant pharmacotherapy at a BMI of 27 to 29.9 are hypertension, dyslipidemia, CHD, type 2 diabetes, and sleep apnea. However, sibutramine, the only FDA approved drug for long-term use, should not be used in patients with a history of hypertension, CHD, congestive heart failure, arrhythmias, or history of stroke. Certain patients may be candidates for weight loss surgery. Each component of weight loss therapy can be introduced briefly. The selection of weight loss methods should be made in the context of patient preferences, analysis of past failed attempts, and consideration of the available resources.
Box 9: “Progress Being Made/Goal Achieved”
During the acute weight loss period and at 6-month and 1-year follow-up visits, the patients should be weighed, BMI calculated, and progress assessed. If at any time it appears that the program is failing, a reassessment should take place to determine the reasons (see Box 10). If pharmacotherapy is being used, appropriate monitoring for side effects is recommended (See page 86). If a patient can achieve the recommended 10 percent reduction in body weight in 6 months to 1 year, this change in weight can be considered good progress. The patient can then enter the phase of weight maintenance and long-term monitoring. It is important for the practitioner to recognize that some persons are more apt to lose or gain weight on a given regimen and that this phenomenon cannot always be attributed to degree of compliance. However, if significant obesity remains and absolute risk from obesity-associated risk factors remains high, at some point an effort should be made to reinstitute weight loss therapy to achieve further weight reduction. Once a limit of weight loss has been obtained, the practitioner is responsible for long-term monitoring of risk factors and for encouraging the patient to maintain a reduced weight level.
Box 10: “Assess Reasons for Failure to Lose Weight”
If a patient fails to achieve the recommended 10 percent reduction in body weight in 6 months or 1 year, a reevaluation is required. A critical question is whether the level of motivation is high enough to continue clinical therapy. If motivation is high, revise the goals and strategies (see Box 8). If motivation is not high, clinical therapy should be discontinued, but the patient should be encouraged to embark on efforts to lose weight or to at least avoid further weight gain. Even if weight loss therapy is stopped, risk factor management must be continued.
Failure to achieve weight loss should prompt the practitioner to investigate energy intake (dietary recall including alcohol intake, daily intake logs), energy expenditure (physical activity diary), attendance at behavior therapy group meetings, recent negative life events, family and societal pressures, or evidence of detrimental psychiatric problems (depression, binge eating disorder). If attempts to lose weight have failed, and the BMI is ≥ 40, surgical therapy should be considered.
Box 11: “Maintenance Counseling”
Evidence suggests that over 80 percent of persons who lose weight will gradually regain it (see page 72). Patients who continue on weight maintenance programs have a greater chance of keeping weight off. Maintenance consists of continued contact with the health care practitioner for continued education, support, and medical monitoring (see page 72 and 75).
Box 12: “Does the Patient Want to Lose Weight?”
All patients who are overweight (BMI 25 to 29.9), or do not have a high waist circumference, and have few (0 to 1) cardiovascular risk factors and do not want to lose weight, should be counseled regarding the need to keep their weight at or below its present level. Patients who wish to lose weight should be guided per Boxes 8 and 9. The justification for offering these overweight patients the option of maintaining (rather than losing) weight is that their health risk, while higher than that of persons with a BMI < 25, is only moderately increased (page 62).
Box 13: “Advise to Maintain Weight/Address Other Risk Factors”
Those who have a history of overweight and are now at appropriate weight, and those who are overweight and not obese but wish to focus on maintenance of their current weight, should be provided with counseling and advice so that their weight does not increase. An increase in weight increases their health risk and should be prevented. The physician should actively promote prevention strategies including enhanced attention by the patient to diet, physical activity, and behavior therapy. For addressing other risk factors, see Box 6, because even if weight loss cannot be addressed, other risk factors should be covered.
Box 14: “History of BMI ≥ 25”
This box differentiates those who are not overweight now and never have been from those with a history of overweight; see Box 2.
Box 15: “Brief Reinforcement”
Those who are not overweight and never have been should be advised of the importance of staying in this category.
Box 16: “Periodic Weight, BMI, and Waist Circumference Check”
Patients should receive periodic monitoring of their weight, BMI, and waist circumference. Patients who are not overweight or have no history of overweight should be screened for weight gain every 2 years. This time span is a reasonable compromise between the need to identify weight gain at an early stage and the need to limit the time, effort, and the cost of repeated measurements.
E. Exclusion from Weight Loss Therapy
Patients in whom weight loss therapy is not appropriate include most pregnant or lactating women, those with serious psychiatric illness, and patients who have a variety of serious illnesses in whom caloric restriction might exacerbate the illness.
F. Patient Motivation
Assessment of patient motivation is a prerequisite for weight loss therapy. Weight reduction in the clinical setting represents a major investment of time and effort on the part of the health care team and expense to the patient. For these reasons, motivation for weight loss should be relatively high before initiating clinical therapy. At the same time, it is the duty of the primary care practitioner to heighten a patient's motivation for weight loss when such is perceived to be of significant benefit for risk reduction. This can be done by enumerating the dangers associated with persistent obesity and by describing the strategy for clinically assisted weight reduction. For patients who are not motivated (or able) to enter clinical weight loss therapy, appropriate management of risk factors (e.g., high serum cholesterol, hypertension, smoking, and type 2 diabetes) is still necessary. Sustained weight reduction may facilitate control of cardiovascular risk factors and delay the onset of type 2 diabetes.
Evidence Statement
Patient motivation is a key component for success in a weight loss program. Evidence Category D.
Rationale: Assessment of the patient's motivation for treatment by the practitioner is important in the decision to initiate a weight loss program. The following factors must be evaluated:
- Reasons and motivation for weight loss—What is the extent of the patient's seriousness and readiness to undergo a sustained period of weight loss at this time? What is the patient's current attitude about making a lifelong commitment to behavior change?
- Previous history of successful and unsuccessful weight loss attempts—What factors were responsible for previous failures and successes at weight loss or maintenance of normal body weight?
- Family, friends, and work-site support—What is the social framework in which the patient will attempt to lose weight, and who are the possible helpers and antagonists to such an attempt?
- The patient's understanding of overweight and obesity and how it contributes to obesity-associated diseases—Does the patient have an appreciation of the dangers of obesity, and are these dangers of significant concern to the patient?
- Attitude toward physical activity—Is the patient motivated to enter a program of increased physical activity to assist in weight reduction?
- Time availability—Is the patient willing to commit the time required to interact with health professionals in long-term weight loss therapy?
- Barriers—What are the obstacles that will interfere with the patient's ability to implement the suggestions for change?
- Financial considerations—Is the patient willing to pay for obesity therapy? This may include having to pay for travel to the medical facility, time lost from work, and paying for professional counseling that is not covered by insurance.
One of the most important aspects of the initial evaluation is to prepare patients for treatment. Reviewing patients' past attempts at weight loss and explaining how the new treatment plan will be different can encourage patients and provide hope for successful weight loss. It is helpful to discuss the proposed course of treatment and describe necessary behaviors, such as keeping diaries of food intake and physical activity.
Finally, given the social stigmatization that obese patients often feel, even from health care professionals, the initial evaluation is an opportunity to show the patient respect, concern, and hope [550]. A patient who has shared feelings about being overweight and previous attempts to lose weight with a sympathetic listener may be more willing to consider new ideas and information. A partnership in which the patient feels supported and understood can help to sustain the necessary motivation for the difficult task of weight loss and maintenance [551, 552].
RECOMMENDATION
Practitioners need to assess the patient's motivation to enter weight loss therapy; assess the readiness of the patient to implement the plan; and then take appropriate steps to motivate the patient for treatment. Evidence Category D.
G. Goals of Weight Loss and Management
The general goals of weight loss and management are: (1) to reduce body weight; and (2) to maintain a lower body weight over the long term; or (3) at a minimum, to prevent further weight gain. Specific targets for each of these goals can be considered.
1. Weight Loss
1.a. Target levels for weight loss—
The initial target goal of weight loss therapy for overweight patients is to decrease body weight by about 10 percent. If this target can be achieved, consideration can be given to the next step of further weight loss.
Evidence Statement
Overweight and obese patients in well-designed programs can achieve a weight loss of as much as 10 percent of baseline weight, a weight loss that can be maintained for a sustained period of time (1 year or longer). Evidence Category A.
Rationale: The rationale for this initial goal is that even moderate weight loss, i.e., 10 percent of initial body weight, can significantly decrease the severity of obesity-associated risk factors. It can also set the stage for further weight loss, if indicated. Available evidence indicates that an average weight loss of 8 percent can be achieved in 6 months; however, since the observed average 8 percent includes people who do not lose weight, an individual goal of 10 percent is reasonable. This degree of weight loss can be achieved and is realistic, and moderate weight loss can be maintained over time. It is better to maintain a moderate weight loss over a prolonged period than to regain from a marked weight loss. The latter is counterproductive in terms of time, costs, and self-esteem. Patients generally will wish to lose more weight than 10 percent, and will need to be counseled and persuaded of the appropriateness of this initial goal [553, 554]. Further weight loss can be considered after this initial goal is achieved and maintained for 6 months.
RECOMMENDATION
The initial goal of weight loss therapy should be to reduce body weight by approximately 10 percent from baseline. With success, further weight loss can be attempted, if indicated through further assessment. Evidence Category A.
1.b. Rate of weight loss—
A reasonable time line for weight loss is to achieve a 10 percent reduction in body weight over 6 months of therapy. For overweight patients with BMIs in the typical range of 27 to 35, a decrease of 300 to 500 kcal/day will result in weight losses of about ½ to 1 lb/week and a 10 percent weight loss in 6 months. For more severely obese patients with BMIs ≥ 35, deficits of up to 500 to 1,000 kcal/day will lead to weight losses of about 1 to 2 lb/week and a 10 percent weight loss in 6 months.
Evidence Statement
Weight loss at the rate of 1 to 2 lb/week (calorie deficit of 500 to 1,000 kcal/day) commonly occurs for up to 6 months, at which point weight loss begins to plateau unless a more restrictive regimen is implemented. Evidence Category B.
Rationale: To achieve significant weight loss, an energy deficit must be created and maintained. Weight can be lost at a rate of 1 to 2 lb/week with a calorie deficit of 500 to 1,000 kcal/day. After 6 months, this caloric deficit theoretically should result in a loss of 26 to 52 lb. However, the average amount of weight lost actually observed over this time period usually is in the range of 20 to 25 lb. A greater rate of weight loss does not yield a better result at the end of 1 year [437]. It is difficult for most patients to continue to lose weight after a period of 6 months due to changes in resting metabolic rates and difficulty in adhering to treatment strategies, although some can do so. To continue to lose weight, diet and physical activity goals need to be revised to create an energy deficit at the lower weight, since energy requirements decrease as weight is decreased. To achieve additional weight loss, the patient must further decrease calories and/or increase physical activity. Many studies show that rapid weight reduction almost always is followed by regaining of weight. Moreover, with rapid weight reduction, there is an increased risk for gallstones and, possibly, electrolyte abnormalities.
RECOMMENDATION
Weight loss should be about 1 to 2 lb/week for a period of 6 months with the subsequent strategy based on the amount of weight lost. Evidence Category B.
2. Weight Maintenance at Lower Weight
Once the goals of weight loss have been successfully achieved, maintenance of a lower body weight becomes a major challenge. In the past, obtaining the goal of weight loss has been considered the end of weight loss therapy. Unfortunately, once patients are dismissed from clinical therapy, they frequently regain the lost weight. This report recommends that observation, monitoring, and encouragement of patients who have successfully lost weight be continued on a long-term basis.
Evidence Statement
After 6 months of weight loss treatment, efforts to maintain weight loss through diet, physical activity, and behavior therapy are important. Evidence Category B.
Rationale: After 6 months of weight loss, the rate of weight loss usually declines and plateaus [395, 507, 555]. The primary care practitioner and patient should recognize that at this point, weight maintenance, the second phase of the weight loss effort, should take priority. Successful weight maintenance is defined as a weight regain of < 3 kg (6.6 lb) in 2 years and a sustained reduction in waist circumference of at least 4 cm. If a patient wishes to lose more weight after a period of weight maintenance, the procedure for weight loss outlined above can be repeated.
RECOMMENDATION
A weight maintenance program should be a priority after the initial 6 months of weight loss therapy. Evidence Category B.
Evidence Statement
Lost weight usually will be regained unless a weight maintenance program consisting of dietary therapy, physical activity, and behavior therapy is continued indefinitely. Drug therapy can also be used; however, drug safety and efficacy beyond 1 year of total treatment have not been established. Evidence Category B.
Rationale: After a patient has achieved the goals of weight loss, the combined modalities of therapy (dietary therapy, physical activity, and behavior therapy) must be continued indefinitely; otherwise, excess weight likely will be regained. Numerous strategies are available for motivating the patient; all of these require that the practitioner continue to communicate frequently with the patient. Long-term monitoring and encouragement can be accomplished in several ways: by regular clinic visits, at group meetings, or via telephone or E-mail. The longer the weight maintenance phase can be sustained, the better the prospects for long-term success in weight reduction. Drug therapy may also be helpful during the weight maintenance phase.
RECOMMENDATION
After successful weight loss, the likelihood of weight loss maintenance is enhanced by a program consisting of dietary therapy, physical activity, and behavior therapy, which should be continued indefinitely. Drug therapy can also be used. However, drug safety and efficacy beyond 1 year of total treatment have not been established. Evidence Category B.
3. Prevention of Further Weight Gain
Some patients may not be able to achieve significant weight reduction. In such patients, an important goal is to prevent further weight gain that would exacerbate disease risk. Thus, prevention of further weight gain may justify entering a patient into weight loss therapy. Prevention of further weight gain can be considered a partial therapeutic success for many patients. Moreover, if further weight gain can be prevented, this achievement may be an important first step toward beginning the weight loss process. Primary care practitioners ought to recognize the importance of this goal for those patients who are not able to immediately lose weight. The need to prevent weight gain may warrant maintaining patients in a weight management program for an extended period.
H. Strategies for Weight Loss and Weight Maintenance
1. Dietary Therapy
In the majority of overweight and obese patients, adjustment of the diet to reduce caloric intake will be required. Dietary therapy consists, in large part, of instructing patients on how to modify their diets to achieve a decrease in caloric intake. A key element of the current recommendation is the use of a moderate reduction in caloric intake to achieve a slow but progressive weight loss. Ideally, caloric intake should be reduced only to the level required to maintain weight at the desired level. If this level of caloric intake is achieved, excess weight will gradually disappear. In practice, somewhat greater caloric deficits are used in the period of active weight loss, but diets with very low calories are to be avoided. Finally the composition of the diet should be modified to minimize other cardiovascular risk factors [142].
The centerpiece of dietary therapy for weight loss in overweight patients is a low-calorie diet (LCD) (800 to 1,500 kcal/day). This diet is to be distinguished from a very low-calorie diet (VLCD) (250 to 800 kcal/day), which has been unsuccessful in achieving weight loss over the long term. The LCD recommended in this report also contains nutrient compositions that will decrease other risk factors, notably, high serum cholesterol and hypertension.
Evidence Statement
LCDs can reduce total body weight by an average of 8 percent and help reduce abdominal fat content over a period of approximately 6 months. Evidence Category A.
Rationale: A decrease in calorie intake is the most important dietary component of weight loss and maintenance. LCDs have been shown to reduce total body weight by an average of 8 percent over a period of 6 months, accompanied by significant reductions in waist circumference. Since this represents an average that includes individuals who did not lose weight, an individual average goal of 10 percent is feasible. When weight loss occurs, the loss consists of about 75 percent fat and 25 percent lean tissue [556, 557]. A deficit of 500 to 1,000 kcal/day will produce a weight loss of 70 to 140 grams/day, or 490 to 980 grams/week (1 to 2 lb/week). A deficit of 300 to 500 kcal/day will produce a weight loss of 40 to 70 grams/day, or 280 to 490 grams/week (1/2 to 1 lb/week) A patient may choose a diet of 1,000 to 1,200 kcal for women and 1,200 to 1,500 kcal for men.
VLCDs (less than 800 kcal/day) are not recommended for weight loss therapy because the deficits are too great, and nutritional inadequacies will occur unless VLCDs are supplemented with vitamins and minerals [558]. Moreover, clinical trials show that LCDs are just as effective as VLCDs in producing weight loss after 1 year [437]. Although more weight is initially lost with VLCDs, more is usually regained. Further, rapid weight reduction does not allow for gradual acquisition of changes in eating behavior. Successful behavior therapy is the key to long-term maintenance of weight at a reduced level. Finally, patients using VLCDs are at increased risk for developing gallstones.
Successful weight reduction by LCDs is more likely to occur when consideration is given to a patient's food preferences in tailoring a particular diet. Care should be taken to be sure that all of the recommended dietary allowances are met; this may require use of a dietary supplement. Dietary education is a necessary ingredient in achieving adjustment to an LCD. Educational efforts should pay particular attention to the following topics:
- energy value of different foods;
- food composition—fats, carbohydrates (including dietary fiber), and proteins;
- reading nutrition labels to determine caloric content and food composition;
- new habits of purchasing—preference to low-calorie foods;
- food preparation—avoiding adding high-calorie ingredients during cooking (e.g., fats and oils);
- avoiding overconsumption of high-calorie foods (both high-fat and high-carbohydrate foods);
- maintain adequate water intake
- reducing portion sizes; and
- limiting alcohol consumption.
- The Step I Diet in ATP II provides an appropriate nutrient composition for an LCD diet. The composition of the diet is presented in Table IV-3. Additional practical dietary advice for patients is included in Appendix VI.
RECOMMENDATION
A diet that is individually planned to help create a deficit of 500 to 1,000 kcal/day should be an integral part of any program aimed at achieving a weight loss of 1 to 2 lb/week. Evidence Category A.
RECOMMENDATION
Reducing dietary fat alone without reducing calories is not sufficient for weight loss. However, reducing dietary fat, along with reducing dietary carbohydrates, can facilitate caloric reduction. Evidence Category A.
Evidence Statement
Optimally, dietary therapy should last at least 6 months. Evidence Category A.
Rationale: Many studies suggest that the rate of weight loss diminishes after about 6 months. Shorter periods of dietary therapy usually result in lesser weight reductions. Therapeutic efforts should be directed toward behavior therapy as well as maintaining LCDs [486, 570, 571].
Evidence Statement
During dietary therapy, frequent contacts between professional counselors and patients promote weight loss and maintenance. Evidence Category C.
Rationale: Frequent clinical encounters during the initial 6 months of weight reduction appear to facilitate reaching the goals of therapy. During the period of active weight loss, regular visits of at least once per month and preferably more often with a health professional for the purposes of reinforcement, encouragement, and monitoring will facilitate weight reduction. Weekly group meetings can be conducted at a low cost, and can contribute to favorable behavior changes. However, no clinical trials have been specifically designed to test the relative efficacy of different frequencies of encounters with physicians, dietitians, or others in the weight loss team [487].
Evidence Statement
The amount of time spent with the patient favorably affects weight change in overweight or obese adults given dietary therapy. Evidence Category D.
Rationale: Training of a health professional in techniques of weight reduction, especially in behavior therapy and dietary principles, is expected to facilitate weight reduction. Further, adequate time must be made available to the patient to convey the information necessary, to reinforce behavioral and dietary messages, and to monitor the patient's response. Despite these judgments, none of the studies reviewed were designed to specifically address the type or qualifications of the health professional who implemented the various weight loss approaches. Many of the studies differed in the types of dietary intervention provided. Most programs involved dietitians and nutritionists as primary therapists and used group therapy rather than individual sessions. The length of time spent during each session and the nature of the practitioner/patient interaction tended not to be provided.
RECOMMENDATION
The literature suggests that weight loss and weight maintenance therapies that provide a greater frequency of contacts between the patient and the practitioner and are provided over the long term should be put in place. This can lead to more successful weight loss and weight maintenance. Evidence Category C.
2. Physical Activity
An increase in physical activity is an important component of weight loss therapy since it leads to increased expenditure of energy. Increased physical activity may also inhibit food intake in overweight patients. Physical activity can also be helpful in maintaining a desirable weight. In addition, sustained physical activity has the benefit of reducing overall CHD risk beyond that produced by weight reduction alone.
Several experts believe that a progressive decrease in the amount of energy expended for work, transportation, and personal chores is a major cause of obesity in the United States. These authorities note that total caloric intake has not increased over the last few decades; instead, the caloric imbalance leading to overweight and obesity is the result of a substantial decrease in physical activity and, consequently, a decrease in daily energy expenditure. However, this hypothesis is difficult to prove because appropriate data are lacking. Successful restoration of normal weight in many overweight and obese persons requires a higher level of energy expenditure. Increased regular physical activity is the way to achieve this goal of augmenting daily energy expenditure.
Evidence Statement
Physical activity contributes to weight loss, both alone and when it is combined with dietary therapy. Evidence Category A.
Rationale: Increased physical activity alone can create a caloric deficit and can contribute to weight loss. However, efforts to achieve weight loss through physical activity alone generally produce an average of a 2 to 3 percent decrease in body weight or BMI. Even so, increased physical activity is a useful adjunct to LCDs in promoting weight reduction.
Evidence Statement
Physical activity in overweight and obese adults increases cardiorespiratory fitness independent of weight loss. Evidence Category A.
Rationale: There is strong evidence that increased physical activity increases cardiorespiratory fitness, with or without weight loss [346, 363, 369, 375, 401, 404, 406, 432, 434, 445, 447, 448]. Improved cardiovascular fitness also improves the quality of life in overweight patients by improving mood, self-esteem, and physical function in daily activities [572].
Evidence Statement
Physical activity independently reduces CVD risk factors (Evidence Category A), and reduces risk for cardiovascular disease. Evidence Category C.
Rationale: There is considerable evidence that physical inactivity is an independent risk factor for CVD and diabetes [572]. Furthermore, the more active an individual is, the lower the risk. By the same token, increased physical activity appears to independently reduce risk for CVD morbidity and mortality, and diabetes [411, 548, 573, 574]. Physical activity reduces elevated levels of CVD risk factors, including blood pressure and triglycerides, increases HDL-cholesterol, and improves glucose tolerance with or without weight loss [572].
Evidence Statement
Physical activity contributes to a decrease in body fat, including a modest effect on abdominal fat. Evidence Category B.
Rationale: Physical activity appears to have a favorable effect on distribution of body fat [572]. Several large cross-sectional studies in Europe [464], Canada [575], and the United States [466–468] showed an inverse association between energy expenditure through physical activity and several indicators of body fat distribution, such as WHR and waist-to-thigh circumference ratio. Fewer data are available on the effects of physical activity on waist circumference, although the ratio changes noted above suggest a decrease in abdominal obesity. Only a few randomized controlled trials that have tested the effect of physical activity on weight loss measured waist circumference. In some (but not all) studies, physical activity was found to produce only modest weight loss and decreased waist circumference [365, 369, 375]. However, it is not known whether the effects of physical activity on abdominal fat are independent of weight loss.
2.a. Strategies to increase physical activity
Many people live sedentary lives, have little training or skills in physical activity, and are difficult to motivate toward increasing their activity. For these reasons, starting a physical activity regimen may require supervision for some people. The need to avoid injury during physical activity is high. Extremely obese persons may need to start with simple exercises that can gradually be intensified. The practitioner must decide whether exercise testing for cardiopulmonary disease is needed before embarking on a new physical activity regimen. This decision should be based on a patient's age, symptoms, and concomitant risk factors.
For most obese patients, physical activity should be initiated slowly, and the intensity should be increased gradually. Initial activities may be walking or swimming at a slow pace. With time, depending on progress, the amount of weight lost, and functional capacity, the patient may engage in more strenuous activities. Some of these include fitness walking, cycling, rowing, cross-country skiing, aerobic dancing, and rope jumping. Jogging provides a high-intensity aerobic exercise, but can lead to orthopedic injury. If jogging is desired, the patient's ability to do this must first be assessed. The availability of a safe environment for the jogger is also a necessity. Competitive sports, such as tennis and volleyball, can provide an enjoyable form of physical activity for many, but again, care must be taken to avoid injury, especially in older people. As the examples listed in Table IV-4 show, a moderate amount of physical activity can be achieved in a variety of ways. People can select activities that they enjoy and that fit into their daily lives. Because amounts of activity are functions of duration, intensity, and frequency, the same amounts of activity can be obtained in longer sessions of moderately intense activities (such as brisk walking) as in shorter sessions of more strenuous activities (such as running).
A regimen of daily walking is an attractive form of physical activity for many people, particularly those who are overweight or obese. The patient can start by walking 10 minutes, 3 days a week, and can build to 30 to 45 minutes of more intense walking at least 5 days a week and preferably most, if not all, days [577, 578]. With this regimen, an additional 100 to 200 calories per day of physical activity can be expended. Caloric expenditure will vary depending on the individual's body weight and intensity of the activity (see Table IV-5).
This regimen can be adapted to other forms of physical activity, but walking is particularly attractive because of its safety and accessibility. With time, a larger weekly volume of physical activity can be performed that would normally cause a greater weight loss if it were not compensated by a higher caloric intake.
Reducing sedentary time is another approach to increasing activity. Patients should be encouraged to build physical activities into each day. Examples include leaving public transportation one stop before the usual one, parking further than usual from work or shopping, and walking up stairs instead of taking elevators or escalators. New forms of physical activity should be suggested, e.g., gardening, walking a dog daily, or new athletic activities. Engaging in physical activity can be facilitated by identifying a safe area to perform the activity, e.g., community parks, gyms, pools, and health clubs. However, when these sites are not available, an area of the home can be identified and perhaps outfitted with equipment such as a stationary bicycle or a treadmill.
Health professionals should encourage patients to plan and schedule physical activity 1 week in advance, budget the time necessary to do it, and document their physical activity by keeping a diary and recording the duration and intensity of exercise.
RECOMMENDATION
Physical activity should be an integral part of weight loss therapy and weight maintenance. Evidence Category A. Initially, moderate levels of physical activity for 30 to 45 minutes, 3 to 5 days per week should be encouraged. All adults should set a long-term goal to accumulate at least 30 minutes or more of moderate-intensity physical activity on most, and preferably all, days of the week. Evidence Category B.
3. Behavior Therapy
Behavioral strategies to reinforce changes in diet and physical activity can produce a weight loss in obese adults in the range of 10 percent of baseline weight over 4 months to 1 year. Unless a patient acquires a new set of eating and physical activity habits, long-term weight reduction is unlikely to succeed. The acquisition of new habits is particularly important for long-term weight maintenance at a lower weight. Most patients return to baseline weights in the absence of continued intervention. Thus, the physician or staff members must become familiar with techniques for modifying life habits of overweight or obese patients.
The goal of behavior therapy is to alter the eating and activity habits of an obese patient. Techniques for behavior therapy have been developed to assist patients in modifying their life habits.
Evidence Statement
Behavior therapy, in combination with an energy deficit, provides additional benefits in assisting patients to lose weight short-term (1 year). Its effectiveness for long-term weight maintenance has not been shown in the absence of continued behavioral intervention. Evidence Category B.
Rationale: The primary assumptions of behavior therapy are that:
- by changing eating and physical activity habits, it is possible to change body weight;
- patterns of eating and physical activity are learned behaviors and can be modified; and
- to change these patterns over the long term, the environment must be changed.
- Behavior therapies provide methods for overcoming barriers to compliance with dietary therapy and/or increased physical activity, and are thus important components of weight loss therapy. Most weight loss programs incorporating behavioral strategies do so as a package that includes education about nutrition and physical activity. However, this standard “package” of management should not ignore the need for individualizing behavioral strategies [579].
3.a. Behavior Therapy Strategies Used in Weight Loss and Weight Maintenance Programs
Studies reviewed for this report examined a range of modalities of behavioral therapy. No single method or combination of behavioral methods proved to be clearly superior. Thus, various strategies can be used by the practitioner to modify patient behavior. The aim is to change eating and physical activities behaviors over the long term. Such change can be achieved either on an individual basis or in group settings. Group therapy has the advantage of lower cost. Specific behavioral strategies include the following:
- Self-monitoring of both eating habits and physical activity—Objectifying one's own behavior through observation and recording is a key step in behavior therapy. Patients should be taught to record the amount and types of food they eat, the caloric values, and nutrient composition. Keeping a record of the frequency, intensity, and type of physical activity likewise will add insight to personal behavior. Extending records to time, place, and feelings related to eating and physical activity will help to bring previously unrecognized behavior to light [580].
- Stress management—Stress can trigger dysfunctional eating patterns, and stress management can defuse situations leading to overeating. Coping strategies, meditation, and relaxation techniques all have been successfully employed to reduce stress.
- Stimulus control—Identifying stimuli that may encourage incidental eating enables individuals to limit their exposure to high-risk situations. Examples of stimulus control strategies include learning to shop carefully for healthy foods, keeping high-calorie foods out of the house, limiting the times and places of eating, and consciously avoiding situations in which overeating occurs [580].
- Problem solving—This term refers to the self-correction of problem areas related to eating and physical activity. Approaches to problem solving include identifying weight-related problems, generating or brainstorming possible solutions and choosing one, planning and implementing the healthier alternative, and evaluating the outcome of possible changes in behavior [580]. Patients should be encouraged to reevaluate setbacks in behavior and to ask “What did I learn from this attempt?” rather than punishing themselves.
- Contingency management—Behavior can be changed by use of rewards for specific actions, such as increasing time spent walking or reducing consumption of specific foods [44]. Verbal as well as tangible rewards can be useful, particularly for adults. Rewards can come from either the professional team or from the patients themselves. For example, self-rewards can be monetary or social and should be encouraged.
- Cognitive restructuring—Unrealistic goals and inaccurate beliefs about weight loss and body image need to be modified to help change self-defeating thoughts and feelings that undermine weight loss efforts. Rational responses designed to replace negative thoughts are encouraged [580]. For example, the thought, “I blew my diet this morning by eating that doughnut; I may as well eat what I like for the rest of the day,” could be replaced by a more adaptive thought, such as, “Well, I ate the doughnut this morning, but I can still eat in a healthy manner at lunch and dinner.”
- Social support—A strong system of social support can facilitate weight reduction. Family members, friends, or colleagues can assist an individual in maintaining motivation and providing positive reinforcement. Some patients may benefit by entering a weight reduction support group. Overweight patients should be asked about (possibly) overweight children and family weight control strategies. Parents and children should work together to engage in and maintain healthy dietary and physical activity habits.
3.b. Treatment of Obese Individuals with Binge Eating Disorder
If a patient suffers from binge eating disorder (BED), consideration can be given to referring the patient to a health professional who specializes in BED treatment. Behavioral approaches to BED associated with obesity have been derived from cognitive behavior therapy (CBT) used to treat bulimia nervosa [227]. Among the techniques are self-monitoring of eating patterns, encouraging regular patterns of eating (three meals a day plus planned snacks), cognitive restructuring, and relapse prevention strategies [581].
RECOMMENDATION
Behavior therapy strategies to promote diet and physical activity should be used routinely, as they are helpful in achieving weight loss and weight maintenance. Evidence Category B.
4. Combined Therapy
To achieve the greatest likelihood of success from weight loss therapy, the combination of dietary therapy with an LCD, increased physical activity, and behavior therapy will be required. Inclusion of behavior therapy and increased physical activity in a weight loss regimen will provide the best opportunity for weight loss, and hopefully for long-term weight control. In order to achieve weight loss, such a regimen should be maintained for at least 6 months before considering pharmacotherapy.
Evidence Statement
Combined intervention of an LCD, increased physical activity, and behavior therapy provides the most successful therapy for weight loss and weight maintenance. Evidence Category A.
Rationale: Clinical trials have demonstrated that combining behavior therapy, LCDs, and increased physical activity provides better outcomes for long-term weight reduction than programs that use only one or two of these modalities. A lower-fat diet markedly improves the potential of physical activity to achieve a negative energy balance [317, 369, 434, 444, 582]. In addition, lower-fat diets that are also low in saturated fats reduce serum cholesterol levels, which would reduce CVD risk. It is difficult to achieve a negative energy balance and weight loss with physical activity of moderate duration and intensity in individuals who consume a high-fat diet and alcohol [583, 584].
RECOMMENDATION
Weight loss and weight maintenance therapy should employ the combination of LCDs, increased physical activity, and behavior therapy. Evidence Category A.
5. Pharmacotherapy
Drug therapy has undergone radical changes in the last 2 years. With the publication of the trials with phentermine and fenfluramine by Weintraub in 1992 (210 weeks), drug therapy began to change from short-term to long-term use. Both dexfenfluramine and fenfluramine alone, as well as the combination of phentermine/fenfluramine, were used long term. However, concerns about recently reported unacceptable side effects, such as valvular lesions of the heart causing significant insufficiency of the valves [658], have led to the withdrawal of the drugs dexfenfluramine and fenfluramine from the market in September 1997 [761]. No drugs remained that were approved by the Food and Drug Administration (FDA) for use longer than 3 months. In November 1997, the FDA approved a new drug, sibutramine, for use in obesity and is in the process of evaluating orlistat for long-term use.
Evidence Statement
Appropriate weight loss drugs can augment diet, physical activity, and behavior therapy in weight loss. Evidence Category B.
Rationale: The purpose of weight loss and weight maintenance is to reduce health risks. If weight is regained, health risks increase once more. The majority of persons who lose weight regain it [585], so the challenge to the patient and the practitioner is to maintain the weight loss. Because of the tendency to regain weight after weight loss, the use of long-term medication to aid in the treatment of obesity may be indicated in carefully selected patients.
The drugs used to promote weight loss have been anorexiants or appetite suppressants. Three classes of anorexiant drugs have been developed, all of which affect neurotransmitters in the brain: those that affect catecholamines, those that affect serotonin, and those that affect both. They work by increasing the secretion of dopamine, norepinephrine, or serotonin into the synaptic neural cleft, or by inhibiting the reuptake of these neurotransmitters back into the neuron, or by both mechanisms. The new agent sibutramine has norepinephrine and serotonin effects. Another new agent, orlistat, has a different mechanism of action, the blockage of fat absorption. Very few trials longer than 6 months have been done with any drug. The ones tested for at least 1 year that received FDA approval for long-term use are shown in Table IV-6.
These drugs are effective but modest in their ability to produce weight loss. Net weight loss attributable to drugs generally has been reported to be in the range of 2 to 10 kg (4.4 to 22 lb), although some patients lose significantly more weight. It is not possible to predict how much weight an individual may lose. Most of the weight loss usually occurs in the first 6 months of therapy.
Adverse effects include primary pulmonary hypertension with fenfluramine and dexfenfluramine [395, 586, 587], valvular heart disease with dexfenfluramine and fenfluramine [658], and increases in blood pressure and pulse with sibutramine [510]. With orlistat, there is a possible decrease in the absorption of fat-soluble vitamins; overcoming this may require vitamin supplementation. People with a history of high blood pressure, CHD, congestive heart failure, arrhythmias, or history of stroke should not take sibutramine, and all patients taking the medication should have their blood pressure monitored on a regular basis. Depression has been described with the serotonergic drugs but it is generally not clinically significant. Neurotoxic effects with neuronal atrophy have been described with high doses of dexfenfluramine in rats and primates, but not in humans [588]. The risks for using appetite suppressant drugs during pregnancy is unknown.
Evidence Statement
Weight loss drugs approved by the FDA for long-term use may be useful as an adjunct to diet and physical activity for patients with a BMI of ≥ 30 with no concomitant obesity-related risk factors or diseases, and for patients with a BMI of ≥ 27 with concomitant obesity-related risk factors or diseases. Evidence Category B.
Rationale: If after at least 6 months on a weight loss regimen of an LCD, increased physical activity, and behavior therapy, the patient has not lost the recommended 1 lb/week, careful consideration may be given to pharmacotherapy. There are few long-term studies evaluating the safety or effectiveness of many currently approved weight loss medications. At present, sibutramine is available for long-term use. (Note: FDA approval for orlistat is pending a resolution of labeling issues and results of Phase III trials.) Their risk/benefit ratio is such that they can be recommended for use with the degree of obesity outlined above [589]. Weight loss medications should be used only by patients who are at increased medical risk because of their weight and should not be used for “cosmetic” weight loss. The risk factors and diseases considered serious enough to warrant pharmacotherapy at BMI of 27 to 29.9 are hypertension, dyslipidemia, CHD, type 2 diabetes, and sleep apnea.
Not every patient responds to drug therapy. Tests with weight loss drugs have shown that initial responders tend to continue to respond, while initial nonresponders are less likely to respond even with an increase in dosage [395, 507]. If a patient does not lose 2 kg (4.4 lb) in the first 4 weeks after initiating therapy, the likelihood of long-term response is very low [507]. This finding may be used as a guide to treatment, either continuing medication in the responders or stopping it in the nonresponders. If weight is lost in the initial 6 months of therapy or is maintained after the initial weight loss phase, this should be considered a success, and the drug may be continued. It is important to remember that the major role of medications should be to help patients stay on a diet and physical activity plan while losing weight. Medication cannot be expected to continue to be effective in weight loss or weight maintenance once it has been stopped [590, 591]. The use of the drug may be continued as long as it is effective and the adverse effects are manageable and not serious. There are no indications for specifying how long a weight loss drug should be continued. Therefore, an initial trial period of several weeks with a given drug or combination of drugs may help determine their efficacy in a given patient. If a patient does not respond to a drug with reasonable weight loss, the physician should reassess the patient to determine adherence to the medication regimen and adjunctive therapies, or consider the need for dosage adjustment. If the patient continues to be unresponsive to the medication, or serious adverse effects occur, the physician should consider its discontinuation [592].
Evidence Statement
Adverse side effects from the use of weight loss drugs have been observed in patients. Evidence Category A.
Rationale: The potential for side effects from the use of weight loss drugs is of great concern. Adverse effects with sibutramine include increased blood pressure and tachycardia [590]. With orlistat there are oily and loose stools and some fat-soluble vitamin malabsorption [389]. Thus, a multivitamin supplement is recommended. Side effects are generally mild and may improve with continued use, although their persistence may result in discontinuation of the drug.
There is a great interest in weight loss drugs among consumers. Because of the possibility of serious adverse effects, it is incumbent on the practitioner to use drug therapy with caution. Practitioners should be sure that patients are not taking drugs that have been withdrawn from the market for safety reasons, and herbal medications are not recommended as part of a weight loss program. These preparations have unpredictable amounts of active ingredients and unpredictable and potentially harmful effects. In those patients with a lower level of obesity risk, nonpharmacological therapy is the treatment of choice. It is important for the physician to monitor both the effectiveness and the side effects of the drug.
Evidence Statement
Using weight loss drugs singly (not in combination) and starting with the lowest effective doses can decrease the likelihood of adverse effects. Evidence Category C.
Rationale: Given the fact that adverse events may increase in association with combination drug therapy, it seems wise that, until further safety data are available, using weight loss drugs singly would be more prudent. Some patients will respond to lower doses, so that full dosage is not always necessary. The short-term use of drugs (< 3 months) has not generally been found to be effective.
Drugs should be used only as part of a comprehensive program that includes behavior therapy, diet, and physical activity. Appropriate monitoring for side effects must be continued while drugs are part of the regimen. Patients will need to return for followup in 2 to 4 weeks, then monthly for 3 months, and then every 3 months for the first year after starting the medication. After the first year, the doctor will advise the patient on appropriate return visits. The purposes of these visits are to monitor weight, blood pressure, and pulse, discuss side effects, conduct laboratory tests, and answer questions.
Since obesity is a chronic disorder, the short-term use of drugs is not helpful. The health professional should include drugs only in the context of a long-term treatment strategy [593]. The risk/benefit ratio cannot be predicted at this time, since not enough long-term data (> 1 year) are available on any of the available drugs.
RECOMMENDATION
Weight loss drugs approved by the FDA may only be used as part of a comprehensive weight loss program, including dietary therapy and physical activity, for patients with a BMI of ≥ 30 with no concomitant obesity-related risk factors or diseases, and for patients with a BMI of ≥ 27 with concomitant obesity-related risk factors or diseases. Weight loss drugs should never be used without concomitant lifestyle modifications. Continual assessment of drug therapy for efficacy and safety is necessary. If the drug is efficacious in helping the patient lose and/or maintain weight loss and there are no serious adverse effects, it can be continued. If not, it should be discontinued. Evidence Category B.
6. Surgery for Weight Loss
Surgery is one option for weight reduction for some patients with severe and resistant obesity. The aim of surgery is to modify the gastrointestinal tract to reduce net food intake. Most authorities agree that weight loss surgery should be reserved for patients with severe obesity, in whom efforts at other therapy have failed, and who are suffering from the complications of obesity.
Considerable progress has been made in developing safer and more effective surgical procedures for promoting weight loss. Surgical interventions commonly used include gastroplasty, gastric partitioning, and gastric bypass. These procedures are designed primarily to reduce food consumption. They have replaced previous procedures that were designed to promote malabsorption of nutrients. The latter procedures were fraught with side effects that made their use impractical or dangerous.
Evidence Statement
Gastrointestinal surgery (gastric restriction [vertical gastric banding] or gastric bypass [Roux-en Y]) can result in substantial weight loss, and therefore is an available weight loss option for well-informed and motivated patients with a BMI ≥ 40 or ≥ 35, who have comorbid conditions and acceptable operative risks. Evidence Category B.
Rationale: According to the National Institutes of Health's Consensus Development Conference on Gastrointestinal Surgery for Severe Obesity [523], the risk for morbidity and mortality accompanying obesity increases with the degree of overweight. Thus, treatment of clinically severe obesity involves an effort to create a caloric deficit sufficient to result in weight loss and reduction of weight-associated risk factors or comorbidities. Surgical approaches can result in substantial weight loss, i.e., from 50 kg (110 lb) to as much as 100 kg (220 lb) over a period of 6 months to 1 year. A major limitation of nonsurgical approaches is the failure to maintain reduced body weight in many individuals.
Surgical procedures in current use (gastric restriction [vertical gastric banding] and gastric bypass [Roux-en Y]) can induce substantial weight loss, and serve to reduce weight-associated risk factors and comorbidities. Compared to other interventions available, surgery has produced the longest period of sustained weight loss. Assessing both perioperative risk and long-term complications is important and requires assessing the risk/benefit ratio in each case. Patients whose BMI equals or exceeds 40 kg/m2 are potential candidates for surgery if they strongly desire substantial weight loss, because obesity severely impairs the quality of their lives. Less severe obese patients (BMIs between 35 and 39.9 kg/m2) also may be considered for surgery. This group primarily includes those patients with high-risk comorbid conditions (cardiovascular, sleep apnea, uncontrolled type 2 diabetes) or weight-induced physical problems interfering with performance of daily life activities.
A recent retrospective study of severely overweight patients with noninsulin-dependent diabetes, who were referred for consideration of a gastric bypass procedure, allowed for a comparison of those who opted for the surgical procedure versus those who did not undergo the procedure because of personal preference or refusal of insurance payment. Patients undergoing the surgical procedure had a decrease in mortality rate for each year of follow up [594]. This latter observation provides initial documentation of the significant impact that reduction in weight may have on mortality.
Most of the surgery studies primarily included women of childbearing age. Caution should be exercised in selecting candidates for surgery to treat obesity, as pregnancy demands increase nutritional needs and a normal need for weight gain. Women with reproductive potential should be advised to avoid pregnancy until their weight has stabilized postoperatively and potential micronutrient deficiencies have been identified and treated.
Of special note is that many of the studies reported to date have not had population samples representative of the general severely overweight population with respect to race, ethnicity, cultural or socioeconomic background, or gender.
Evidence Statement
Patients opting for surgical intervention should be followed by a multidisciplinary team (medical, behavioral, and nutritional). Evidence Category D.
Rationale: As for all other interventions for obesity, an integrated program should be in place that will provide guidance concerning the necessary dietary regimen, appropriate physical activity, and behavioral and social support both prior to and after the surgical procedure.
Evidence Statement
Lifelong medical surveillance after surgical therapy is a necessity. Evidence Category C.
Rationale: Since surgical procedures result in some loss of absorptive function, the long-term consequences of potential nutrient deficiencies must be recognized and adequate monitoring must be performed, particularly with regard to vitamin B12, folate, and iron. Some patients may develop other gastrointestinal symptoms such as “dumping syndrome” or gallstones. Occasionally, patients may have postoperative mood changes or their presurgical depression symptoms may not be improved by the achieved weight loss. Thus, surveillance should include monitoring of indices of inadequate nutrition and modification of any preoperative disorders. Table IV-7 illustrates some of the complications that can occur following gastric bypass surgery.
RECOMMENDATION
Weight loss surgery is an option for carefully selected patients with clinically severe obesity (BMI ≥ 40 or ≥ 35 with comorbid conditions) when less invasive methods of weight loss have failed and the patient is at high risk for obesity-associated morbidity or mortality. Evidence Category B.
COMMENTARY: Adapting Weight Loss Programs To Meet the Needs of Diverse Patient Populations
Standard obesity treatment approaches should be tailored to the needs of patients. It is, however, difficult to determine from the literature how often this occurs and whether it makes weight loss programs more effective. Very few published reports of such adapted programs can be identified, particularly when a distinction is made from reports that include or focus on special populations but do not report any particular steps taken to modify the intervention for these populations. In addition, it is impossible to compare directly the amount of weight lost using specially adapted programs with that achieved when more standard approaches are used. Studies reporting these programs are sometimes pilot studies or descriptive reports that do not meet the standards of evidence set forth elsewhere in these guidelines. Where randomized controlled trials or quasi-experiments are available, they usually do not include an internal comparison with a program involving no adaptations. Appendix III illustrates the types of adaptations that have been reported.
Large individual variation exists within any social or cultural group; furthermore, there is substantial overlap among subcultures within the larger society. There is, therefore, no “cookbook” or standardized set of rules to optimize weight reduction with a given type of patient. A theoretical and qualitative analysis of cultural appropriateness in obesity treatment programs has been conducted, and it provides some guidance for incorporating patient characteristics and perspectives when designing and delivering weight loss programs [257]. Some examples follow:
- Adapt the setting and staffing to the patient population. The setting should:
- be physically accessible to the patient;
- have features likely to be familiar to the patient;
- be free of negative psychosocial connotations;
- be devoid of aspects that create a large social distance among patients or between patient and practitioner; and
- promote active patient participation and high patient self-esteem and self-efficacy.The staff should be culturally self-aware and culturally competent in working with persons of diverse cultural backgrounds and income or educational levels. For that community centers may be preferable to hospitals or medical offices as venues for conducting lifestyle weight reduction programs. Or, some programs have included peer educators as a possible way of helping to overcome background and social class differences by providing a bridge of knowledge, experience, and perspective between patients and practitioners (see Appendix III).
- List assumptions about the type of patient for whom the program will be best suited and evaluate the extent to which these assumptions are appropriate for prospective patients. Where appropriate, modify the program to avoid the need for certain assumptions. Consider patients'—
- preexisting knowledge base;
- day-to-day routine;
- discretionary time;
- financial resources and living situation; and
- cultural preferences for types of food and activity.For example, redesign printed materials to be suitable for patients with low literacy skills or poor vision. Offer dietary and physical activity recommendations that will be feasible for low-income patients living in inner-city areas with limited access to supermarkets or with high crime rates.
- Consider how the obesity treatment program fits in other aspects of the health care and self-care of the patient(s), and integrate other aspects where appropriate. For example, for those patients with diabetes, information about weight reduction should be aligned with other diabetes management advice.
- Expect and allow for program modifications based on patient feedback and preferences. Program appropriateness can be increased when patients can express their needs and preferences, and the program is then adapted to those needs and preferences. This is especially applicable when practitioners have limited common experience with patients.
In recent years, a fat acceptance, nondieting advocacy group has developed. This has emerged from concerns about weight cycling and its possible adverse effects on morbidity and mortality. However, recent evidence suggests that intentional weight loss is not associated with increased morbidity and mortality. For this reason, the guidelines have been made explicit on the importance of intervention for weight loss and maintenance in the appropriate patient groups.
COMMENTARY: Weight Reduction After Age 65—What Are the Issues?
- Are the indications for treating obesity in older adults the same as those for younger adults?
- Does weight loss reduce risk factors in older adults?
- Does weight reduction prolong the lives of older adults?
- Are there risks associated with obesity treatment that are unique to older adults?
The higher prevalence of cardiovascular risk factors in overweight versus nonoverweight persons is clearly observed at older ages [596, 597]. In addition, obesity is a major predictor of functional limitations and mobility impairments in older adults [596, 598–600]. Both observational data [596] and applicable randomized controlled trials cited in these guidelines suggest that weight loss reduces risk factors and improves functional status in older persons in the same manner as in younger adults.
The question of whether weight reduction leads to increased survival among older adults has been raised because of observations that weight reduction after age 60 or 65 years may be unable to reverse the deleterious effects of longstanding obesity [288, 596, 601, 602]. Also, weight loss at older ages has been associated with increased mortality [318, 603–607]. Some of the association of weight loss with higher mortality may be due to the increased frequency at older ages of involuntary weight loss due to identified or occult illness. In any case, the association of weight loss with higher mortality applies most clearly to individuals who enter old age with a BMI in the lower part of the range. It is not clear that it applies to overweight older persons with CVD risk factors. This issue has been difficult to clarify in observational data, but there are no randomized trials in which the effects of obesity treatment on mortality can be directly assessed, at any age.
The wisdom or importance of treating obesity at older ages has also been questioned because of epidemiological observations suggesting a decreased significance of obesity-related relative risks at older ages (see chapter 2.3.b.). However, these relative-risk data are not a useful reference point for considering whether obese older persons will benefit. Relative risks are influenced by the characteristics of the comparison group. In this case, the comparison group is lower-weight older persons who have also had high morbidity and mortality.
Concerns about potential adverse effects of obesity treatment in older adults have been raised with respect to bone health and to dietary adequacy. Weight reduction may accelerate aging-related bone loss and thereby increase the risk of osteoporotic fractures in high-risk groups such as older white women [608–610]. This concern is more relevant to weight loss in thin persons than in obese persons. Some evidence suggests that including resistance training and moderate weight-bearing exercise as a part of a weight reduction program may help maintain bone integrity [611, 612].
The general nutritional safety of weight reduction at older ages is of interest because restrictions on overall food intake due to dieting could result in inadequate intakes of protein or essential vitamins and minerals. In addition, involuntary weight loss indicative of occult disease might be mistaken for success in voluntary weight reduction. These concerns can be alleviated by providing proper nutritional counseling and regular body weight monitoring for older persons for whom weight reduction is prescribed.
Evidence Statement
Age alone should not preclude treatment for obesity in adult men and women. Evidence Category D.
Rationale: There is little evidence at present to indicate that obesity treatment should be withheld from adult men and women on the basis of age alone up to 80 years of age.
RECOMMENDATION
A clinical decision to forego obesity treatment in an older adult should be guided by an evaluation of the potential benefits of weight reduction for day-to-day functioning and reduction of the risk of future cardiovascular events, as well as the patient's motivation for weight reduction. Care must be taken to ensure that any weight reduction program minimizes the likelihood of adverse effects on bone health or other aspects of nutritional status. Evidence Category D.
I. Smoking Cessation in the Overweight or Obese Patient
Cigarette smoking is a major risk factor for cardiopulmonary disease. Because of its attendant high risk, smoking cessation is a major goal of risk-factor management. This aim is especially important in the overweight or obese patient, who usually carries excess risk from obesity-associated risk factors. Thus, smoking cessation in such patients becomes a high priority for risk reduction.
Evidence Statement
Smoking and obesity together increase cardiovascular risk, but fear of weight gain upon smoking cessation is an obstacle for many patients who smoke. Evidence Category C.
Rationale: Both smoking and obesity are accompanied by increased risks for cardiovascular disease. Many well-documented health benefits are associated with smoking cessation, but a major obstacle to successful smoking cessation has been the attendant weight gain observed in about 80 percent of quitters. This weight gain averages 4.5 to 7 lb, but in 13 percent of women and 10 percent of men, weight gains in excess of 28 lb have been noted among quitters [613–615]. Weight gain is an important barrier to smoking cessation, particularly in women [616, 617].
Weight gain that accompanies smoking cessation so far has been relatively resistant to most dietary, behavioral, or physical activity interventions [618, 619]. Postcessation weight gain has been associated with a reduction in energy expenditure of up to 100 kcal/day, accounting for approximately one-third of the weight gain after smoking cessation [620, 621]. The reduction in energy expenditure appears to be the result of a decrease in the resting metabolic rate [614]. In general, no differences in the level of physical activity have been observed after smoking cessation. About two-thirds of the weight gain after smoking cessation appears to result from increased caloric intake [621–623]. However, dietary counseling programs combined with smoking cessation programs have not been very successful. There are several products that reduce postcessation weight gain during drug administration, including nicotine replacement therapy [624], phenylpropanol-amine [625], and bupropion [626]. No matter what the drug, however, it appears that these drugs merely delay rather than prevent postcessation weight gain. That is, while providing weight gain suppression during drug administration, subjects on these drugs experience a rebound of weight gain once they go off the products and long-term weight gain is equal to that in those not receiving these drugs [624, 626].
The weight gained with smoking cessation is less likely to produce negative health consequences than would continued smoking. For this reason, smoking cessation should be strongly reinforced in persons regardless of their baseline weight. Smoking is not an acceptable weight control therapy, although it seems to be used for this purpose by a great many people. Overweight patients, as well as all others, should be counseled to quit smoking. For practical reasons, it may be prudent to avoid initiating smoking cessation and weight loss therapy simutaneously. Prevention of weight gain through diet and physical activity should be stressed. If weight gain ensues after smoking cessation, it should be managed vigorously according to the guidelines outlined in this report. Although short-term weight gain is a common side effect of smoking cessation, this gain does not rule out the possibility of long-term weight control. There are no clinical trials to test whether ex-smokers are less likely to successfully achieve long-term weight reduction than those who never smoked.
RECOMMENDATION
All smokers, regardless of their weight status, should quit smoking. Evidence Category A. Prevention of weight gain should be encouraged and if weight gain does occur, it should be treated through dietary therapy, physical activity, and behavior therapy, maintaining the primary emphasis on the abstinence from smoking. Evidence Category C.
J. Role of Health Professionals in Weight Loss Therapy
Evidence Statement
A number of health professionals can play an important role in a weight loss and management program. Evidence Category B.
Rationale: Various randomized controlled trials were reviewed that highlighted the role of the nutritionists [413, 476], exercise physiologists and physical education instructors [401, 447], nurses [413], and psychologists [476, 487] in addition to the physician in providing assessment, treatment, and follow up during weight loss. As a result, it is suggested that the health professionals avail themselves of the various disciplines that offer expertise in dietary counseling, physical activity, and behavior change. The relationship between the physician and these disciplines can be a direct, formal one or a more indirect referral. It is important to emphasize that a positive attitude of support and encouragement from all professionals is crucial to continuing success [627].
RECOMMENDATION
A weight loss and maintenance program can be conducted by a practitioner without specialization in weight loss so long as that person has the requisite interest and knowledge. However, various health professionals with different expertise are available and helpful to a practitioner who would like assistance. Evidence Category B.
Figures
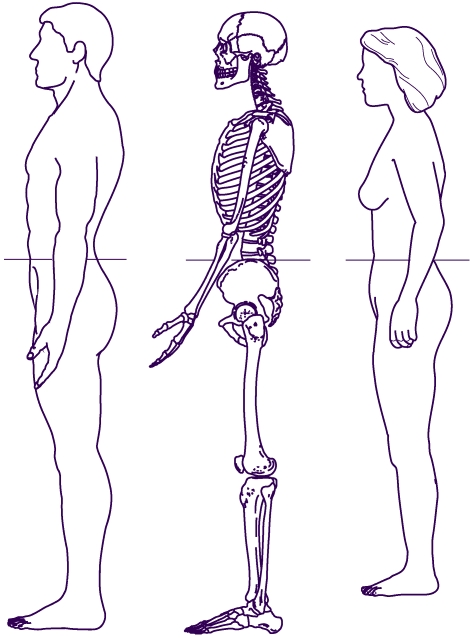
Figure 5
Measuring tape position for waist (abdominal) circumference

Figure 6
Treatment Algorithm*
Tables
Table IV-1Classification of Overweight and Obesity by BMI*
| Obesity Class | BMI (kg/m2) | |
|---|---|---|
| Underweight | < 18.5 | |
| Normal | 18.5 – 24.9 | |
| Overweight | 25.0 – 29.9 | |
| Obesity | I | 30.0 – 34.9 |
| II | 35.0 – 39.9 | |
| Extreme Obesity | III | ≥ 40 |
Source (adapted from): Preventing and Managing the Global Epidemic of Obesity. Report of the World Health Organization Consultation of Obesity. WHO, Geneva, June 1997 [65].
Table IV-2Classification of Overweight and Obesity by BMI, Waist Circumference and Associated Disease Risk*
| Disease Risk* Relative to Normal Weight and Waist Circumference | ||||
|---|---|---|---|---|
| BMI (kg/m2) | Obesity Class | Men ≤102 cm (≤40 in) | >102 cm (>40 in) | |
| Women ≤88 cm (≤35 in) | >88 cm (>35 in) | |||
| Underweight | <18.5 | — | — | |
| Normal+ | 18.5 – 24.9 | — | — | |
| Overweight | 25.0 – 29.9 | Increased | High | |
| Obesity | 30.0 – 34.9 | I | High | Very High |
| 35.0 – 39.9 | II | Very High | Very High | |
| Extreme Obesity | ≥40 | III | Extremely High | Extremely High |
- *
Disease risk for type 2 diabetes, hypertension, and CVD.
- +
Increased waist circumference can also be a marker for increased risk even in persons of normal weight.
Source (adapted from): Preventing and Managing the Global Epidemic of Obesity. Report of the World Health Organization Consultation of Obesity. WHO, Geneva, June 1997 [65].
Table IV-3Low-Calorie Step I Diet
| Nutrient | Recommended Intake |
|---|---|
| Calories1 | Approximately 500 to 1,000 kcal/day reduction from usual intake |
| Total Fat2 | 30 percent or less of total calories |
| Saturated Fatty Acids3 | 8 to 10 percent of total calories |
| Monounsaturated Fatty Acids | Up to 15 percent of total calories |
| Polyunsaturated Fatty Acids | Up to 10 percent of total calories |
| Cholesterol3 | < 300 mg/day |
| Protein4 | Approximately 15 percent of total calories |
| Carbohydrate5 | 55 percent or more of total calories |
| Sodium Chloride | No more than 100 mmol per day (approximately 2.4 g of sodium or approximately 6 g of sodium chloride) |
| Calcium6 | 1,000 to 1,500 mg |
| Fiber5 | 20 to 30 g |
- 1
A reduction in calories of 500 to1,000 kcal/day will help achieve a weight loss of 1 to 2 lbs/week. Alcohol provides unneeded calories and displaces more nutritious foods. Alcohol consumption not only increases the number of calories in a diet but has been associated with obesity in epidemiological studies [559–562] as well as in experimental studies [563–566]. The impact of alcohol calories on a person's overall caloric intake needs to be assessed and appropriately controlled.
- 2
Fat-modified foods may provide a helpful strategy for lowering total fat intake but will only be effective if they are also low in calories and if there is no compensation of calories from other foods.
- 3
Patients with high blood cholesterol levels may need to use the Step II diet to achieve further reductions in LDL-cholesterol levels; in the Step II diet, saturated fats are reduced to less than 7 percent of total calories, and cholesterol levels to less than 200 mg/day. All of the other nutrients are the same as in Step I.
- 4
Protein should be derived from plant sources and lean sources of animal protein.
- 5
Complex carbohydrates from different vegetables, fruits, and whole grains are good sources of vitamins, minerals, and fiber. A diet rich in soluble fiber, including oat bran, legumes, barley, and most fruits and vegetables may be effective in reducing blood cholesterol levels. A diet high in all types of fiber may also aid in weight management by promoting satiety at lower levels of calorie and fat intake. Some authorities recommend 20 to 30 grams of fiber daily, with an upper limit of 35 grams [546, 567, 568].
- 6
During weight loss, attention should be given to maintaining an adequate intake of vitamins and minerals. Maintenance of the recommended calcium intakes of 1,000 to 1,500 mg/day is especially important for women who may be at risk of osteoporosis [569].
Table IV-4Examples of Moderate Amounts of Activity*

Table IV-5Duration Of Various Activities to Expend 150 Kilocalories For an Average 70 kg (154 lb) Adult
| Intensity | Activity | Approximate duration in minutes |
|---|---|---|
| Moderate | Volleyball, noncompetitive | 43 |
| Moderate | Walking, moderate pace (3mph, 20 min/mile) | 37 |
| Moderate | Walking, brisk pace (4mph, 15 min/mile) | 32 |
| Moderate | Table tennis | 32 |
| Moderate | Raking leaves | 32 |
| Moderate | Social dancing | 29 |
| Moderate | Lawn mowing (powered push mower) | 29 |
| Hard | Jogging (5 mph, 12 min/mile) | 18 |
| Hard | Field hockey | 16 |
| Very Hard | Running (6 mph, 10 min/mile) | 13 |
Source: Surgeon General's Report on Physical Activity and Health
Table IV-6Weight Loss Drugs+
| Drug | Action | Adverse Effects |
|---|---|---|
| dexfenfluramine* | serotonin reuptake inhibitor | valvular heart disease |
| fenfluramine* | serotonin releaser | primary pulmonary hypertension neurotoxicity |
| sibutramine | norepinephrine, dopamine, and serotonin reuptake inhibitor | increase in heart rate and blood pressure |
| orlistat± | inhibits pancreatic lipase, decreases fat absorption | decrease in absorption of fat-soluble vitamins |
| soft stools and anal leakage | ||
| possible link to breast cancer |
- +
Ephedrine and caffeine, and, fluoxetine have also been tested for weight loss, but are not approved for use in the treatment of obesity. Mazindol, phentermine, benzphetamine, and phendimetrazine are approved for only short-term use for the treatment of obesity.
- *
FDA approval withdrawn
- ±
FDA approval pending
Table IV-7Gastric Bypass Surgery Complications: 14-Year Follow Up
| Vitamin B12 deficiency | 239 | 39.9 percent |
| Readmit for various reasons | 229 | 38.2 percent |
| Incisional hernia | 143 | 23.9 percent |
| Depression | 142 | 23.7 percent |
| Staple line failure | 90 | 15.0 percent |
| Gastritis | 79 | 13.2 percent |
| Cholecystitis | 68 | 11.4 percent |
| Anastomotic problems | 59 | 9.8 percent |
| Dehydration, malnutrition | 35 | 5.8 percent |
| Dilated pouch | 19 | 3.2 percent |
Data derived from source (Pories WJ [595]) and modified based on personal communication.