NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Propofol is the mostly commonly used parenteral anesthetic agent in the United States, extensively used for minor and outpatient surgical procedures because of its rapid onset and reversal of action, and in intensive care units (ICUs) for maintenance of coma. Propofol has been associated with rare instances of idiosyncratic acute liver injury; in addition, prolonged high dose propofol therapy can cause the “Propofol infusion syndrome” which is marked by bradyarrhythmias, metabolic acidosis, rhabdomyolysis, hyperlipidemia and an enlarged or fatty liver.
Background
Propofol (proe' poe fol) is an intravenously administered anesthetic agent that is widely used for minor and outpatient surgical procedures. Chemically, propofol is 2,6-diisopropylphenol and its mechanism of action is similar to the barbiturates and benzodiazepines, binding to gamma amino butyric acid (GABA) receptors in the central nervous system. The binding is to a different site than the benzodiazepines and causes marked increases the neuroinhibitory actions of the GABA receptor resulting in increased chloride conduction and hyperpolarization of neurons. Propofol also lowers intracerebral pressure and reduces cerebral oxygen consumption. Importantly, propofol has the unique pharmacokinetic and pharmacodynamic features of rapid onset of action and rapid reversal with stopping which makes it a valuable agent for induction of anesthesia and for short-term procedures. Propofol was approved for use in the United States in 1989 and it has become widely used for induction of general anesthesia, as an sole anesthetic agent for short, minor surgical and endoscopic procedures, and as a means of prolonged sedation in critically ill patients in intensive care units. Propofol is highly insoluble in water and is given in a lipid emulsion usually in a 1% solution of 10% soy bean oil. The typical induction dose of propofol is 1.5 to 2.5 mg/kg followed with small boluses or a constant low dose infusion for maintenance of anesthesia. Propofol is available generically and under the brand name Diprivan. Propofol should be administered by a trained anesthesiologist or anesthetist with adequate availability of ventilatory and cardiac support. Deaths from propofol overdose have been reported, particularly with its abuse.
Hepatotoxicity
Liver test abnormalities are not common among patients during or after propofol anesthesia when given for a few hours. Indeed, propofol can be used safely in patients with cirrhosis and may be the preferred anesthetic agent in patients with minimal hepatic encephalopathy. However, isolated case reports of hepatitis arising within days or weeks after propofol anesthesia for minor procedures have been published. The pattern of serum enzyme elevations was usually hepatocellular and some instances were accompanied by jaundice and prolongation of prothrombin time activity (Case 1). Immunoallergic features and autoantibodies during the liver injury were absent. In most published instances, other diagnoses such as ischemic hepatitis and hepatitis C were not completely excluded.
Prolonged infusions of propofol can result in a distinctive clinical syndrome known as the propofol infusion syndrome. It is marked by combinations of cardiac bradyarrhythmias, metabolic acidosis, rhabdomyolysis, hyperlipidemia, renal insufficiency and death from cardiovascular collapse. The syndrome generally arises after 2 to 3 days of sedation in association with use of higher doses of propofol (>5 mg/kg/hour) and may be more common in children than adults. Early termination of the propofol infusion can result in reversal of the syndrome, but the mortality rate in published series has been greater than 50%. On autopsy, patients with the propofol infusion syndrome may have hepatic microvesicular steatosis, explaining the lactic acidosis that frequently accompanies the muscle and heart abnormalities. However, jaundice and marked elevations in typical liver associated enzymes in this syndrome are uncommon. In some instances, both the urine and the liver have been described as being green in color, returning to normal soon after propofol is stopped. A mild form of this syndrome may occur earlier during infusions, as shown by lactic acidosis arising within 2 to 24 hours of starting propofol which is rapidly reversed upon stopping. More than 50 instances of propofol infusion syndrome have been described in the literature with a high mortality rate, although most deaths were due to cardiac involvement. Some instances of propofol infusion syndrome and lactic acidosis have been associated with higher than expected plasma levels of propofol, perhaps due to idiosyncratic differences in pharmacokinetics or miscalculation of administered dose.
Likelihood score: A[H] (well established cause of fatty liver injury when given in high doses over several days as a part of the propofol infusion syndrome) and D (possible rare cause of idiosyncratic, clinically apparent liver injury when given short term in conventional doses).
Mechanism of Injury
The mechanism by which propofol causes liver injury is not known. The idiosyncratic cases are likely due to a metabolic byproduct as propofol is extensive metabolized in the liver by multiple P450 isoforms. The propofol infusion syndrome is likely due to direct mitochondrial injury which primarily affects myocardial and skeletal muscle, but which also can cause mitochondrial injury in hepatocytes resulting in microvesicular fat in the liver. The cardiac manifestations tend to be most prominent and are the usual reason for fatalities. There may be a genetic predisposition (perhaps a subclinical form of a mitochondrial disorder) to the propofol infusion syndrome or lactic acidosis.
Outcome and Management
Management of the propofol infusion syndrome requires prompt discontinuation of the medication and cardiorespiratory support. Hemodialysis or hemofiltration may also be warranted. Lactic acidosis should be managed with intravenous fluids, 20% glucose infusions and bicarbonate. The idiosyncratic acute liver injury due to propofol is usually self-limited. Several reports of recurrence of propofol infusion syndrome upon restarting the anesthetic have been reported and reexposure should be avoided.
Drug Class: Anesthetic Agents
CASE REPORT
Case 1. Acute hepatitis after propofol anesthesia.(1)
A 62 year old woman underwent colonoscopy under propofol anesthesia and developed nausea, vomiting and epigastric pain 2 weeks later. She had no history of liver disease, took no medications, did not drink alcohol excessively and had no risk factors for viral hepatitis. She was jaundiced but was without signs of chronic liver disease. Laboratory testing showed marked elevations in ALT and AST with moderate increase in alkaline phosphatase (Table). She was admitted for evaluation. Tests for hepatitis A and B, EBV and cytomegalovirus were negative and autoantibodies were not found. She had antibody to hepatitis C (anti-HCV), although routine laboratory tests taken 6 months earlier had showed normal ALT levels. An abdominal CT scan showed no evidence of biliary obstruction. A liver biopsy showed an acute hepatocellular injury with mild fibrosis with changes suggesting a drug induced injury, rather than chronic hepatitis C. Subsequently, her symptoms resolved and laboratory tests had were falling when she was seen three weeks after onset.
Key Points
| Medication: | Propofol anesthesia (250 mg, total dose) |
|---|---|
| Pattern: | Hepatocellular (R=10.2) |
| Severity: | 3+ (jaundice, hospitalization) |
| Latency: | 14 days |
| Recovery: | Unclear, probably within 6 weeks |
| Other medications: | None mentioned |
Laboratory Values
| Time After Starting | Time After Stopping | ALT (U/L) | Alk P (U/L) | Bilirubin (mg/dL) | Other |
|---|---|---|---|---|---|
| Pre | Pre | 11 | 94 | 0.2 | |
| Outpatient colonoscopy under propofol anesthesia | |||||
| 14 days | 0 | 1313 | 322 | 4.8 | Admitted. INR=0.96 |
| 16 days | 2 days | 2219 | 311 | 6.7 | |
| 17 days | 3 days | 2008 | 289 | 7.2 | |
| 23 days | 8 days | 1504 | 225 | 10.0 | INR=1.34 |
| 25 days | 10 days | 914 | 232 | 10.5 | |
| 4 weeks | 2 weeks | 197 | 196 | 7.1 | |
| 5 weeks | 3 weeks | 62 | 162 | 4.4 | |
| Normal Values | <50 | <125 | <1.2 | ||
Comment
A possible case of drug induced liver injury in which the only medication exposure was propofol anesthesia given 2 weeks before clinical presentation with symptoms and jaundice. The course was somewhat prolonged and the INR rose slightly suggesting that the injury was significant. Propofol anesthesia has been used in several million patients and drug induced liver injury as a result must be very rare. An alternative explanation in this case was acute hepatitis C, which was perhaps the more likely diagnosis, but HCV RNA results and follow up testing results were not provided.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Propofol – Generic, Diprivan®
DRUG CLASS
Anesthetics
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Propofol | 2078-54-8 | C12-H18-O |
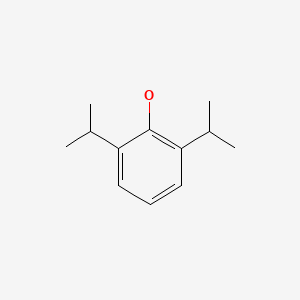
|
CITED REFERENCE
- 1.
- Nguyen HD, Borum ML. Acute hepatitis in a patient given propofol during colonoscopy. South Med J. 2009;102:333–4. [PubMed: 19204630]
ANNOTATED BIBLIOGRAPHY
References updated: 10 July 2020
- Patel PM, Pearn ML, Patel HH, Roth DM. Propofol. General anesthetics and therapeutic gases. In, Brunton LL, Hilal-Dandan, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 387-404.(Textbook of pharmacology and therapeutics).
- Kawar P, Briggs LP, Bahar M, McIlroy PDA, Dundee JW, Merrett JD, Nesbitt GS. Liver enzyme studies with disoprofol (ICI 35,868) and midazolam. Anaesthesia. 1982;37:305–8. [PubMed: 6979953](Controlled trial of propofol vs midazolam vs thiopentone as induction agent for nitrous oxide anesthesia in 72 patients with monitoring of serum enzymes over next 2 weeks [3 determinations]; average levels did not rise and minor elevations occurred equally in all three groups).
- Stark RD, Binks SM, Dutka VN, O'Connor KM, Arnstein MJ, Glen JB. A review of the safety and tolerance of propofol ('Diprivan'). Postgrad Med J. 1985;61 Suppl 3:152–6. [PubMed: 3877284](None of 155 patients given propofol anesthesia who were closely monitored in follow up had ALT elevations above 2 times ULN; no mention of hepatotoxicity or jaundice).
- [Adverse effects of propofol (Diprivan)]. Ugeskr Laeger 1990; 152: 1176. Danish. [PubMed: 2330646](The original report of what was later called the propofol infusion syndrome).
- Parke TJ, Stevens JE, Rice ASC, Greenway CL, Bray RJ, Smith PJ, Waldmann CS, et al. Metabolic acidosis and fatal myocardial failure after propofol infusion in children: five case reports. BMJ. 1992;305:613–6. [PMC free article: PMC1883365] [PubMed: 1393073](Initial report of propofol infusion syndrome in English: 5 children, ages 0.1 to 6 years on propofol at doses >4 mg/kg/hour for 4-6 days developed fatal arrhythmias and metabolic acidosis; microvesicular fat in liver on autopsy in 2).
- Motsch J, Schmidt H, Bach A, Böttiger BW, Böhrer H. Long-term sedation with propofol and green discolouration of the liver. Eur J Anaesthesiol. 1994;11:499–502. [PubMed: 7851359](56 year old man with complications of bowel resection for cancer requiring repeated open peritoneal lavage and ventilatory support, was treated with propofol and found to have "lawn-like" green color to liver 7 days later [bilirubin 5.9 mg/dL, ALT 20 U/L, Alk P 346 U/L, thought to be due to sepsis]; 2 weeks after propofol was stopped the liver was normal color).
- Müller C, Jelinek T, Endres S, Loeschke K. Z Gastroenterol. 1996;34:809–12. [Severe protracted cholestasis after general anesthesia in a patient with Alagille syndrome] [PubMed: 9082660](27 year old woman with Alagille syndrome developed severe cholestasis [bilirubin 59 mg/dL, ALT 61 U/L, Alk P 269 U/L] and ascites 4 weeks after general anesthesia with propofol and isoflurane; eventually resolved).
- Marinella MA. Lactic acidosis associated with propofol. Chest. 1996;109:292. [PubMed: 8549205](30 year old woman intubated for asthma and given iv propofol developed lactic acidosis within 2 hours which improved on stopping).
- Cray SH, Robinson BH, Cox PN. Lactic acidemia and bradyarrhythmia in a child sedated with propofol. Crit Care Med. 1998;26:2087–92. [PubMed: 9875925](10 month old given propofol at 10 mg/kg/hour for 4 days developed green urine, lactic acidosis and fatal bradyarrhythmia; microvesicular steatosis in the liver on autopsy).
- Hanna JP, Ramundo ML. Rhabdomyolysis and hypoxia associated with prolonged propofol infusion in children. Neurology. 1998;50:301–3. [PubMed: 9443502](Two children, ages 7 and 17 years, developed fatal arrhythmias, lactic acidosis, rhabdomyolysis after 1-3 days of propofol sedation for status epilepticus).
- Bray RJ. Propofol infusion syndrome in children. Paediatr Anaesth. 1998;8:491–9. [PubMed: 9836214](Summary of 18 cases of propofol infusion syndrome in children, only 3 of whom survived; usually received >4 mg/kg/hour for 1-5 days, dying of bradyarrhythmias, often with acidosis and hyperlipidemia and enlarged or fatty liver; among 9 children treated in one unit with propofol for at least 48 hours, 3 developed fatal syndrome compared to 0 of 26 sedated with other agents).
- Hatch DJ. Propofol-infusion syndrome in children. Lancet. 1999;353:1117–8. [PubMed: 10209973](Commentary on article by Bray in 1998 calling for a clinical trial to reassess safety of iv propofol in children).
- Bray RJ. Propofol-infusion syndrome in children. Lancet. 1999;353:2074–5. [PubMed: 10376650](Response to letter from Hatch in 1999 citing ethical concerns of doing clinical trials of propofol in children).
- Murdoch SD, Cohen AT. Propofol-infusion syndrome in children. Lancet. 1999;353:2074–5. [PubMed: 10376651](Survey of 218 ICUs in UK; 47 reported that they used propofol in children including 11 of 18 pediatric units, limiting to doses of 1-4 mg/kg/hour and only for short term).
- Mehta N, De Hunter C, Parviz H, Nadel S, Britto J. Short-term propofol infusions in children. Lancet. 1999;354:866–7. [PubMed: 10485752](18 month old developed acidosis 5 hours after starting propofol with subsequent arrhythmia and renal and respiratory failure).
- Stelow EB, Johari VP, Smith SA, Crosson JT, Apple FS. Propofol-associated rhabdomyolysis with cardiac involvement in adults: chemical and anatomic findings. Clin Chem. 2000;46:577–81. [PubMed: 10759487](47 year old woman and 41 year old man developed rhabdomyolysis with marked CPK and troponin I elevations within 2-4 hours of starting high doses of iv propofol during intubation for asthma; one died).
- Perrier ND, Baerga-Varela Y, Murray MJ. Death related to propofol use in an adult patients. Crit Care Med. 2000;28:3071–4. [PubMed: 10966298](18 year old man with head trauma given iv propofol [5.8-7.6 mg/kg/hour] developed arrhythmias on day 5 followed by progressive lactic acidosis, hyperlipidemia, and death in asystole).
- Cannon ML, Glazier SS, Bauman LA. Metabolic acidosis, rhabdomyolysis, and cardiovascular collapse after prolonged propofol infusion. J Neurosurg. 2001;95:1053–6. [PubMed: 11765823](13 year old girl given propofol [6 mg/kg/hour] in ICU for 4 days developed green urine, acidosis and right bundle branch block with coved ST segments and subsequent cardiovascular collapse; autopsy showed "no hepatic steatosis").
- Kelly DF. Propofol-infusion syndrome. J Neurosurg. 2001;95:925–6. [PubMed: 11765835](Editorial on case described by Cannon et al., reporting a case in an adult man with acidosis and cardiovascular collapse after 55 hours of propofol sedation).
- Cremer OL, Moons KG, Bouman EA, Kruijswijk JE, de Smet AM, Kalkman CJ. Long-term propofol infusion and cardiac failure in adult head-injured patients. Lancet. 2001;357:117–8. [PubMed: 11197401](Retrospective review of 67 head injured ICU patients who received propofol for more than 24 hours; 7 developed propofol infusion syndrome, onset in 24-48 hours with arrhythmias and 6 with acidosis, usually with higher doses [>5 mg/kg/hour]).
- Anand K, Ramsay MA, Crippin JS. Hepatocellular injury following the administration of propofol. Anesthesiology. 2001;95:1523–4. [PubMed: 11748416](17 year old girl developed nausea the day after propofol anesthesia for outpatient hernia repair, ALT rising to 1567 U/L [day 3] but normal Alk P and bilirubin, resolving within 2 weeks).
- Badr AE, Mychaskiw G, Eichhorn JH. Metabolic acidosis associated with a new formulation of propofol. Anesthesiology. 2001;94:536–8. [PubMed: 11374620](21 year old woman with intracerebral bleed treated with iv propofol [4.5-9 mg/kg/hour] developed lactic acidosis after 2 days and died after 3).
- Wolf A, Weir P, Segar P, Stone J, Shield J. Impaired fatty acid oxidation in propofol infusion syndrome. Lancet. 2001;357:606–7. [PubMed: 11558490](2 year old boy with head trauma given propofol [5.2 mg/kg/hour] developed renal insufficiency on day 4 followed by arrhythmias and lactic acidosis, responded to stopping propofol and hemofiltration; high C5-acylcarnitide suggested impaired mitochondrial fatty acid oxidation).
- Kang TM. Propofol infusion syndrome in critically ill patients. Ann Pharmacother. 2002;36:1453–6. [PubMed: 12196066](Review of propofol infusion syndrome; mentions unpublished prospective, randomized clinical trial in children which found higher rate of death [8% and 11%] with propofol than standard agents [4%]).
- Ernest D, French C. Propofol infusion syndrome-report of an adult fatality. Anaesth Intensive Care. 2003;31:316–9. [PubMed: 12879680](31 year old man with head injury maintained on propofol anesthesia [average 5.8 mg/kg/hour] developed EKG changes and CPK rise [11,100 U/L] starting on day 4, and dying with lactic acidosis and asystole on day 7).
- Holzki J, Aring C, Gillor A. Death after re-exposure to propofol in a 3-year-old child: a case report. Paediatr Anaesth. 2004;14:265–70. [PubMed: 14996268](3 year old girl ventilated for aspiration pneumonia with propofol developed acidosis after 15 hours [20 mg/kg/hour], improving on stopping propofol, but acutely worsening within 8 hours of restarting with arrhythmias and cardiovascular collapse).
- Koch M, De Backer D, Vincent JL. Lactic acidosis: an early marker of propofol infusion syndrome? Intensive Care Med. 2004;30:522. [PubMed: 14685664](5 year old girl with embolization of an arterial-venous malformation was sedated with propofol [15 mg/kg/hour] developed lactic acidosis within 6 hours, reversing upon stopping).
- Burow BK, Johnson ME, Packer DL. Metabolic acidosis associated with propofol in the absence of other causative factors. Anesthesiology. 2004;101:239–41. [PubMed: 15220796](31 year old woman developed acidosis between 5-6.5 hours of propofol anesthesia [~5 mg/kg/hour], reversing rapidly with discontinuation).
- Salengros JC, Velghe-Lenelle CE, Bollens R, Engleman E, Barvals L. Lactic acidosis during propofol-remifentanil anaesthesia in an adult. Anesthesiology. 2004;101:241–3. [PubMed: 15220797](64 year old man developed tachycardia after 3 hours of propofol anesthesia [~8 mg/kg/hour] with subsequent lactic acidosis [lactate rising from 1.45 to 8.57 mM, pH falling from 7.43 to 7.28], but rapid resolution on stopping propofol after 4.5 hours).
- Russo MW, Galanko JA, Shrestha R, Fried MW, Watkins P. Liver transplantation for acute liver failure from drug-induced liver injury in the United States. Liver Transpl. 2004;10:1018–23. [PubMed: 15390328](Among ~50,000 liver transplants done in the United States between 1990 and 2002, 137 [0.2%] were done for idiosyncratic drug induced acute liver failure, but none were attributed to propofol).
- Liolios A, Guét JM, Scholtes JL, Raftopoulos C, Hantson P. Propofol infusion syndrome associated with short-term large-dose infusion during surgical anesthesia in an adult. Anesth Analg. 2005;100:1804–6. [PubMed: 15920217](42 year old man developed lactic acidosis within 15 hours of starting propofol [2.3-9 mg/kg/hour], rapidly reversing with stopping).
- Haase R, Sauer H, Eichler G. Lactic acidosis following short-term propofol infusion may be an early warning of propofol infusion syndrome. J Neurosurg Anesthesiol. 2005;17:122–3. [PubMed: 15841003](7 year old boy developed increased lactate levels 5 hours after receiving 40 minutes of propofol sedation spontaneously improving).
- Farag E, DeBoer G, Cohen BH, Niezgoda J. Anesthesiology. 2005;102:697–8. [PubMed: 15731621](Letter suggesting that patients developing lactic acidosis on propofol have a subclinical mitochondrial disorder, mentioning that use of propofol in patients undergoing muscle biopsy for mitochondrial diseases was complicated by prolonged recovery).
- Chukwuemeka A, Ko R, Ralph-Edwards A. Short-term low-dose propofol anaesthesia associated with severe metabolic acidosis. Anaesth Intensive Care. 2006;34:651–5. [PubMed: 17061643](45 year old man undergoing coronary bypass graft developed lactic acidosis after 6 hours of propofol anesthesia, reversing rapidly on stopping).
- Polo-Romero FJ. Propofol is not so safe for ERCP. Hepatobiliary Pancreat Dis Int. 2006;5:314–author reply 315. [PubMed: 16698600](65 year old man received propofol during ERCP for biliary pancreatitis and 48 hours later had rise in ALT [50 times ULN], Alk P [slight increase] and bilirubin [8.9 mg/dL], with rapid recovery and normal values 2 weeks later; suspected propofol as cause of acute liver injury).
- Kam PCA, Cardone D. Propofol infusion syndrome. Anaesthesia. 2007;62:690–701. [PubMed: 17567345](Systematic review including history and definition of propofol infusion syndrome; listing of 61 cases, including 38 deaths and 32 pediatric cases; discussion of mechanisms of injury and management).
- Fodale V, La Monaca E. Propofol infusion syndrome: an overview of a perplexing disease. Drug Saf. 2008;31:293–303. [PubMed: 18366240](Review of propofol infusion syndrome including summary and listing of all published cases).
- Vanlersberghe C, Camu F. Propofol. Handb Exp Pharmacol. 2008;(182):227–52. [PubMed: 18175094](Extensive review of pharmacology, metabolism, mechanism of action and pharmacologic effects of propofol).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J., Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology. 2008;135:1924–34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected between 2004 and 2008, propofol was implicated as possibly the cause in one case that was later attributed to cefazolin).
- Laquay N, Pouard P, Silicani MA, Vaccaroni L, Orliaguet G. Early stages of propofol infusion syndrome in paediatric cardiac surgery: two cases in adolescent girls. Br J Anaesth. 2008;101:880–1. [PubMed: 19004919](12 and 16 year old girls had second cardiac operations under propofol anesthesia [<3 mg/kg/hour] and developed rising lactate levels within 2-6 hours, reversing after stopping).
- Tan CK, Lai CC, Cheng KC. Propofol-related green urine. Kidney Int. 2008;74:978. [PubMed: 18794836](52 year old man with cirrhosis was given single bolus of iv propofol [100 mg] and developed green urine one hour later).
- Polo-Romero FJ, Paricio P, Tovar A, Alonso JM. Propofol-induced acute toxic hepatitis after brief sedation for endoscopic retrograde cholangiopancreatography. Endoscopy. 2008;40 Suppl 2:E49. [PubMed: 18300198](Same case as described by Polo-Romero in 2006).
- Rison RA, Ko DY. Isolated fatty liver from prolonged propofol use in a pediatric patient with refractory status epilepticus. Clin Neurol Neurosurg. 2009;111:558–61. [PubMed: 19395155](13 year old girl with status epilepticus and complex medical course with multiple medications developed hepatomegaly and "macrofasicular fatty deposits" on liver biopsy after 56 days of propofol sedation [2 mg/kg/hour] with preexisting ALT elevation rising from 135 to 380 U/L; high ammonia levels but no mention of Alk P or bilirubin).
- Orsini J, Nadkarni A, Chen J, Cohen N. Propofol infusion syndrome: case report and literature review. Am J Health Syst Pharm. 2009;66:908–15. [PubMed: 19420309](36 year old woman with HCV/HIV coinfection developed rash, ALT [536 U/L] and CPK [36,327 U/L] elevations with normal lactate levels and no acidosis after 7 days of iv propofol [1.5 mg/kg/hour], resolving on switching to phenobarbital; patient had received multiple other medications).
- Nguyen HD, Borum ML. Acute hepatitis in a patient given propofol during colonoscopy. South Med J. 2009;102:333–4. [PubMed: 19204630](62 year old woman developed jaundice 2 weeks after colonoscopy and propofol anesthesia with bilirubin 4.8 mg/dL, ALT 1313 U/L, Alk P 322 U/L and recovery within 2 weeks; patient also had anti-HCV. Case 1).
- Roberts RJ, Barletta JF, Fong J, Schumaker G, Kuper P, Papadopoulos S, Yogaratnam D, et al. Incidence of propofol-related infusion syndrome in critically ill adults: a prospective, multicenter study. Crit Care. 2009;13:R169. [PMC free article: PMC2784401] [PubMed: 19874582](Prospective study of 1017 critically ill patients on propofol for more than 24 hours; 1.1% developed propofol infusion syndrome but most cases were mild, mortality rate 18% [n=2], and no patient had classical cardiac manifestations).
- Jorens PG, Van den Eynden GG. Propofol infusion syndrome with arrhythmia, myocardial fat accumulation and cardiac failure. Am J Cardiol. 2009;104:1160–2. [PubMed: 19801042](12 year old boy developed rhabdomyolysis [CPK 863,000 U/L] and fatal arrythmias after 5 days of propofol sedation for head trauma; autopsy showed fat in myocardial and skeletal muscles; no mention of the liver).
- Sammartino M, Garra R, Sbaraglia F, Papacci P. Propofol overdose in a preterm baby: may propofol infusion syndrome arise in two hours? Paediatr Anaesth. 2010;20:973–4. [PubMed: 20849514](Neonate and preterm baby receiving 2 hours of propofol anesthesia [later found to be an overdose] developed hypotension and bradycardia [ALT 5760 U/L, Alk P 630 U/L, pH 7.35], with rapid recovery and normal enzymes within 1 day).
- Wong JM. Propofol infusion syndrome. Am J Ther. 2010;17:487–91. [PubMed: 20844346](Review of the history of description of propofol infusion syndrome, diagnosis, prognosis, treatment and suspected mechanisms).
- Kneiseler G, Bachmann HS, Bechmann LP, Dechene A, Heyer T, Baba H, Saner F, et al. A rare case of propofol-induced acute liver failure and literature review. Case Rep Gastroenterol. 2010;4:57–65. [PMC free article: PMC2988899] [PubMed: 21103229](35 year old woman developed jaundice and signs of hepatic failure one week after surgery and propofol anesthesia [bilirubin ~18.5 mg/dL, ALT ~1050 U/L, INR ~1.6], liver biopsy showing massive necrosis and mild fat, resolving rapidly over next month).
- Reuben A, Koch DG, Lee WM., Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology. 2010;52:2065–76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury including 2 attributed to anesthetic agents, one to halothane and one to isoflurane, but none to propofol).
- Correia LM, Bonilha DQ, Gomes GF, Brito JR, Nakao FS, Lenz L, Rohr MR, et al. Sedation during upper GI endoscopy in cirrhotic outpatients: a randomized, controlled trial comparing propofol and fentanyl with midazolam and fentanyl. Gastrointest Endosc. 2011;73(1):45–51.e1. [PubMed: 21184869](Among 210 patients with cirrhosis undergoing endoscopy comparing propofol and midazolam anesthesia, propofol was more efficacious and had a shorter recovery time than midazolam, side effects were similar; no mention of worsening of liver disease).
- Fagà E, De Cento M, Giordanino C, Barletti C, Bruno M, Carucci P, De Angelis C, et al. Safety of propofol in cirrhotic patients undergoing colonoscopy and endoscopic retrograde cholangiography: results of a prospective controlled study. Eur J Gastroenterol Hepatol. 2012;24:70–6. [PubMed: 21941187](Among 214 patients undergoing endoscopic procedures under propofol anesthesia, the dose of propofol, duration of sedation and rate of complications was the same in those with cirrhosis [61] as those without [153]).
- Wang D, Chen C, Chen J, Xu Y, Wang L, Zhu Z, Deng D, et al. The use of propofol as a sedative agent in gastrointestinal endoscopy: a meta-analysis. PLoS One. 2013;8:e53311. [PMC free article: PMC3540096] [PubMed: 23308191](A systematic review of 22 randomized controlled trials of propofol vs other agents as anesthesia during endoscopy found propofol to provide better sedation and shorter recovery compared to conventional agents, without differences in rates of in adverse events).
- Asai A, Yagi M, Tsuchimoto Y, Fukunishi S, Takeshita A, Tsuda Y, Fukuda A, et al. A rare case of propofol-induced liver injury during modified electroconvulsive therapy in an elderly woman. Intern Med. 2013;52:761–5. [PubMed: 23545671](A 75 year old woman developed evidence of liver injury 5 days after a third course of electroshock therapy for depression under propofol anesthesia [bilirubin 1.6 mg/dL, ALT 3246 U/L, Alk P 632 U/L, LDH 2841 U/L], resolving within 2 weeks).
- Savard M, Dupré N, Turgeon AF, Desbiens R, Langevin S, Brunet D. Propofol-related infusion syndrome heralding a mitochondrial disease: case report. Neurology. 2013;81:770–1. [PMC free article: PMC3776462] [PubMed: 23873972](27 year old woman with intractable status epilepticus developed metabolic acidosis and EKG abnormalities 3 days after starting intravenous propofol therapy which improved on stopping, but she was resistant to all anticonvulsant therapy and subsequent testing found mutations in the POLG1 gene).
- Bowdle A, Richebe P, Lee L, Rostomily R, Gabikian P. Hypertriglyceridemia, lipemia, and elevated liver enzymes associated with prolonged propofol anesthesia for craniotomy. Ther Drug Monit. 2014;36:556–9. [PubMed: 25222854](39 year old woman with brain tumor undergoing two-stage neurosurgical removal developed lipemic serum during 19 hour infusion of propofol [pH 7.46, triglycerides 15.8 nmol/L] and had elevated ALT postoperatively [ALT 420 U/L, Alk P 130 U/L, bilirubin not given], with improved rapidly thereafter).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A, Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America. An analysis of published reports. Ann Hepatol. 2014;13:231–9. [PubMed: 24552865](Systematic review of literature of drug induced liver injury in Latin American countries published from 1996 to 2012 identified 176 cases, none of which were attributed to propofol).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 5 cases [0.4%] were attributed to general anesthetics [2 to isoflurane, 2 to sevoflurane, 1 to ketamine] but none to propofol).
- Dabir S, Mohammad-Taheri Z, Parsa T, Abbasi-Nazari M, Radpay B, Radmand G. Effects of propofol versus isoflurane on liver function after open thoracotomy. Asian Cardiovasc Thorac Ann. 2015;23:292–8. [PubMed: 25227774](Among 88 patients undergoing elective thoracotomy under either sevoflurane or propofol anesthesia, minor transient elevations in ALT and AST occurred at postoperative days 1 and 3 in small numbers of patients, but more frequently with sevoflurane and without symptoms or jaundice).
- Mirrakhimov AE, Voore P, Halytskyy O, Khan M, Ali AM. Propofol infusion syndrome in adults: a clinical update. Crit Care Res Pract. 2015;2015:260385. [PMC free article: PMC4410753] [PubMed: 25954513](Review of the history, pathogenesis, risk factors, clinical features and management of propofol infusion syndrome in adults).
- Yatabe T, Yamashita K, Yokoyama M. Drug fever caused by propofol in the intensive care unit. J Anesth. 2015;29:786–9. [PubMed: 25801543](57 year old woman developed fever after a segmental hepatic resection without evidence of infection while on continuous propofol which continued for 5 days until propofol was stopped [ALT rising to 1316 U/L and AST to 3395 U/L on postoperative day 3]).
- Starczewska MH, Mon W, Shirley P. Anaesthesia in patients with liver disease. Curr Opin Anaesthesiol. 2017;30:392–8. [PubMed: 28306680](Review and recommendations on anesthesia in patients with liver disease recommends use of propofol or the newer inhalation agents that have minimal hepatic metabolism [sevoflurane and desflurane]).
- Vollmer JP, Haen S, Wolburg H, Lehmann R, Steiner J, Reddersen S, Fend F, et al. Propofol related infusion syndrome: ultrastructural evidence for a mitochondrial disorder. Crit Care Med. 2018;46:e91–e94. [PubMed: 29252954](19 year old male with an intracerebral bleed from an arterio-venous malformation underwent surgery with anesthesia and subsequent sedation with propofol for 5 days developing brain edema and tachyarrhythmia followed by asystole, autopsy showing massive hepatic steatosis and electron dense material associated with mitochondria in heart muscle).
- Watanabe K, Hikichi T, Takagi T, Suzuki R, Nakamura J, Sugimoto M, Kikuchi H, et al. Propofol is a more effective and safer sedative agent than midazolam in endoscopic injection sclerotherapy for esophageal varices in patients with liver cirrhosis: a randomized controlled trial. Fukushima J Med Sci. 2018;64:133–41. [PMC free article: PMC6305790] [PubMed: 30344206](Among 23 patients undergoing sclerotherapy for esophageal varices sedated with either propofol or midazolam, neurologic worsening occurred to a similar extent with both, but propofol provided better sedation and patient satisfaction).
- Ichikawa T, Okuyama K, Kamata K, Masui K, Ozaki M. Suspected propofol infusion syndrome during normal targeted propofol concentration. J Anesth. 2020 Mar 28; Epub ahead of print. [PubMed: 32222909](55 year old woman with an orbital mass undergoing awake craniotomy with propofol anesthesia developed lactic acidosis during therapy with appropriately calculated dose, but was found to have plasma levels 12 times higher than predicted and acidosis reversed rapidly with switching anesthetic agents).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Propofol infusion syndrome: a case of increasing morbidity with traumatic brain injury.[Am J Crit Care. 2007]Propofol infusion syndrome: a case of increasing morbidity with traumatic brain injury.Sabsovich I, Rehman Z, Yunen J, Coritsidis G. Am J Crit Care. 2007 Jan; 16(1):82-5.
- The syndrome of irreversible acidosis after prolonged propofol infusion.[Neurocrit Care. 2005]The syndrome of irreversible acidosis after prolonged propofol infusion.Kumar MA, Urrutia VC, Thomas CE, Abou-Khaled KJ, Schwartzman RJ. Neurocrit Care. 2005; 3(3):257-9.
- Metabolic acidosis, rhabdomyolysis, and cardiovascular collapse after prolonged propofol infusion.[J Neurosurg. 2001]Metabolic acidosis, rhabdomyolysis, and cardiovascular collapse after prolonged propofol infusion.Cannon ML, Glazier SS, Bauman LA. J Neurosurg. 2001 Dec; 95(6):1053-6.
- Review Rhabdomyolysis and hypoxia associated with prolonged propofol infusion in children.[Neurology. 1998]Review Rhabdomyolysis and hypoxia associated with prolonged propofol infusion in children.Hanna JP, Ramundo ML. Neurology. 1998 Jan; 50(1):301-3.
- Review The propofol infusion 'syndrome' in intensive care unit: from pathophysiology to prophylaxis and treatment.[Acta Anaesthesiol Belg. 2008]Review The propofol infusion 'syndrome' in intensive care unit: from pathophysiology to prophylaxis and treatment.Papaioannou V, Dragoumanis C, Theodorou V, Pneumatikos I. Acta Anaesthesiol Belg. 2008; 59(2):79-86.
- Propofol - LiverToxPropofol - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...