All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: tni.ohw@sredrokoob). Requests for permission to reproduce or translate WHO publications - whether for sale or for noncommercial distribution - should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; email: tni.ohw@snoissimrep).
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Manual for the Health Care of Children in Humanitarian Emergencies. Geneva: World Health Organization; 2008.
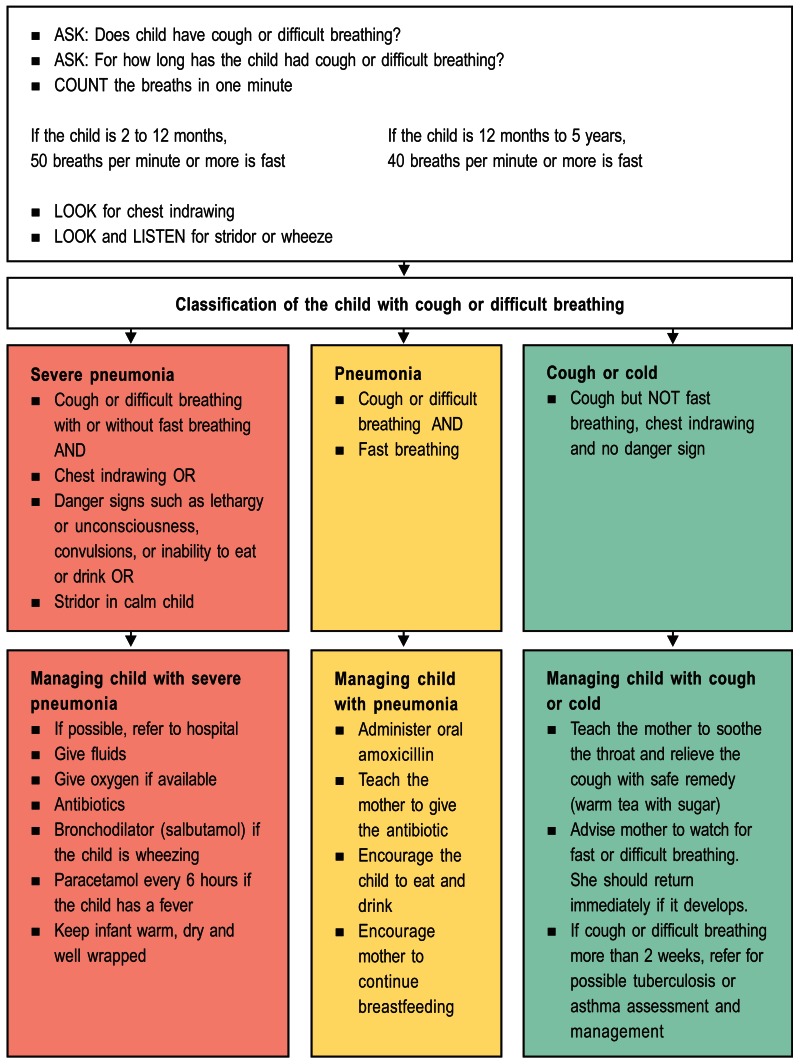
Assessment of the child with cough or difficult breathing
Assess the child for acute respiratory tract infection (cough or difficult breathing)
- ASK: Does the child have cough or difficult breathing?
- ASK: For how long has the child had cough or difficult breathing?
- COUNT the breaths in one minute.
If the child is: The child has fast breathing if you count: 2 months up to 12 months 50 breaths per minute or more 12 months up to 5 years 40 breaths per minute or more. - LOOK for chest indrawing.
- LOOK and LISTEN for stridor or wheeze, a sign of airway obstruction
Chest indrawing is the inward movement of the lower chest wall when the child breathes in, and is a sign of respiratory distress. Chest indrawing does not refer to the inward movement of the soft tissue between the ribs.
Stridor is a harsh noise heard when a sick child breathes in. Stridor is usually caused by a viral infection (croup) which causes swelling in the child's upper airway. Another cause of stridor is diphtheria, a bacterial infection preventable by vaccination. Stridor may also be caused by an object in the upper airway.
Wheeze is a high-pitched whistling sound near the end of expiration. It is caused by narrowing of the small air passages of the lung. To hear a wheeze, place the ear next to the child's mouth and listen to the breathing while the child is calm, or use a stethoscope to listen for wheezes.
Some signs of diphtheria:
- Look at the child's nose and throat very carefully without distressing the child. If there is a grey, adherent membrane which cannot be wiped off with a swab, this is probably diphtheria.
- Look at the child's neck. If it is swollen (“bull neck”) on one side this also suggests diphtheria.
Classify the child with cough or difficult breathing
There are three possible classifications for a child with cough or difficult breathing:
- severe pneumonia
- pneumonia
- cough or cold (without pneumonia)
- Classify the child with SEVERE PNEUMONIA if the child has fast breathing and:
- Classify the child with PNEUMONIA if the child does not have the above signs but the child has:
- Fast breathing.
- Classify the child as having COUGH OR COLD if the child does not have fast breathing but has a cough.
- Child as having CHRONIC COUGH if the child has had:
- Cough for 3 weeks or longer. This child may have tuberculosis or asthma or whooping cough.
Management of the child with cough or difficult breathing
Treat pneumonia
The child with SEVERE PNEUMONIA needs urgent care.
- If possible, refer the child with SEVERE PNEUMONIA to a hospital for care.
- Administer antibiotics for a total of 10 days.
- intramuscular gentamicin and ampicillin or
- intramuscular chloramphenicol or
- intramuscular benzylpenicillin or ampicillin or
- change to oral chloramphenicol when child improves.
- Administer oxygen if possible.
- Give a bronchodilator (salbutamol) if the child is wheezing.
- Give paracetamol every 6 hours if the child has fever (axillary temperature of 38.5°C or above).
- Manage the airway by clearing a blocked nose with a plastic syringe (without the needle) to gently suck secretions from the nose.
- If the child can drink, give fluids by mouth, but cautiously to avoid fluid overload.
- Encourage the mother to continue breastfeeding if the child is not in respiratory distress.
- If the child is too ill to breastfeed but can swallow, have the mother express milk into a cup and slowly feed the child the breast milk with a spoon.
- If the child is not able to drink, either use a dropper to give the child fluid very slowly or drip fluid from a cup or a syringe without a needle. Avoid using a nasogastric (NG) tube if the child is in respiratory distress.
- Keep the infant warm. Keep the sick infant dry and well wrapped. If possible, have the mother keep her infant next to her body, ideally between her breasts. A hat or bonnet will prevent heat loss from the head.
The child with non-severe PNEUMONIA needs antibiotics but can be managed at home.
- Administer an oral antibiotic.
- The preferred treatment is oral amoxicillin (25 mg/kg/dose) 2 times a day for 3 days.
- An alternative treatment is oral chloramphenicol (50 mg/kg) in 3 divided doses per day.
- The duration of treatment should be extended to 5 days in high HIV prevalence settings.
- Show the mother how to give the antibiotic.
- Encourage the child to eat and drink.
- Encourage the mother to continue breastfeeding the child.
- Advise the mother to return with the child immediately if the child's breathing worsens or the child develops any danger sign.
- Follow up in 2 days.
The child with COUGH or COLD (no pneumonia) does not need antibiotics.
- Teach the mother to soothe the throat and relieve the cough with a safe remedy such as warm tea with sugar.
- Advise the mother to watch for fast or difficult breathing and to return if either one develops.
- Follow up in 5 days if there is no improvement.
Treat wheezing
Give inhaled bronchodilator using a spacer.
- A spacer is a way of delivering the bronchodilator drugs effectively into the lungs. No child under 5 years should be given an inhaler without a spacer. A spacer works as well as a nebuliser if correctly used.
- From salbutamol metered dose inhaler (100ug/puff) give 2 puffs.
- Repeat up to 3 times every 15 minutes before classifying pneumonia.
Spacers can be made in the following way:
- Use a 500ml drink bottle or similar.
- Cut a hole in the bottle base in the same shape as the mouthpiece of the inhaler. This can be done using a sharp knife.
- Cut the bottle between the upper quarter and the lower 3/4 and discard the upper quarter of the bottle.
- Cut a small V in the border of the large open part of the bottle to fit to the child's nose and be used as a mask.
- Flame the edge of the cut bottle with a candle or a lighter to soften it.
In a small baby, a mask can be made by making a similar hole in a plastic (not polystyrene) cup. Alternatively commercial spacers can be used if available.
To use an inhaler with a spacer:
- Remove the inhaler cap. Shake the inhaler well.
- Insert mouthpiece of the inhaler through the hole in the bottle or plastic cup.
- The child should put the opening of the bottle into his mouth and breathe in and out through the mouth.
- A carer then presses down the inhaler and sprays into the bottle while the child continues to breathe normally.
- Wait for three to four breaths and repeat for total of five sprays.
- For younger children place the cup over the child's mouth and use as a spacer in the same way.
N.B. If a spacer is being used for the first time, it should be primed by 4-5 extra puffs from the inhaler.
Treat stridor
- Give oxygen if possible
- Give one dose of oral corticosteroid
- If diphtheria: give procaine penicillin and diphtheria antitoxin IM
Treat STRIDOR as severe:
- If stridor is present when the child is breathing quietly (not crying)
- Give oxygen using nasal prongs if possible. Continue oxygen therapy until the lower chest wall indrawing is no longer present.
- Steroid treatment: give one dose of oral dexamethasone (0.6 mg/kg).
- If the child has severe chest indrawing, refer the child.
If DIPHTHERIA is the cause of stridor:
- Give IM procaine penicillin (50 000 units/kg) daily for 7 days.
- Give 40 000 units of diphtheria antitoxin IM immediately. As there is risk for a serious allergic reaction, an initial intradermal test should be done to check for hypersensitivity.
- If the child is in severe distress, consider referral if possible as the child might need a tracheotomy (a hole in the front of the neck into the windpipe to allow air entry to lungs).
- Check on the child every few hours. Anyone caring for the child should have been immunized against diphtheria.
- Give all unimmunized household contacts of the child one IM dose of benzathine penicillin (600 000 units if 5 years or younger; 1 200 000 units to persons over age 5 years) and immunize them with diphtheria toxoid.
- Give all immunized household contacts a diphtheria toxoid booster.
- A child who has had diphtheria may have complications of the heart (myocarditis) or paralysis 2–7 weeks after the initial infection.
- Manage the child as MILD STRIDOR if child has a hoarse voice and stridor is only heard when the child is agitated or crying. Manage child at home with supportive care, encouraging oral fluids, breastfeeding or feeding. Give paracetamol if child has a fever. Advise the mother to return immediately with the child if the child's breathing worsens or the child develops any danger sign.
Treat the child with cough or difficult breathing for more than 2 weeks
The child with COUGH for more than 2 weeks needs evaluation for possible asthma or tuberculosis.
Managing the child with cough for more than 2 weeks:
- Evaluate for asthma and TB
- Give first-line antibiotic for pneumonia for 5 days if child was not recently treated with antibiotics for pneumonia
- Give salbutamol for 14 days if child is wheezing or coughing at night
- Weigh child to assess for weight loss
- Ask about TB or chronic cough in the family
- See the child in 2 weeks
- If there is no response to above treatment or child is losing weight, obtain an X-ray of the chest to check for signs of TB.
- If an X-Ray is not available, a clinician can make the decision to begin treatment for TB based on high index of suspicion (see below)
Approach to diagnosis of TB in children:
- The commonest type of TB in children is extrapulmonary TB, mainly intrathoracic. Other forms include TB lymphadenopathy, TB meningitis, TB effusions (pleural, pericardial, peritoneal) and spinal TB.
- The diagnosis of pulmonary TB in children is difficult. Most children with pulmonary TB are too young to produce sputum for smear microscopy.
- Important features of pulmonary TB include:
- Contact with a smear-positive pulmonary case;
- Respiratory symptoms for more than 2 weeks, not responding to broad-spectrum antibiotics;
- Weight loss or failure to thrive especially when not response to therapeutic feeding programme.
- Positive test to the standard dose of tuberculin (2 units tuberculin (TU) or RT23 or 5 TU of PPD-S: 10 mm or more in unvaccinated children, 15mm or more in BCG-vaccinated children. However, with severe TB and/or advanced immunosuppression, the TST may be negative.
- Chest X-ray findings are often not specific, however become more valuable if there has been a history of close contact with a diagnosed pulmonary TB case.
- Cough or difficult breathing - Manual for the Health Care of Children in Humanit...Cough or difficult breathing - Manual for the Health Care of Children in Humanitarian Emergencies
Your browsing activity is empty.
Activity recording is turned off.
See more...