NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Oxaliplatin is an intravenously administered platinum containing alkylating agent which is used for the treatment of advanced colorectal cancer. Oxaliplatin therapy is associated with a low rate of transient serum aminotransferase elevations, but is commonly associated with sinusoidal and vascular injury to the liver which can lead to sinusoidal obstruction syndrome and to nodular regenerative hyperplasia with noncirrhotic portal hypertension.
Background
Oxaliplatin (ox al" i pla' tin) is a cisplatin analog with a tetravalent platinum molecule which is referred to as a platinum coordination complex. Oxaliplatin acts as an alkylating agent causing cross linking between and within DNA strands leading to inhibition of DNA, RNA and protein synthesis and the triggering of programmed cell death, mostly in rapidly dividing cells. Oxaliplatin was approved for use in cancer chemotherapy in the United States in 2002. Its current indications are colorectal carcinoma and it is usually administered in combination with other agents such as 5-fluorouracil (5-FU), irinotecan or capecitabine. Oxaliplatin is available in an aqueous solution for injection in 50, 100 and 200 mg vials in generic forms and under the brand name Eloxatin. The typical dose regimen is a single infusion of oxaliplatin (85 mg/m2) on day 1 of each two-week course with leucovorin and 5-FU. Oxaliplatin should be administered only by health care professions with knowledge and experience in using cancer chemotherapeutic agents and in management of their complications. The platinum based antineoplastic agents have similar toxicities, including nausea and vomiting, diarrhea, bone marrow suppression, as well as neuro-, oto- and nephrotoxicity. They are also mutagenic, teratogenic and carcinogenic, and their use has been associated with an increased risk of secondary leukemias. Uncommon but potentially severe adverse events include anaphylaxis, neuropathy, interstitial pulmonary disease and fibrosis, hepatotoxicity and embryo-fetal toxicity.
Hepatotoxicity
Mild and transient elevations in serum aminotransferase levels are found in an appreciable proportion of patients taking oxaliplatin, but their relationship to oxaliplatin is often unclear. Chemotherapy with oxaliplatin has been associated with histological changes in the liver marked by sinusoidal dilatation, congestion and centrolobular necrosis indicative of sinusoidal obstruction syndrome. These changes are usually mild-to-moderate in severity and not clinically significant during the acute phase, but they can progress to clinically apparent sinusoidal obstruction syndrome or, with chronic therapy, to nodular regenerative hyperplasia with splenomegaly, thrombocytopenia and esophageal varices. Nodular regenerative hyperplasia typically requires 6 to 18 months to develop and arises after repeated cycles of chemotherapy with oxaliplatin. Serum enzyme and bilirubin elevations are minimal, the major laboratory finding being a progressive and persistent thrombocytopenia reflecting the development of splenomegaly and portal hypertension. The first clinical evidence of nodular regenerative hyperplasia may be ascites, esophageal variceal hemorrhage or hepatic encephalopathy. Attempts at hepatic resection, severe gastrointestinal bleeding and septicemia may trigger hepatic decompensation and liver failure. Interestingly, nodular regenerative hyperplasia and portal hypertension tend to improve slowly once chemotherapy is stopped, but the long term consequences of the changes are not well defined.
Likelihood score: A (well established cause of clinically apparent liver injury).
Mechanism of Injury
The cause of sinusoidal dilatation and central congestion after oxaliplatin therapy is unknown, but probably relates to injury to sinusoidal endothelial lining cells. While described largely after oxaliplatin therapy, similar changes may occur after therapy with the other platinum coordination complexes, alkylating agents and antimetabolites.
Outcome and Management
The majority of instances of sinusoidal dilatation, vascular injury and congestion found histologically after oxaliplatin therapy occur without significant serum enzyme elevations or clinically apparent liver injury. Rare instances of acute onset of sinusoidal obstruction syndrome with ascites and hepatic failure have been described after oxaliplatin therapy, but usually when given in combination with other antineoplastic agents. Repeated cycles of oxaliplatin and chronic therapy have been linked to nodular regenerative hyperplasia which can be associated with portal hypertension and complications of ascites, variceal hemorrhage and hepatic encephalopathy. There is likely to be cross sensitivity to liver toxicities of the various platinum coordination complexes and continued use or rechallenge after clinically apparent liver injury from oxaliplatin should be avoided. Routine monitoring of liver tests is recommended during courses of oxaliplatin therapy, but evidence of portal hypertension is better assessed using serial platelet counts or repeated radiologic evaluation of spleen size.
Drug Class: Antineoplastic Agents, Alkylating Agents
Other Drugs in the Subclass, Platinum Coordination Complexes: Carboplatin, Cisplatin
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Oxaliplatin – Generic, Eloxatin®
DRUG CLASS
Antineoplastic Agents, Alkylating Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Oxaliplatin | 61825-94-3 | C8-H14-N2-O4-Pt |
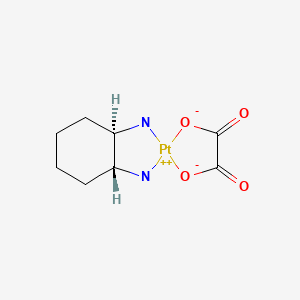
|
ANNOTATED BIBLIOGRAPHY
References updated: 12 September 2020
- Abbreviations: BMI, body mass index; CT, computerized tomography; NRH, nodular regenerative hyperplasia; SOS, sinusoidal obstruction syndrome; HVPG, hepatic venous pressure gradient; SAMe, S-adenosylmethionine.
- Zimmerman HJ. Oncotherapeutic and immunosuppressive agents. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 673-708.(Expert review of hepatotoxicity of cancer chemotherapeutic agents published in 1999; mentions that cisplatin had been reported to cause dose related serum enzyme elevations and has been linked to steatosis and necrosis, whereas carboplatin has been linked to rare instances of cholestatic and hepatocellular injury; oxaliplatin not discussed).
- DeLeve LD. Liver sinusoidal endothelial cells and liver injury. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, p. 139-43.(Review of liver injury to sinusoidal endothelial cells caused by medications mentions that oxaliplatin as capable of causing sinusoidal dilatation, peliosis hepatis, nodular regenerative hyperplasia and sinusoidal obstruction syndrome).
- Wellstein A, Giaccone G, Atkins MB, Sausville EA. Cytotoxic agents. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 1167-201.(Textbook of pharmacology and therapeutics).
- Jones RJ, Lee KS, Beschorner WE, Vogel VG, Grochow LB, Braine HG, Vogelsang GB, et al. Veno-occlusive disease of the liver following bone marrow transplantation. Transplantation. 1987;44:778–83. [PubMed: 3321587](Among 235 patients undergoing bone marrow transplantation between 1982 and 1985, SOS developed in 52 [22%] of whom half died, making SOS the third most common cause of death in this population).
- Washington K, Lane KL, Meyers WC. Nodular regenerative hyperplasia in partial hepatectomy specimens. Am J Surg Pathol. 1993;17:1151–8. [PubMed: 8214260](Pathological review of liver resections from 72 patients showed nodular regenerative hyperplasia in 5, all of whom had colon cancer metastases and had been treated with chemotherapy: usually 5-fluorouracil; 9 patients had hyperplastic foci some of whom had received cisplatin and other agents including cyclophosphamide, VP-16 and carmustine).
- Hartmann JT, Lipp H-P. Toxicity of platinum compounds. Expert Opin Pharmacother. 2003;4:889–901. [PubMed: 12783586](Review of pharmacology, mechanism of action, adverse effects and tolerance of platinum containing alkylating agents; "Mild reversible increases in liver function tests can occur in patients who have received platinum compounds. However, the platinum compounds are generally not classified as hepatotoxic drugs").
- Rubbia-Brandt L, Audard V, Sartoretti P, Roth AD, Brezault C, Le Charpentier M, Dousset B, et al. Severe hepatic sinusoidal obstruction associated with oxaliplatin-based chemotherapy in patients with metastatic colorectal cancer. Ann Oncol. 2004;15:460–6. [PubMed: 14998849](Among 153 patients undergoing hepatic resection for colon cancer, centrolobular congestion and necrosis was found in nontumor liver tissue in 51% of those who received neoadjuvant chemotherapy, but in none undergoing surgery alone; oxaliplatin as the most frequently implicated agent; follow up biopsies often showed fibrosis).
- Sebagh M, Plasse M, Lévi F, Adam R. Severe hepatic sinusoidal obstruction and oxaliplatin-based chemotherapy in patients with metastatic colorectal cancer: a real entity? Ann Oncol. 2005;16(2):331–Author reply 332-3. [PubMed: 15668292](Letter in response to Rubbia-Brandt [2004] questioning the clinical significance of the histological findings; among 700 patients treated "mainly" by oxaliplatin, the authors mention no increase in operative mortality).
- Tisman G, MacDonald D, Shindell N, Reece E, Patel P, Honda N, Nishimora EK, et al. Oxaliplatin toxicity masquerading as recurrent colon cancer. J Clin Oncol. 2004;22:3202–4. [PubMed: 15284280](69 year old man with adenocarcinoma of the rectum developed ascites after radiation and a fourth course of chemotherapy with capecitabine and oxaliplatin, with a hepatic venous pressure gradient of 18 mm Hg and liver biopsy showing sinusoidal obstruction syndrome and no cirrhosis [bilirubin and Alk P elevated but ALT normal], with progressive hepatic and multiorgan failure and death).
- Fernandez FG, Ritter J, Goodwin JW, Linehan DC, Hawkins WG, Strasberg SM. Effect of steatohepatitis associated with irinotecan or oxaliplatin pretreatment on resectability of hepatic colorectal metastases. J Am Coll Surg. 2005;200:845–53. [PubMed: 15922194](Among patients undergoing hepatic resections for colorectal cancer metastases, steatohepatitis and liver injury was more common among the 14 who received oxaliplatin and/or irinotecan than 10 who received 5-FU alone or 13 given no chemotherapy).
- Rubbia-Brandt L, Mentha G, Terris B. Sinusoidal obstruction syndrome is a major feature of hepatic lesions associated with oxaliplatin neoadjuvant chemotherapy for liver colorectal metastases. J Am Coll Surg. 2006;202:199–200. [PubMed: 16377516](Letter in response to Fernandez [2005] suggesting that some of the hepatic changes represented sinusoidal obstruction syndrome).
- Aloia T, Sebagh M, Plasse M, Karam V, Lévi F, Giacchetti S, Azoulay D, et al. Liver histology and surgical outcomes after preoperative chemotherapy with fluorouracil plus oxaliplatin in colorectal cancer liver metastases. J Clin Oncol. 2006;24:4983–90. [PubMed: 17075116](Among 92 patients undergoing resection of colorectal liver metastases, those who received chemotherapy [mostly oxaliplatin and fluorouracil] were more likely to have vascular changes, but had similar rates of steatosis compared to those who did not receive chemotherapy).
- Vauthey JN, Pawlik TM, Ribero D, Wu TT, Zorzi D, Hoff PM, Xiong HQ, et al. Chemotherapy regimen predicts steatohepatitis and an increase in 90-day mortality after surgery for hepatic colorectal metastases. J Clin Oncol. 2006;24:2065–72. [PubMed: 16648507](Among 406 patients undergoing hepatic resection for colorectal metastases, preoperative chemotherapy with oxaliplatin was associated with sinusoidal dilatation [19% vs 2%], whereas irinotecan was associated with steatohepatitis [20% vs 4.4%] which was associated with higher 90 day mortality rates).
- Karoui M, Penna C, Amin-Hashem M, Mitry E, Benoist S, Franc B, Rougier P, et al. Influence of preoperative chemotherapy on the risk of major hepatectomy for colorectal liver metastases. Ann Surg. 2006;243:1–7. [PMC free article: PMC1449955] [PubMed: 16371728](Retrospective analysis of 67 patients undergoing hepatic resection of colorectal liver metastasis, found preoperative chemotherapy was associated with higher rates of complications [38% vs 14%] and hepatic failure [11% vs 0%] compared to no chemotherapy, despite no difference in degree of elevation of liver tests during first 10 postoperative days).
- Higashiyama H, Harabayashi T, Shinohara N, Chuma M, Hige S, Nonomura K. Reactivation of hepatitis in a bladder cancer patient receiving chemotherapy. Int Urol Nephrol. 2007;39:461–3. [PubMed: 17171423](A 59 year old woman with bladder cancer who was an HBV carrier developed severe reactivation of hepatitis B after 2 cycles of chemotherapy with methotrexate, epiadriamycin and cisplatin, resolving with lamivudine and prednisolone therapy).
- Zorzi D, Laurent A, Pawlik TM, Lauwers GY, Vauthey J-N, Abdalla EK. Chemotherapy-associated hepatotoxicity and surgery for colorectal liver metastases. Brit J Surg. 2007;94:274–86. [PubMed: 17315288](Systematic review of liver toxicity occurring after preoperative systemic chemotherapy for colorectal liver metastases, oxaliplatin has been linked to histological changes in microvasculature of the liver but not with increased mortality rate or hepatic failure).
- Liao Y, Lu X, Lu C, Li G, Jin Y, Tang H. Selection of agents for prevention of cisplatin-induced hepatotoxicity. Pharmacol Res. 2008;57:125–31. [PubMed: 18282716](Analysis of factors that decreased hepatotoxicity of cisplatin in animal model found antioxidants and glutathione precursors were effective in decreasing ALT elevations during therapy).
- Schouten van der Velden AP, Punt CJ, Van Krieken JH, Derleyn VA, Ruers TJ. Hepatic veno-occlusive disease after neoadjuvant treatment of colorectal liver metastases with oxaliplatin: a lesson of the month. Eur J Surg Oncol. 2008;34:353–5. [PubMed: 17207961](54 year old man with colon cancer metastatic to liver underwent attempt at resection followed by 11 cycles of chemotherapy [5-fluorouracil, and oxaliplatin] and repeat hepatic resection, but developed liver failure and died postoperatively, autopsy showing absence of central hepatic vein in the area of the resected tumor).
- Morris-Stiff G, Tan YM, Vauthey JN. Hepatic complications following preoperative chemotherapy with oxaliplatin or irinotecan for hepatic colorectal metastases. Eur J Surg Oncol. 2008;34:609–14. [PubMed: 17764887](Systematic review of the literature on oxaliplatin and liver injury; histological vascular changes with sinusoidal damage occurs in at least 20% of patients treated with oxaliplatin, but it is not associated with an increase in mortality in most studies).
- Khan AZ, Morris-Stiff G, Makuuchi M. Patterns of chemotherapy-induced hepatic injury and their implications for patients undergoing liver resection for colorectal liver metastases. J Hepatobiliary Pancreat Surg. 2009;16:137–44. [PubMed: 19093069](Review of liver injury from neoadjuvant therapy of colon cancer metastases; oxaliplatin is frequently associated with sinusoidal injury, but rarely with clinically significant SOS).
- Brouquet A, Benoist S, Julie C, Penna C, Beauchet A, Rougier P, Nordlinger B. Risk factors for chemotherapy-associated liver injuries: A multivariate analysis of a group of 146 patients with colorectal metastases. Surgery. 2009;145:362–71. [PubMed: 19303984](Analysis of factors predictive of steatosis, steatohepatitis and sinusoidal dilatation in liver tissue from 146 patients undergoing liver resection of colorectal metastases found that oxaliplatin based chemotherapy was a risk factor for sinusoidal changes [Hazard ratio 4.4]).
- Kudo D, Tsutsumi S, Akasaka H, Jin H, Ohashi T, Muroya T, Hasebe T, et al. Gan To Kagaku Ryoho. 2009;36:2025–7. [Predictive factors for histopathological liver injury in the patients who received preoperative systemic chemotherapy for colorectal liver metastases] Japanese. [PubMed: 20037312](Abstract only: Among 47 patient undergoing hepatic resections for metastatic colorectal cancer, sinusoidal dilation but not steatohepatitis was more common among those who received preoperative oxaliplatin chemotherapy).
- van den Broek MA, Olde Damink SW, Driessen A, Dejong CH, Bemelmans MH. Nodular regenerative hyperplasia secondary to neoadjuvant chemotherapy for colorectal liver metastases. Case Rep Med. 2009;2009:457975. [PMC free article: PMC2787019] [PubMed: 19997518](Two men, ages 68 and 51 years, developed nodular regenerative hyperplasia after 6 cycles of oxaliplatin/capecitabine with minimal liver test abnormalities [bilirubin 2.3 and 1.2 mg/dL, ALT 23 and 57 U/L, Alk P 237 and 205 U/L], one dying of hepatic failure after partial hepatectomy of residual tumor, and the second developing variceal hemorrhage and encephalopathy after one resection but eventually recovering and tolerating a repeat hepatic resection 18 months later).
- Cleary JM, Tanabe KT, Lauwers GY, Zhu AX. Hepatic toxicities associated with the use of preoperative systemic therapy in patients with metastatic colorectal adenocarcinoma to the liver. Oncologist. 2009;14:1095–105. [PubMed: 19880627](Review of hepatic complications of oxaliplatin chemotherapy for colorectal cancer; sinusoidal dilation reported in 10-61% of patients sometimes with greater postoperative morbidity, but with no greater mortality).
- Slade JH, Alattar ML, Fogelman DR, Overman MJ, Agarwal A, Maru DM, Coulson RL, et al. Portal hypertension associated with oxaliplatin administration: clinical manifestations of hepatic sinusoidal injury. Clin Colorectal Cancer. 2009;8:225–30. [PubMed: 19822514](Six patients developed noncirrhotic portal hypertension after 6 to 12 cycles of oxaliplatin and 5-FU chemotherapy [6-15 months] for metastatic colorectal cancer, including 3 men, 3 women, ages 37 to 69 years, all of whom developed thrombocytopenia [53-128,000/µL], splenomegaly and varices, 2 with variceal hemorrhage and 2 with ascites).
- McDonald GB. Hepatobiliary complications of hematopoietic cell transplantation, 40 years on. Hepatology. 2010;51:1450–60. [PMC free article: PMC2914093] [PubMed: 20373370](Review of liver complications of bone marrow [hematopoietic cell] transplantation, which have become less frequent with better understanding of their causes and means of prevention; the rate of SOS has decreased because of avoidance of more aggressive ablative therapies [total body irradiation and high doses of cyclophosphamide] and better understanding of pharmacokinetics of the alkylating agents).
- Soubrane O, Brouquet A, Zalinski S, Terris B, Brézault C, Mallet V, Goldwasser F, Scatton O. Predicting high grade lesions of sinusoidal obstruction syndrome related to oxaliplatin-based chemotherapy for colorectal liver metastases: correlation with post-hepatectomy outcome. Ann Surg. 2010;251:454–60. [PubMed: 20160638](Among 78 patients undergoing resection of hepatic metastases from colon cancer after oxaliplatin neoadjuvant therapy, vascular changes occurred in 46 [59%] and 5 had fibrosis; AST elevations occurred in 61% of patients with vascular changes and 25% of those without).
- Pessaux P, Chenard MP, Bachellier P, Jaeck D. Consequences of chemotherapy on resection of colorectal liver metastases. J Visc Surg. 2010;147:e193–201. [PubMed: 20655821](Review of the role and liver toxicity of chemotherapy for colorectal metastases; oxaliplatin is associated with sinusoidal injury and irinotecan with chemotherapy induced steatohepatitis [CASH]).
- Takamoto T, Hashimoto T, Sano K, Maruyama Y, Inoue K, Ogata S, Takemura T, et al. Recovery of liver function after the cessation of preoperative chemotherapy for colorectal liver metastasis. Ann Surg Oncol. 2010;17:2747–55. [PubMed: 20425145](Indocyanine green [ICG] testing of 55 patients receiving chemotherapy before hepatic resection for colorectal cancer metastases showed improvements in ISG clearance within 4 weeks of stopping therapy).
- Ryan P, Nanji S, Pollett A, Moore M, Moulton CA, Gallinger S, Guindi M. Chemotherapy-induced liver injury in metastatic colorectal cancer: semiquantitative histologic analysis of 334 resected liver specimens shows that vascular injury but not steatohepatitis is associated with preoperative chemotherapy. Am J Surg Pathol. 2010;34:784–91. [PubMed: 20421779](Among 334 patients undergoing hepatic resection for colorectal cancer metastases, marked hepatic steatosis was uncommon [9%] and correlated with BMI rather than chemotherapy, while sinusoidal lesions were present in 35% of cases and correlated with oxaliplatin use; neither correlated with immediate operative outcome).
- Overman MJ, Maru DM, Charnsangavej C, Loyer EM, Wang H, Pathak P, Eng C, et al. Oxaliplatin-mediated increase in spleen size as a biomarker for the development of hepatic sinusoidal injury. J Clin Oncol. 2010;28:2549–55. [PubMed: 20406923](Spleen size as measured by CT increased [by an average of 22%] in 86% of 96 patients treated with oxaliplatin and 5FU for colorectal cancer and correlated with thrombocytopenia and sinusoidal injury seen on subsequent liver biopsy of 60 patients).
- Komori H, Beppu T, Baba Y, Horino K, Imsung C, Masuda T, Hayashi H, et al. Histological liver injury and surgical outcome after FOLFOX followed by a hepatectomy for colorectal liver metastases in Japanese patients. Int J Clin Oncol. 2010;15:263–70. [PubMed: 20238233](Comparison of 15 patients who received oxaliplatin to 12 who received no chemotherapy before hepatic resection of metastatic colorectal cancer showed higher rates of marked sinusoidal dilatation [33% vs 8%] and “blue liver” [47% vs 0%], but similar rates of steatosis [40% vs 33%] in oxaliplatin treated subjects).
- Heo J, Shin KY, Kwon YH, Park SY, Jung MK, Cho CM, Tak WY, Kweon YO. Korean J Gastroenterol. 2011;57:253–7. [A case of portal hypertension after the treatment of oxaliplatin based adjuvant chemotherapy for rectal cancer] Korean. [PubMed: 21519180](Abstract only: 35 year old woman developed portal hypertension after 12 cycles of oxaliplatin for rectal cancer).
- Makowiec F, Möhrle S, Neeff H, Drognitz O, Illerhaus G, Opitz OG, Hopt UT, zur Hausen A. Chemotherapy, liver injury, and postoperative complications in colorectal liver metastases. J Gastrointest Surg. 2011;15:153–64. [PubMed: 21061183](Among 102 patients undergoing hepatic resections for colorectal cancer metastases, steatosis was most common in those who had preoperative chemotherapy regardless of regimen [46% vs 18%], but BMI was a stronger risk factor and steatosis did not correlate with poor outcome; none of 22 patients who received oxaliplatin died or developed hepatic insufficiency).
- Tamandl D, Klinger M, Eipeldauer S, Herberger B, Kaczirek K, Gruenberger B, Gruenberger T. Sinusoidal obstruction syndrome impairs long-term outcome of colorectal liver metastases treated with resection after neoadjuvant chemotherapy. Ann Surg Oncol. 2011;18:421–30. [PubMed: 20844968](Among 199 patients undergoing hepatic resection for colorectal metastases, findings of hepatic steatosis did not correlate with decreased survival, whereas severe sinusoidal lesions [found in 18% of oxaliplatin recipients vs 6% of controls] were associated with markedly reduced survival).
- Vincenzi B, Daniele S, Frezza AM, Berti P, Vespasiani U, Picardi A, Tonini G. The role of S-adenosylmethionine in preventing oxaliplatin-induced liver toxicity: a retrospective analysis in metastatic colorectal cancer patients treated with bevacizumab plus oxaliplatin-based regimen. Support Care Cancer. 2012;20:135–9. [PubMed: 21229271](Among 78 patients with metastatic colon cancer who received 3 cycles of oxaliplatin, capecitabine and bevacizumab with or without S-adenosyl-methionine [SAMe], those on SAMe had lower peak ALT levels [98 vs 179 U/L] and less frequent discontinuations).
- Nam SJ, Cho JY, Lee HS, Choe G, Jang JJ, Yoon YS, Han HS, et al. Chemotherapy-associated hepatopathy in Korean colorectal cancer liver metastasis patients: oxaliplatin-based chemotherapy and sinusoidal injury. Korean J Pathol. 2012;46:22–9. [PMC free article: PMC3479708] [PubMed: 23109974](Among 89 patients with colorectal cancer undergoing hepatic resection for metastases, sinusoidal dilation, centrolobular fibrosis, small vessel obliteration and hepatocyte plate disruption were more frequent after oxaliplatin than fluorouracil chemotherapy and correlated with number of cycles).
- Viganò L, Ravarino N, Ferrero A, Motta M, Torchio B, Capussotti L. Prospective evaluation of accuracy of liver biopsy findings in the identification of chemotherapy-associated liver injuries. Arch Surg. 2012;147:1085–91. [PubMed: 22910896](Prospective study of 100 patients with colorectal cancer and hepatic metastases found liver biopsy was accurate in demonstrating marked steatosis [>30%] but not in detecting sinusoidal dilation [28% in oxaliplatin recipients] or steatohepatitis [19% in irinotecan recipients]).
- Robinson SM, Wilson CH, Burt AD, Manas DM, White SA. Chemotherapy-associated liver injury in patients with colorectal liver metastases: a systematic review and meta-analysis. Ann Surg Oncol. 2012;19:4287–99. [PMC free article: PMC3505531] [PubMed: 22766981](Systematic review of literature on chemotherapy induced liver injury in patients with colorectal cancer; oxaliplatin in regimens are associated with a higher rate of sinusoidal injury [17% vs 6%] but not steatosis [11.5% vs 9.8%], and rates are reduced by concurrent bevacizumab therapy).
- Vreuls CP, Van Den Broek MA, Winstanley A, Koek GH, Wisse E, Dejong CH, Olde Damink SW, et al. Hepatic sinusoidal obstruction syndrome (SOS) reduces the effect of oxaliplatin in colorectal liver metastases. Histopathology. 2012;61:314–8. [PubMed: 22571348](Among 50 patients with hepatic resection for colorectal cancer after 1 to 12 cycles [mean = 6] of oxaliplatin, 32 [64%] had changes of sinusoidal obstruction syndrome among whom tumor regression scores were reduced compared to patients without the sinusoidal histological changes; no discussion of survival).
- Robinson SM, White SA. Hepatic sinusoidal obstruction syndrome reduces the effect of oxaliplatin in colorectal liver metastases. Histopathology. 2012;61:1247–8. [PubMed: 23043422](Editorial in response to Vreuls [2012]).
- Bissonnette J, Généreux A, Côté J, Nguyen B, Perreault P, Bouchard L, Pomier-Layrargues G. Hepatic hemodynamics in 24 patients with nodular regenerative hyperplasia and symptomatic portal hypertension. J Gastroenterol Hepatol. 2012;27:1336–40. [PubMed: 22554152](Among 24 patients with various forms of nodular regenerative hyperplasia [NRH], wedged hepatic venous pressure gradients [HVPG: range 2 to 17, mean=8.9 mm Hg] were lower than directly obtained portal venous pressure gradients [range 16 to 35, mean=20.5 mmHg], indicating that HVPG measurements are inaccurate in NRH).
- Jardim DL, Rodrigues CA, Novis YA, Rocha VG, Hoff PM. Oxaliplatin-related thrombocytopenia. Ann Oncol. 2012;23:1937–42. [PubMed: 22534771](Review of thrombocytopenia related to oxaliplatin therapy which has three possible causes: myelosuppression, immune destruction or portal hypertension and liver disease).
- Pilgrim CH, Thomson BN, Banting S, Phillips WA, Michael M. The developing clinical problem of chemotherapy-induced hepatic injury. ANZ J Surg. 2012;82:23–9. [PubMed: 22507491](Review of types of liver injury from chemotherapy; oxaliplatin is associated with vascular and sinusoidal injury whereas irinotecan is linked to steatohepatitis).
- Narita M, Oussoultzoglou E, Chenard MP, Fuchshuber P, Rather M, Rosso E, Addeo P, et al. Liver injury due to chemotherapy-induced sinusoidal obstruction syndrome is associated with sinusoidal capillarization. Ann Surg Oncol. 2012;19:2230–7. [PubMed: 22402811](Among 98 patients with colorectal cancer undergoing hepatic resection for metastases, 39 [36 of whom had received oxaliplatin] had changes of SOS and degree of changes correlated with isocyanine green [ICG] retention and overexpression of CD34 indicating capillarization of hepatic sinusoids).
- Vietor NO, George BJ. Oxaliplatin-induced hepatocellular injury and ototoxicity: a review of the literature and report of unusual side effects of a commonly used chemotherapeutic agent. J Oncol Pharm Pract. 2012;18:355–9. [PubMed: 22333669](46 year old woman with colorectal cancer developed ototoxicity and marked ALT elevations [~850 U/L] during cycle 2 of fluorouracil, oxaliplatin and leucovorin, that resolved when oxaliplatin was held, and then recurred despite a reduced dose of oxaliplatin).
- Agostini J, Benoist S, Seman M, Julié C, Imbeaud S, Letourneur F, Cagnard N, et al. Identification of molecular pathways involved in oxaliplatin-associated sinusoidal dilatation. J Hepatol. 2012;56:869–76. [PubMed: 22200551](Analysis of differences in gene expression in livers of patients with and without sinusoidal dilation after oxaliplatin therapy identified increased expression of genes involved with angiogenesis, inflammation and collagen production in response to sinusoidal injury).
- Hoff PM, Saad ED, Costa F, Coutinho AK, Caponero R, Prolla G, Gansl RC. Literature review and practical aspects on the management of oxaliplatin-associated toxicity. Clin Colorectal Cancer. 2012;11:93–100. [PubMed: 22154408](Review of adverse effects of oxaliplatin including hepatotoxicity which appears to be due to sinusoidal cell injury).
- Tsimberidou AM, Leick MB, Lim J, Fu S, Wheler J, Piha-Paul SA, Hong D, et al. Dose-finding study of hepatic arterial infusion of oxaliplatin-based treatment in patients with advanced solid tumors metastatic to the liver. Cancer Chemother Pharmacol. 2013;71:389–97. [PubMed: 23143207](Among 76 patients with hepatic metastases of different cancers given hepatic artery infusions of oxaliplatin [369 cycles], 26 [34%] had ALT elevations [5% were >5 times ULN] and 11 [14%] had bilirubin elevations).
- van den Broek MA, Vreuls CP, Winstanley A, Jansen RL, van Bijnen AA, Dello SA, Bemelmans MH, et al. Hyaluronic acid as a marker of hepatic sinusoidal obstruction syndrome secondary to oxaliplatin-based chemotherapy in patients with colorectal liver metastases. Ann Surg Oncol. 2013;20(5):1462–9. [PubMed: 23463086](Among 40 patients with colorectal cancer undergoing hepatic resection for metastases after oxaliplatin based chemotherapy, 23 had SOS which was severe in 11 patients who had higher hyaluronic acid levels than the 29 with mild or no injury [52 vs 29 ng/mL]).
- Rahbari NN, Weitz J. Hyaluronic acid as a marker of sinusoidal obstruction syndrome after oxaliplatin-based chemotherapy for colorectal liver metastases: Don't forget the tumor. Ann Surg Oncol. 2013;20(5):1405–7. [PubMed: 23463087](Editorial in response to van den Broek [2013]).
- Hubert C, Sempoux C, Humblet Y, van den Eynde M, Zech F, Leclercq I, Gigot JF. Sinusoidal obstruction syndrome (SOS) related to chemotherapy for colorectal liver metastases: factors predictive of severe SOS lesions and protective effect of bevacizumab. HPB (Oxford). 2013;15(11):858–64. [PMC free article: PMC4503283] [PubMed: 23458554](Retrospective analysis of 151 patients with colorectal cancer and hepatic metastases; SOS occurred in 60 of 67 [90%] of those who received oxaliplatin and fluorouracil alone and was severe in 37 [55%], but arose in only 6 of 10 who received both oxaliplatin and bevacizumab and was severe in only 1 [10%]).
- Wolf PS, Park JO, Bao F, Allen PJ, DeMatteo RP, Fong Y, Jarnagin WR, et al. Preoperative chemotherapy and the risk of hepatotoxicity and morbidity after liver resection for metastatic colorectal cancer: a single institution experience. J Am Coll Surg. 2013;216:41–9. [PubMed: 23041049](Among 506 patients undergoing hepatic resection for colorectal cancer, histologic evaluation of non-tumor parenchyma showed that steatohepatitis was associated with irinotecan regimens, higher BMI and diabetes, whereas sinusoidal dilatation was not associated with chemotherapy; neither chemotherapy or liver histology correlated with complications or deaths).
- Urdzik J, Bjerner T, Wanders A, Duraj F, Haglund U, Norén A. Magnetic resonance imaging flowmetry demonstrates portal vein dilatation subsequent to oxaliplatin therapy in patients with colorectal liver metastasis. HPB (Oxford). 2013;15:265–72. [PMC free article: PMC3608980] [PubMed: 23458313](Prospective monitoring by magnetic resonance imaging found that oxaliplatin chemotherapy was associated with portal vein dilatation independent of sinusoidal injury, but that a combination of measurements of portal velocity and cross sectional area was predictive of the finding of sinusoidal injury).
- Béchade D, Désolneux G, Fonck M, Soubeyran I, Bécouarn Y, Evrard S. Presse Med. 2013;42:102–7. [Regenerative nodular hyperplasia of the liver related to oxaliplatin-based chemotherapy] [PubMed: 22770975](Two cases of NRH in a man and woman, age 60 years, with metastatic colorectal cancer after 17 and 12 courses of oxaliplatin based chemotherapy).
- Vreuls CP, Olde Damink SW, Koek GH, Winstanley A, Wisse E, Cloots RH, van den Broek MA, et al. Glutathione S-transferase M1-null genotype as risk factor for SOS in oxaliplatin-treated patients with metastatic colorectal cancer. Br J Cancer. 2013;108:676–80. [PMC free article: PMC3593549] [PubMed: 23287989](Among 55 patients with metastatic colorectal cancer who received oxaliplatin chemotherapy, the glutathione S-transferase [GST] M1-null polymorphism was frequent in those who developed moderate or severe sinusoidal injury [12 of 17: 70%] than in those with no or mild injury [13 of 38: 34%]).
- Ogata H, Gushima T, Maruoka S, Takasaki S, Tanaka R, Matsuura T, Aishima S, et al. A case of portal hypertension after 5-fluorouracil, leucovorin, and oxaliplatin (mFOLFOX6) chemotherapy. Nihon Shokakibyo Gakkai Zasshi. 2013;110:2119–26. [PubMed: 24305101](46 year old man developed noncirrhotic portal hypertension after 10 cycles of oxaliplatin and fluorouracil for colorectal cancer metastases, and required endoscopic ligation and transvenous obliteration of bleeding esophageal varices).
- Uchino K, Fujisawa M, Watanabe T, Endo Y, Nobuhisa T, Matsumoto Y, Kai K, et al. Oxaliplatin-induced liver injury mimicking metastatic tumor on images: a case report. Jpn J Clin Oncol. 2013;43:1034–8. [PubMed: 23958518](47 year old man developed radiologically apparent hepatic masses after 6 cycles of oxaliplatin and fluorouracil for metastatic colorectal cancer which, on resection, were not tumors but represented severe sinusoidal dilatation and congestion).
- Lu QY, Zhao AL, Deng W, Li ZW, Shen L. Hepatic histopathology and postoperative outcome after preoperative chemotherapy for Chinese patients with colorectal liver metastases. World J Gastrointest Surg. 2013;5:30–6. [PMC free article: PMC3615301] [PubMed: 23556058](Retrospective analysis of 106 patients undergoing hepatic resection for colorectal cancer at a single Chinese medical center over a 10 year period, found that oxaliplatin based regimens were associated with sinusoidal dilation [42%] compared to surgery only controls [21%], but perioperative complication rates were similar).
- Nguyen-Khac E, Lobry C, Chatelain D, Fuks D, Joly JP, Brevet M, Tramier B, et al. A Reappraisal of chemotherapy-induced liver injury in colorectal liver metastases before the era of antiangiogenics. Int J Hepatol. 2013;2013:314868. [PMC free article: PMC3606725] [PubMed: 23533786](Among 50 patients with colorectal cancer undergoing hepatectomy after chemotherapy, 55% of those who received oxaliplatin developed sinusoidal dilatation and 23% had evidence of NRH compared to 23% and 6% of controls; however, there was no difference in overall mortality or outcomes).
- Schwarz RE, Berlin JD, Lenz HJ, Nordlinger B, Rubbia-Brandt L, Choti MA. Systemic cytotoxic and biological therapies of colorectal liver metastases: expert consensus statement. HPB (Oxford). 2013;15:106–15. [PMC free article: PMC3719916] [PubMed: 23297721](Summary of current optimal therapies of patients with colorectal liver metastases and the problem of chemotherapy associated liver injury, particularly to oxaliplatin [SOS, NRH] and irinotecan [steatosis] leading to recommendation that, if possible, preoperative chemotherapy be limited to 3 months).
- Morine Y, Shimada M, Utsunomiya T. Evaluation and management of hepatic injury induced by oxaliplatin-based chemotherapy in patients with hepatic resection for colorectal liver metastasis. Hepatol Res. 2014;44:59–69. [PubMed: 23551330](Review of the frequency, clinical significance and management of hepatic effects of oxaliplatin therapy in patients undergoing liver resection for colorectal cancer metastases).
- Morris-Stiff G, White AD, Gomez D, Cameron IC, Farid S, Toogood GJ, Lodge JP, et al. Nodular regenerative hyperplasia (NRH) complicating oxaliplatin chemotherapy in patients undergoing resection of colorectal liver metastases. Eur J Surg Oncol. 2014;40:1016–20. [PubMed: 24370284](Retrospective review of 978 patients who underwent hepatic resection for colorectal cancer metastases at a single institution in the UK between 2000 and 2010, identified 5 who developed clinically apparent NRH, all had received at least 6 cycles of oxaliplatin and fluorouracil, but only 1 had hepatic failure which was reversible and the all deaths [n=4] were due to cancer recurrence).
- Seo AN, Kim H. Sinusoidal obstruction syndrome after oxaliplatin-based chemotherapy. Clin Mol Hepatol. 2014;20:81–4. [PMC free article: PMC3992335] [PubMed: 24757663](58 year old Korean woman with metastatic colon cancer underwent 6 cycles of chemotherapy with capecitabine and oxaliplatin and subsequent hemihepatectomy, the normal liver showing marked SOS despite normal liver tests [bilirubin 0.8 mg/dL, ALT 12 U/L, Alk P 60 U/L, INR 1.1] indicating the frequent silent nature of SOS).
- Nalbantoglu IL, Tan BR Jr, Linehan DC, Gao F, Brunt EM. Histological features and severity of oxaliplatin-induced liver injury and clinical associations. J Dig Dis. 2014;15:553–60. [PubMed: 25060628](Among 47 patients with metastatic colon cancer undergoing liver resection after oxaliplatin based chemotherapy, 32 [68%] had changes indicative of SOS [using a scoring system of 0 to 4], which was moderate or severe in 26 [55%] and usually associated with serum aminotransferase abnormalities; liver also showing capillarization, sinusoidal fibrosis and hepatocyte proliferation).
- Tajima H, Ohta T, Miyashita T, Nakanuma S, Matoba M, Miyata T, Sakai S, et al. Oxaliplatin-based chemotherapy induces extravasated platelet aggregation in the liver. Mol Clin Oncol. 2015;3:555–8. [PMC free article: PMC4471568] [PubMed: 26137266](Analysis of 32 patients with metastatic colorectal cancer undergoing hepatic resection demonstrated lower platelet counts [167,000 vs 227,000/µL], larger spleen volumes, and prominent aggregation of platelets in zone 3 in those who had received adjuvant oxaliplatin [n=17] vs controls [n=15]).
- Viganò L, Rubbia-Brandt L, De Rosa G, Majno P, Langella S, Toso C, Mentha G, et al. Nodular regenerative hyperplasia in patients undergoing liver resection for colorectal metastases after chemotherapy: risk factors, preoperative assessment and clinical impact. Ann Surg Oncol. 2015;22:4149–57. [PubMed: 25845431](Among 406 patients undergoing 478 liver resections for metastatic colorectal cancer at two European medical centers between 2015 and 2017, 68% had sinusoidal dilatation, 25% had steatosis, 10% had steatohepatitis and 18% had NRH, risk factors for NRH being preoperative oxaliplatin and low platelet counts but not routine liver test abnormalities).
- Choi JH, Won YW, Kim HS, Oh YH, Lim S, Kim HJ. Oxaliplatin-induced sinusoidal obstruction syndrome mimicking metastatic colon cancer in the liver. Oncol Lett. 2016;11:2861–4. [PMC free article: PMC4812530] [PubMed: 27073565](22 year old woman with resected colon cancer presented after 5 cycles of adjuvant chemotherapy with minor liver test abnormalities [bilirubin 0.6 mg/dL, ALT 51 U/L, Alk P 105 U/L] and enlarging nodular hepatic lesions on abdominal CT which at surgery were areas of dark red congested liver which represented areas of severe SOS histologically).
- Stevenson HL, Prats MM, Sasatomi E. Chemotherapy-induced sinusoidal injury (CSI) score: a novel histologic assessment of chemotherapy-related hepatic sinusoidal injury in patients with colorectal liver metastasis. BMC Cancer. 2017;17:35. [PMC free article: PMC5219653] [PubMed: 28061766](Immunohistochemistry done on 30 liver samples from hepatic resections for metastatic colorectal cancer found aberrant CD34 staining [marker for platelets] more frequently in 22 cases with SOS vs 8 controls [82% vs 25%] as well as multifocal increases in smooth muscle actin staining [72% vs 25%] and glutamine synthetase staining [32% vs none]; the combination of the 3 stains being possibly helpful in diagnosis of SOS).
- Vigano L, De Rosa G, Toso C, Andres A, Ferrero A, Roth A, Sperti E, et al. Reversibility of chemotherapy-related liver injury. J Hepatol. 2017;67:84–91. [PubMed: 28284915](Among 15 patients with colorectal cancer who underwent two hepatic resections more than 270 days apart without interval chemotherapy, SOS regressed in 4 of 5 patients who had SOS initially and NRH in 7 of 8 patients, whereas neither steatosis [3 of 3] or steatohepatitis [2 of 2] resolved).
- Duwe G, Knitter S, Pesthy S, Beierle AS, Bahra M, Schmelzle M, Schmuck RB, et al. Hepatotoxicity following systemic therapy for colorectal liver metastases and the impact of chemotherapy-associated liver injury on outcomes after curative liver resection. Eur J Surg Oncol. 2017;43:1668–81. [PubMed: 28599872](Review of the hepatotoxicity of chemotherapies for metastatic colorectal cancer, focusing on fluorouracil [steatosis], irinotecan [steatohepatitis] and oxaliplatin [SOS] and including analysis of the contribution of anti-EGFR antibodies and bevacizumab on both efficacy and safety).
- Wakiya T, Kudo D, Ishido K, Kimura N, Yakoshi Y, Toyoki Y, Kijima H, et al. Effect of age on the development of chemotherapy-associated liver injury in colorectal cancer liver metastasis. Mol Clin Oncol. 2017;7:200–4. [PMC free article: PMC5532632] [PubMed: 28781785](Among 64 patients with metastatic colorectal cancer receiving oxaliplatin-based adjuvant chemotherapy, sinusoidal injury occurred in 27-30% and steatohepatitis in 35-40% of patients, rates being similar in all age groups).
- Bernichon E, Daguenet E, Molla C, Cornillon J, Lejeune C, Casteillo F, Guyotat D, et al. Sinusoidal obstruction syndrome/veno-occlusive disease complication in lymphoma patients treated with oxaliplatin-based regimen: A case series report. Curr Res Transl Med. 2018;66:107–10. [PubMed: 29519713](Among 49 patients with lymphoma receiving autologous hematopoietic cell transplantation over a 2 year period at a single, French referral center, 4 of 19 who had received oxaliplatin-based cycles of chemotherapy developed severe SOS within 2-9 days compared to none of 30 who did not receive oxaliplatin).
- Shigefuku R, Watanabe T, Mizukami T, Matsunaga K, Hattori N, Ehira T, Suzuki T, et al. Esophagogastric varices were diagnosed in a non-cirrhotic liver case during long-term follow-up after oxaliplatin-based chemotherapy. Clin J Gastroenterol. 2018;11:487–92. [PubMed: 29948819](78 year old Japanese man presented with esophageal varices and splenomegaly 3.5 years after receiving 10 cycles of oxaliplatin and fluorouracil for metastatic colorectal cancer [bilirubin1.0, ALT 16 U/L, Alk P 269 U/L, platelets 65,000/µL], liver biopsy showing no evidence of fibrosis).
- Overman MJ, Ferrarotto R, Raghav K, George B, Qiao W, Machado KK, Saltz LB, et al. The addition of bevacizumab to oxaliplatin-based chemotherapy: impact upon hepatic sinusoidal injury and thrombocytopenia. J Natl Cancer Inst. 2018;110:888–94. [PubMed: 29346573](Among 184 patients with metastatic colorectal cancer treated with adjuvant fluorouracil and oxaliplatin with or without bevacizumab, the rate of splenomegaly and thrombocytopenia in follow up was less in those receiving bevacizumab).
- Gutierrez L, Méndez S, Mitjavila M, Llop E, Salas C, Ruiz-Casado A. Noncirrhotic portal hypertension: an under-reported late adverse event of SIRT in metastatic colorectal cancer patients. J Cancer Res Ther. 2019;15:42–7. [PubMed: 30880753](Three patients with metastatic colorectal cancer developed noncirrhotic portal hypertension after cycles of fluorouracil and oxaliplatin and then selective internal radiation therapy with 90-yttrium-radiolabeled microspheres, two later dying of hepatic failure).
- Corbacioglu S, Jabbour EJ, Mohty M. Risk factors for development of and progression of hepatic veno-occlusive disease/sinusoidal obstruction syndrome. Biol Blood Marrow Transplant. 2019;25:1271–80. [PubMed: 30797942](Review of the risks, clinical features and management of chemotherapy induced SOS focusing upon oxaliplatin and the more recent causes, gemtuzumab ozogamicin and inotuzumab ozogamicin).
- Hisaka T, Ishikawa H, Sakai H, Kawahara R, Goto Y, Nomura Y, Yasunaga M, et al. Sinusoidal obstruction syndrome and postoperative complications resulting from preoperative chemotherapy for colorectal cancer liver metastasis. Anticancer Res. 2019;39:4549–54. [PubMed: 31366558](Among 90 cases of metastatic colorectal cancer treated with adjuvant chemotherapy before hepatic resection, rates of sinusoidal injury in the resected nontumorous liver were similar in those who received no monoclonal antibody vs bevacizumab or cetuximab or panitumumab [50% to 51%], but the degree of injury appeared less with bevacizumab).
- Wilcox MA, Hardin J, Weaver J, Voss EA. Liver test monitoring: real-world compliance for drugs with monitoring requirements at 2-week intervals or more frequently. Pharmaceut Med. 2019;33:389–94. [PubMed: 31933226](Analysis of 3 large health databases for compliance with recommendations for liver test monitoring when initiating therapy with 9 drugs found compliance was highest for oxaliplatin [75%], somewhat lower for rifampin [68%], tolcapone [67%], albendazole [66%] and azathioprine [61%], and poor for pentamidine [21%], felbamate [22%], succimer [29%] and ketoconazole [32%]).
- Fujii A, Tateoka T, Okuyama T, Matsushima J, Sato T, Ono Y, Ban S. Uneven distribution of histologic changes of "blue liver" induced after oxaliplatin-based chemotherapy for colon cancer. Int J Surg Pathol. 2020;28:523–5. [PubMed: 31623475](50 year old woman with metastatic colorectal cancer underwent 8 courses of oxaliplatin and capecitabine followed by hepatic resection that revealed mottled red areas of the nontumorous liver with changes of SOS).
- Honda S, Tsujimoto M, Minegaki T, Mori T, Muraoka J, Nishiguchi K. A case of idiosyncratic liver injury after oxaliplatin-induced thrombocytopenia. J Clin Pharm Ther. 2020;45:373–5. [PubMed: 31671217](46 year old woman with metastatic colorectal carcinoma experienced an anaphylactic reaction to a second infusion of oxaliplatin with subsequent abnormal liver tests [bilirubin 0.8 rising to 1.4 mg/dL, ALT 110 to 1010 U/L, Alk P 281 to 313 U/L], with profound thrombocytopenia [7000/µL] and rapid resolution within 2-3 weeks with prednisone therapy).
- Puente A, Fortea JI, Del Pozo C, Huelin P, Cagigal ML, Serrano M, Cabezas J, et al. Porto-sinusoidal vascular disease associated to oxaliplatin: an entity to think about it. Cells. 2019;8:1506. [PMC free article: PMC6952805] [PubMed: 31771307](Review of NRH arising after oxaliplatin therapy including possible pathogenesis, criteria for diagnosis and recommendations for management).
- Debureaux PE, Febvre de Nailly DL, Tavernier E, Bedoui M, Kuhnowski F, Tamburini J, et al. Sinusoidal obstruction syndrome: a warning about autologous stem cell transplantation preceded by regimens containing oxaliplatin. Bone Marrow Transplant. 2020;55:1834–6. [PubMed: 31959893](Among 23 patients with SOS after autologous HCT for lymphoma identified in a French national survey, 21 had received oxaliplatin compared to only 13 of 23 matched controls).
- Eren T, Pasaoglu L. Splenomegaly in colon cancer during adjuvant oxaliplatin-based chemotherapy. Cureus. 2020;12:e7230. [PMC free article: PMC7145381] [PubMed: 32280572](Among 50 patients with metastatic colorectal cancer who received fluorouracil and oxaliplatin between 2015 and 2017, 50% developed splenomegaly [>50% increase in spleen size by CT], which correlated best with total oxaliplatin dose received and development of thrombocytopenia after therapy).
- Morioka D, Izumisawa Y, Yamaguchi K, Sato K, Komiyama S, Nakagawa K, Kakizoe M, et al. Surgical intervention for portal hypertension caused by oxaliplatin-based chemotherapy: a case report and a review of literature regarding radiological and/or surgical interventions for oxaliplatin-associated portal hypertension. Clin J Gastroenterol. 2020 Jun 26; Epub ahead of print. [PMC free article: PMC7519904] [PubMed: 32592150](63 year old man developed recurrent variceal hemorrhage, ascites and hydrothorax after oxaliplatin therapy of metastatic colon cancer followed by hepatic resection who was treated with splenectomy and portocaval shunt, with resolution of the complications of portal hypertension).
- Al-Qudah G, Ghanem M, Blebea J, Shaheen S. Blue liver: case report of blue liver. Am J Case Rep. 2020;21:e923553. [PMC free article: PMC7423174] [PubMed: 32738134](39 year old man with acute cholestatic liver disease of unknown cause [bilirubin 14 to 21 mg/dL, ALT 185 U/L, Alk P 150 U/L INR 1.2] was found to have a blue liver on laparoscopic cholecystectomy, later improving on long term ursodiol therapy; no exposure to oxaliplatin and blue color not explained; jaundice possibly due to unacknowledged anabolic steroid use).
- Di Federico A, Nuvola G, Sisi M, Lenzi B, Nobili E, Campana D. Hyperammonemic encephalopathy during XELOX regimen. is it capecitabine or oxaliplatin responsible? Anticancer Drugs. 2020 Aug 19; Epub ahead of print. [PubMed: 32826413](65 year old man with refractory metastatic lung carcinoid tumor developed confusion and coma 11 days into a 3-week regimen of capecitabine [1.6 mg/m2 daily for 15 days] and oxaliplatin [104 mg/m2 on day 1] with ammonia of 167 µmol/L but normal bilirubin and aminotransferase levels, resolving within 3 days of stopping capecitabine).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Platinum Coordination Complexes.[LiverTox: Clinical and Researc...]Review Platinum Coordination Complexes.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Azathioprine.[LiverTox: Clinical and Researc...]Review Azathioprine.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Porto-Sinusoidal Vascular Disease Associated to Oxaliplatin: An Entity to Think about It.[Cells. 2019]Review Porto-Sinusoidal Vascular Disease Associated to Oxaliplatin: An Entity to Think about It.Puente A, Fortea JI, Del Pozo C, Huelin P, Cagigal ML, Serrano M, Cabezas J, Arias Loste MT, Iruzubieta P, Cuadrado A, et al. Cells. 2019 Nov 24; 8(12). Epub 2019 Nov 24.
- The Clinical Spectrum and Diagnosis of Oxaliplatin Liver Injury in the Era of Nonalcoholic Fatty Liver Disease.[Clin Gastroenterol Hepatol. 2021]The Clinical Spectrum and Diagnosis of Oxaliplatin Liver Injury in the Era of Nonalcoholic Fatty Liver Disease.Kim HP, Navarro V, Zacks S, Odin J, Kleiner DE, Hayashi PH, Drug-Induced Liver Injury Network Investigators. Clin Gastroenterol Hepatol. 2021 Oct; 19(10):2199-2201. Epub 2020 Sep 30.
- A Case Report of Nodular Regenerative Hyperplasia and Non-cirrhotic Portal Hypertension Post Oxaliplatin Chemotherapy.[Cureus. 2022]A Case Report of Nodular Regenerative Hyperplasia and Non-cirrhotic Portal Hypertension Post Oxaliplatin Chemotherapy.Ganta N, Prasad A, Aknouk M, Ghodasara K, Nair A, Taqvi Z, Cheriyath P. Cureus. 2022 Sep; 14(9):e28740. Epub 2022 Sep 3.
- Oxaliplatin - LiverToxOxaliplatin - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...