Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
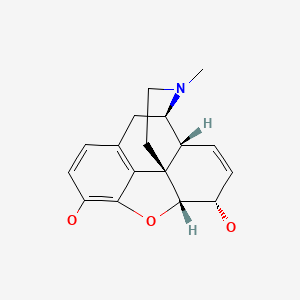
CASRN: 57-27-2
Drug Levels and Effects
Summary of Use during Lactation
Epidural morphine given to mothers for postcesarean section analgesia results in trivial amounts of morphine in their colostrum and milk. Intravenous or oral doses of maternal morphine in the immediate postpartum period result in higher milk levels than with epidural morphine. Labor pain medication may delay the onset of lactation. Maternal use of oral opioids during breastfeeding can cause infant drowsiness, which may progress to rare but severe central nervous system depression, although low-dose morphine might be preferred over other opiates.[1] Newborn infants seem to be particularly sensitive to the effects of even small dosages of narcotic analgesics. If morphine is required by the mother of a newborn, it is not a reason to discontinue breastfeeding; however, once the mother's milk comes in, it is best to provide pain control with a nonnarcotic analgesic and limit maternal intake of morphine to 2 to 3 days at a low dosage with close infant monitoring, especially in the outpatient setting.[2] If the baby shows signs of increased sleepiness (more than usual), difficulty breastfeeding, breathing difficulties, or limpness during maternal morphine use, a physician should be contacted immediately. Some evidence suggests that IV ketorolac, oral ibuprofen and acetaminophen as part of a multimodal post-cesarean section analgesia reduces percentage of mothers who fail exclusive breastfeeding compared to patient-controlled IV morphine-based analgesia.[3]
Drug Levels
Morphine is metabolized to inactive morphine-3-glucuronide (60%) and to active morphine-6-glucuronide (10%). Morphine has an oral bioavailability of about 30% in adults. Morphine-6-glucuronide has an oral bioavailability of about 4%, but probably can be converted back to morphine in the infant's gut and absorbed as morphine. The plasma clearance of morphine is prolonged in very young infants compared to older infants and children. Usual therapeutic intravenous doses of morphine in infants are 10 mcg/kg/hour or 50 to 100 mcg/kg as a single dose. Usual single oral doses of morphine in infants are 100 to 500 mcg/kg.
Maternal Levels. Five lactating mothers who were at least 1 month postpartum were given 1 to 2 doses of either epidural 4 mg or parenteral (intravenous or intramuscular) 5 to 15 mg morphine every 4 to 6 hours for postoperative analgesia. Milk was sampled from each mother 10 times over the 8 hours after her dose. The peak milk level after epidural morphine was 82 mcg/L and occurred 30 minutes after a second dose. The peak milk level after parenteral morphine was about 500 mcg/L and occurred about 45 minutes after a single 15 mg (10 mg intravenous plus 5 mg intramuscular) dose. The half-life in milk was about 3 hours.[4] Using the peak milk levels from this study, an exclusively breastfed infant would receive 75 mcg/kg daily.
Six women who received epidural morphine 5 mg for labor analgesia had their initial colostrum sampled postpartum (range 24-100 hours after epidural). Morphine was undetectable (<0.6 mcg/L) in 4 of the women. The peak morphine level was 4.5 mcg/L and was measured 28 hours after the epidural dose.[5] Considering the small amount of colostrum consumed by the infant, based on the peak level in this study, an exclusively breastfed infant would only receive a negligible amount of morphine from a maternal epidural 5 mg morphine dose for labor analgesia.
Five mothers who had undergone cesarean section delivery at term were given intravenous morphine 7.5 mg after umbilical cord clamping and then 1 to 1.5 mg every 6 minutes via intravenous patient-controlled analgesia (PCA) as needed for up to 48 hours postpartum. When PCA morphine was discontinued, oral morphine 5-30 mg every 2 to 3 hours as needed was given. Colostrum and milk were sampled from each of the mothers 6 times over 96 hours postpartum. Average milk levels from all the mothers studied were about 50 to 65 mcg/L in the first 48 hours postpartum and then dropped to about 20 mcg/L by 72 to 96 hours postpartum. The average cumulative intravenous only dose in the first 48 hours postpartum was about 150 mg. The average cumulative intravenous plus oral morphine dose over the entire 96 hours was about 250 mg.[6] Using the average milk levels reported at each of the 6 collection times from this study, an exclusively breastfed infant would receive about 5 mcg/kg daily. Using the maximum level of 65 mcg/L reported in the first 48 hours postpartum when mothers were receiving intravenous morphine, and assuming 30% oral absorption by the infant, an exclusively breastfed infant would absorb a maximum of about 3 mcg/kg daily equal to 0.3% of the intravenous maternal weight-adjusted daily dosage.
One mother who was 21 days postpartum received oral morphine 10 mg every 6 hours for 4 doses then 5 mg every 6 hours for 2 doses. She had a peak morphine breastmilk level of 100 mcg/L at 1 hour after breastfeeding and 4.5 hours after her first 5 mg dose.[7] Using the peak milk level from this study, an exclusively breastfed infant would receive 15 mcg/kg daily, equal to about 3% of the maternal daily dosage, assuming a daily maternal oral morphine dose of 40 mg.
Epidural morphine 5 mg was given to 30 women immediately following cesarean section and again 24 hours later. There were measurable colostrum morphine levels 12 to 36 hours after delivery in only 3 of the women (range 0.39 to 0.66 mcg/L). The remaining 27 women had undetectable (<0.12 mcg/L) morphine milk levels.[8]
One breastfeeding woman receiving 4 to 8 mg daily of continuous intrathecal morphine had her milk sampled 11 times over 7 weeks postpartum. Levels in milk were undetectable (<8 mcg/L) in 8 of the 11 samples. In 3 of the 11 samples, morphine was detected, but only at levels below the quantification sensitivity of the assay (8 to 25 mcg/L) and was not related to maternal dose.[9] Using the maximum possible milk level of 25 mcg/L from this study, an exclusively breastfed infant would receive about 3 mcg/kg daily from this maternal intrathecal morphine dose regimen.
Seven women who had preterm infants delivered by cesarean section were started on intravenous morphine 7 to 10 mg over 30 to 60 minutes, then 1 mg every 10 minutes by patient-controlled analgesia (PCA) as needed, for up to 48 hours postpartum. Colostrum samples were taken just prior to PCA initiation and again at 12, 24, 36, and 48 hours postpartum. The average cumulative morphine dose was about 60 mg in 48 hours. Three of the women could not produce enough milk for sampling. Morphine and its active 6-glucuronide metabolite were detectable in 3 of the remaining 4 women. There was high intersubject variability with peak milk levels occurring at different times and a wide range of levels measured in each of the women. The peak milk morphine level was 48 mcg/L and the peak 6-glucuronide metabolite level was 1,084 mcg/L. The authors reported median morphine levels of 34, 24, 7, 6.5 and 21 mcg/L and 6-glucuronide levels of 273, 672, 426, 527 and 350 mcg/L at 0, 12, 24, 36 and 48 hours, respectively.[10] Using the reported median milk levels from the 60 mg cumulative 48 hour maternal morphine dose in this study, an exclusively breastfed infant would receive 2.4 mcg/kg daily of morphine and 73 mcg/kg daily of the 6-glucuronide metabolite. Using the peak milk level data from this study, an exclusively breastfed infant would receive an estimated maximum of 7.2 mcg/kg daily of morphine and 163 mcg/kg daily of the 6-glucuronide metabolite.
Twelve women who underwent cesarean section deliveries at 37 to 41 weeks of gestation received a single dose of 2 mg of morphine epidurally. Colostrum was collected several times during the first 24 hours postpartum. The highest average morphine concentration was reported to be 6.2 mg/L and occurred in colostrum 3.2 hours after the cesarean section. The morphine concentration fell with an average half-life of 2.9 hours. By 6 hours after the dose, the reported concentration was 1.1 mg/L. By 24 hours, the drug was undetectable in colostrum.[11] Note: it is likely that this paper reported the milk concentration values in the wrong units. The values reported were probably in mcg/L, not mg/L.
Infant Levels. In a term infant, the measured plasma morphine level was 1.2 mcg/L. The measurement was taken 108 hours after the mother's last dose of morphine and no morphine was detected in her milk. The mother's dose was not reported.[12]
One mother of a term 21-day-old breastfeeding infant received a 10-day tapering dose of oral morphine beginning with 50 mg every 6 hours. On day 9 she received 10 mg every 6 hours, then 5 mg every 6 hours on day 10. The infant's serum morphine level was 4 mcg/L measured 1 hour after breastfeeding and 4 hours after the first 5 mg dose on day 10. Because this serum level occurred while the mother was taking a lower morphine dose, the authors surmised that the infant likely had serum milk levels in what they considered a therapeutic range of over 20 mcg/L during the time the mother was taking higher morphine doses.[7]
Effects in Breastfed Infants
In a term infant with unexplained apnea and bradycardia with cyanosis while hospitalized in the first week of life, the measured plasma morphine in the infant was 1.2 mcg/L. The measurement was taken 108 hours after the mother's last dose of morphine and no morphine was detected in her milk. The mother's dose was not reported.[12]
Breastfed newborns of mothers using intravenous PCA morphine for postcesarean analgesia were more alert and better oriented after postpartum day 3 than infants of mothers using intravenous PCA meperidine and nonbreastfed control infants. There was no difference in newborn respiratory rates. The authors stated that the mothers of nonbreastfed infants had greater parity than the breastfeeding mothers which, combined with a presumed lower desire to breastfeed, may have contributed to the lower behavioral and alertness scores in the nonbreastfed newborns.[6,13]
A study of pregnant women being treated for opiate dependency with slow-release oral morphine at a clinic in Vienna were followed as were their newborn infants. Compared to infants who were not breastfed (n = 91), breastfed infants (n = 21) had lower average measures of neonatal abstinence, lower dosage requirements of morphine (5.23 mg vs 8.75 mg), shorter durations of treatment for neonatal abstinence (10.2 vs 18.1 days) and shorter hospital stays (19.7 vs 31 days).[14]
A search was performed of the shared database of all U.S. poison control centers for the time period of 2001 to 2017 for calls regarding medications and breastfeeding. Of 2319 calls in which an infant was exposed to a substance via breastmilk, 7 were classified as resulting in a major adverse effect, and one of these involved morphine. A one-month-old infant was exposed to fentanyl, morphine, oxycodone, and unspecified benzodiazepines. The infant was admitted to the intensive care unit and described as being agitated and irritable and having tachycardia, confusion, drowsiness, lethargy, miosis, respiratory depression, acidosis, and hyperglycemia. The dosages, routes of administration, and extent of breastfeeding were not reported and the infant survived.[15]
An infant was born to a mother with opioid use disorder who was taking up to 2 grams of intravenous fentanyl daily. In the hospital she was transitioned to intravenous hydromorphone 120 mg three times daily, oral hydromorphone 32 mg every hour as needed, and methadone 70 mg daily by mouth. After 9 days of tapering the oral morphine dosage, the infant was given 72 mL of the mother’s expressed milk. On day 10, the infant received two doses of 0.1 mg of oral morphine and then breastfed for 30 minutes 3 hours after a maternal dose of 110 mg of intravenous hydromorphone. The infant was alert and active, feeding and sleeping well, and the infant’s morphine was discontinued. There were no clinically relevant episodes of apnea, bradycardia, desaturation, signs of respiratory depression, or excessive sedation. The infant continued to receive formula plus either breastfeeding or expressed milk with no clinically important adverse effects. The mother’s hydromorphone dose was tapered over 47 days while oral methadone and oral slow-release morphine were increased to 190 mg and 1200 mg daily, respectively, and she was discharged on day 58 postpartum. The extent of breastfeeding after hospital discharge was not reported. At 4 months of age, the infant scored above average on all developmental domains.[16]
In population study in the province of Ontario, Canada, 85,852 who filled an opioid prescription within seven days of discharge after delivery were matched to 538,815 did not. Compared with infants born to mothers who were not prescribed an opioid, those born to mothers prescribed an opioid were no more likely to be admitted to hospital in the 30 days after the index date. Infants born to mothers prescribed opioids after delivery were slightly more likely to be taken to the emergency department in the subsequent 30 days (hazard ratio 1.04). No infant deaths occurred. Nineteen percent of the mothers prescribed an opioid were prescribed morphine. Of note is that the median drug supply was for 3 days (IQR 2-4).[17]
Effects on Lactation and Breastmilk
Morphine can increase serum prolactin.[18] However, the prolactin level in a mother with established lactation may not affect her ability to breastfeed.
A national survey of women and their infants from late pregnancy through 12 months postpartum compared the time of lactogenesis II in mothers who did and did not receive pain medication during labor. Categories of medication were spinal or epidural only, spinal or epidural plus another medication, and other pain medication only. Women who received medications from any of the categories had about twice the risk of having delayed lactogenesis II (>72 hours) compared to women who received no labor pain medication.[19]
A randomized, blinded study in 250 women receiving a cesarean section at term compared the effects on breastfeeding of postpartum intrathecal morphine 300 to 500 mcg to a control group who received a non-opiate for pain. Systemic morphine or meperidine could be given to control mothers for severe breakthrough pain. All mothers also received midazolam 2 mg after cord clamping and oxytocin. At 2 months of age, there was no difference in the breastfeeding rates between the two groups, although infant weight gain was about 5% lower in the spinal morphine group.[20]
A prospective study in an Australian hospital compared mothers who received epidural fentanyl analgesia, subcutaneous morphine or neither during labor and delivery. When controlled for labor induction, instrumental delivery and special care nursery admission, no difference was seen between the 3 groups in breastfeeding rates at discharge or at 6 weeks postpartum.[21]
A multicenter, prospective cohort study in Hong Kong of 1277 women who gave birth found that women who received epidural analgesia with either fentanyl or morphine had no decreased frequency breastfeeding in the first hour compared to mothers who did not receive epidural analgesia. All epidural injections were combined with a local anesthetic, but the exact dosages were not given.[22]
A prospective cohort study of postcesarean pain control compared (1) morphine PCA and scheduled ibuprofen for the first 12 hours followed by continued scheduled ibuprofen with hydrocodone-acetaminophen as needed to a multimodal pain management regimen consisting of (2) acetaminophen 1000 mg orally every 8 hours, ketorolac 30 mg IV once initially, then 15 mg IV every 8 hours for 24 hours, then ibuprofen 600 mg orally every 8 hours for the remainder of the postoperative course with opioids given only as needed. Of women who planned to exclusively breastfeed on admission, fewer women used formula prior to discharge in the multimodal group compared to the traditional group (9% vs. 12%).[3]
A study compared 2 mg of epidermal morphine to saline given within 1 hour after vaginal delivery. No differences were found between the two groups in the rates of any breastfeeding or exclusive breastfeeding at 1 or 6 weeks postpartum.[23]
Alternate Drugs to Consider
(Analgesia) Acetaminophen, Butorphanol, Fentanyl, Hydromorphone, Ibuprofen
References
- 1.
- Lamvu G, Feranec J, Blanton E. Perioperative pain management: An update for obstetrician-gynecologists. Am J Obstet Gynecol 2018;218:193-9. [PubMed: 28666699]
- 2.
- Ito S. Opioids in breast milk: Pharmacokinetic principles and clinical implications. J Clin Pharmacol 2018;58 (Suppl 10):S151-S63. [PubMed: 30248201]
- 3.
- Macias DA, Adhikari EH, Eddins M, et al. A comparison of acute pain management strategies after cesarean delivery. Am J Obstet Gynecol 2021;226(3):407.e1-407.e7. [PubMed: 34534504]
- 4.
- Feilberg VL, Rosenborg D, Broen Christensen, C, et al. Excretion of morphine in human breast milk. Acta Anaesthesiol Scand 1989;33:426-8. [PubMed: 2800981]
- 5.
- Bernstein J, Patel N, Moszczynski Z, et al. Colostrum morphine concentrations following epidural administration. Anesth Analg 1989;68:S23. https://journals
.lww .com/anesthesia-analgesia/toc/1989/02001 - 6.
- Wittels B, Scott DT, Sinatra RS. Exogenous opioids in human breast milk and acute neonatal neurobehavior: A preliminary study. Anesthesiology 1990;73:864-9. [PubMed: 2240676]
- 7.
- Robieux I, Koren G, Vandenbergh H, et al. Morphine excretion in breast milk and resultant exposure of a nursing infant. J Toxicol Clin Toxicol 1990;28:365-70. [PubMed: 2231835]
- 8.
- Zakowski MI, Ramanathan S, Turndorf H. A two-dose epidural morphine regimen in cesarean section patients: Pharmacokinetic profile. Acta Anaesthesiol Scand 1993;37:584-9. [PubMed: 8213024]
- 9.
- Oberlander TF, Robeson P, Ward V, et al. Prenatal and breast milk morphine exposure following maternal intrathecal morphine treatment. J Hum Lact 2000;16:137-42. [PubMed: 11153344]
- 10.
- Baka NE, Bayoumeu F, Boutroy MJ, et al. Colostrum morphine concentrations during postcesarean intravenous patient-controlled analgesia. Anesth Analg 2002;94:184-7. [PubMed: 11772825]
- 11.
- Guo Q, Zheng KY, Chen FY, et al. Study on pharmacokinetics of morphine in the latex of lying-in women after PCA. Chin Pharm J (China) 2008;43:127-8.
- 12.
- Naumburg EG, Meny RG, Findlay J, et al. Codeine and morphine levels in breast milk and neonatal plasma. Pediatr Res 1987;21 (4, Pt 2):240A. doi:10.1203/00006450-198704010-00437 [CrossRef]
- 13.
- Wittels B, Glosten B, Faure EA, et al. Postcesarean analgesia with both epidural morphine and intravenous patient-controlled analgesia: Neurobehavioral outcomes among nursing neonates. Anesth Analg 1997;85:600-6. [PubMed: 9296416]
- 14.
- Metz VE, Comer SD, Pribasnig A, et al. Observational study in an outpatient clinic specializing in treating opioid-dependent pregnant women: Neonatal abstinence syndrome in infants exposed to methadone-, buprenorphine- and slow-release oral morphine. Heroin Addict Relat Clin Probl 2015;17:5-15. https://www
.heroinaddictionrelatedclinicalproblems .org/harcp-archives .php?year=2015 - 15.
- Beauchamp GA, Hendrickson RG, Horowitz BZ, et al. Exposures through breast milk: An analysis of exposure and information calls to U.S. poison centers, 2001-2017. Breastfeed Med 2019;14:508-12. [PubMed: 31211594]
- 16.
- Patricelli CJ, Gouin IJ, Gordon S, et al. Breastfeeding on injectable opioid agonist therapy: A case report. J Addict Med 2022;7:222-6. [PMC free article: PMC10022656] [PubMed: 36001061]
- 17.
- Zipursky JS, Gomes T, Everett K, et al. Maternal opioid treatment after delivery and risk of adverse infant outcomes: Population based cohort study. Bmj 2023;380:e074005. [PMC free article: PMC10015218] [PubMed: 36921977]
- 18.
- Tolis G, Dent R, Guyda H. Opiates, prolactin, and the dopamine receptor. J Clin Endocrinol Metab 1978;47:200-3. [PubMed: 263291]
- 19.
- Lind JN, Perrine CG, Li R. Relationship between use of labor pain medications and delayed onset of lactation. J Hum Lact 2014;30:167-73. [PMC free article: PMC4684175] [PubMed: 24451212]
- 20.
- Yousefshahi F, Davari-Tanha F, Najafi A, et al. Effects of intrathecal opioids use in cesarean section on breastfeeding and newborns' weight gaining. J Family Reprod Health 2016;10:176-83. [PMC free article: PMC5440816] [PubMed: 28546816]
- 21.
- Mahomed K, Wild K, Brown C, et al. Does fentanyl epidural analgesia affect breastfeeding: A prospective cohort study. Aust N Z J Obstet Gynaecol 2019;59:819-24. [PubMed: 30957895]
- 22.
- Fan HSL, Wong JYH, Fong DYT, et al. Association between intrapartum factors and the time to breastfeeding initiation. Breastfeed Med 2020;15:394-400. [PubMed: 32283038]
- 23.
- Katz D, Hyers B, Siddiqui S, et al. Impact of neuraxial preservative-free morphine in vaginal delivery on opiate consumption and recovery: A randomized control trial. Anesth Analg 2024. [PubMed: 39028662]
Substance Identification
Substance Name
Morphine
CAS Registry Number
57-27-2
Drug Class
Breast Feeding
Lactation
Milk, Human
Analgesics, Opioid
Narcotics
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Dihydrocodeine.[Drugs and Lactation Database (...]Review Dihydrocodeine.. Drugs and Lactation Database (LactMed®). 2006
- Review Nalbuphine.[Drugs and Lactation Database (...]Review Nalbuphine.. Drugs and Lactation Database (LactMed®). 2006
- Review Remifentanil.[Drugs and Lactation Database (...]Review Remifentanil.. Drugs and Lactation Database (LactMed®). 2006
- Review Fentanyl.[Drugs and Lactation Database (...]Review Fentanyl.. Drugs and Lactation Database (LactMed®). 2006
- Review Piritramide.[Drugs and Lactation Database (...]Review Piritramide.. Drugs and Lactation Database (LactMed®). 2006
- Morphine - Drugs and Lactation Database (LactMed®)Morphine - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
