Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 111974-69-7
Drug Levels and Effects
Summary of Use during Lactation
Maternal quetiapine doses of up to 400 mg daily produce doses in milk that are less than 1% of the maternal weight-adjusted dosage. Limited long-term follow-up of infants exposed to quetiapine indicates that infants generally developed normally. A safety scoring system finds quetiapine to be possible to use during breastfeeding.[1] Systematic reviews of second-generation antipsychotics concluded that quetiapine seemed to be the first- or second-choice agent during breastfeeding.[2-4] Monitor the infant for drowsiness and developmental milestones, especially if other antipsychotics are used concurrently. Cases of galactorrhea and milk ejection have been reported rarely.
Drug Levels
Maternal Levels. One mother took oral quetiapine 200 mg daily throughout pregnancy and postpartum. At 3 weeks postpartum, milk samples were taken. The average milk level over the 6-hour dosage interval was 13 mcg/L. A peak milk quetiapine level of 62 mcg/L occurred at 1 hour after the dose. The authors estimated that an exclusively breastfed infant would receive 0.09% of the weight-adjusted maternal dosage on average, with a "worst-case" dosage (assuming all nursing was at the peak concentration) of 0.43% of weight-adjusted maternal dosage.[5]
Six nursing mothers who were 6.5 to 18.5 weeks postpartum were taking quetiapine in doses of 25 to 400 mg daily in addition to an antidepressant for major depression postpartum. Milk samples obtained at various times after the dose had undetectable (<11.5 mcg/L) levels of quetiapine in the 4 mothers taking 75 mg daily or less. A mother taking 100 mg daily had a milk quetiapine level of 12.3 mcg/L and another taking 400 mg daily had a level of 101 mcg/L. The authors estimated that exclusively breastfed infants would receive less than 0.01 mg/kg daily with maternal doses of 100 mg daily or less and less than 0.1 mg/kg daily with a maternal dose of 400 mg daily.[6]
A woman who was 3 months postpartum and taking quetiapine 400 mg daily, fluoxetine 40 mg daily, and oxycodone 20 mg 3 times daily had 16 milk samples taken over 24 hours starting immediately before a daily dose of quetiapine; 12 were paired fore- and hindmilk and the other 4 samples were mixtures of fore- and hindmilk. The highest quetiapine level measured in milk of about 170 mcg/L occurred within 1 hour after the dose. Milk levels dropped to nearly zero by 12 hours after the dose. No differences were noted between fore- and hindmilk concentrations. The authors estimated that the infant received 6.2 mcg/kg daily and that a fully breastfed infant would receive 0.09% of the maternal weight-adjusted dosage.[7]
A nursing mother was taking quetiapine in a dosage of 200 mg daily. Quetiapine was undetectable (<5 mcg/L) in her breastmilk.[8]
In a study of 9 women taking quetiapine in an average dose of 37 mg daily (range 6.25 - 100 mg daily), simulations of infant exposure indicated that the infant would receive <0.5% of the maternal weight-adjusted dosage.[9] Further population analysis of the data was performed using NONMEM. Using the data obtained, 1000 computer simulations of breastmilk concentrations and infant dosages were performed. Results showed that 99% of breastfed infants would ingest quetiapine in dosages below 0.42% of the maternal weight-adjusted dose.[10]
One woman was taking quetiapine 200 mg daily at 11 pm. She avoided breastfeeding from 11 pm to 7 am each day. Breastmilk samples were collected at 4 am, 8 am and 11 pm daily for 26 days. The average quetiapine concentrations in her breastmilk were 11.7 mcg/L, at 4 am, 5.4 mcg/L at 8 am, and 0.9 mcg/L at 11 pm. The authors estimated that her infant would receive a maximum of 0.37 mg/kg daily and a median dosage of 0.1 mg/kg daily, which would translate to 0.017% and 0.005% of the weight-adjusted maternal dosage, respectively.[11]
A woman with bipolar disorder who delivered twins and was taking sodium valproate was started on quetiapine 200 mg and olanzapine 15 mg at 11 pm daily after 20 days postpartum. She withheld breastfeeding during the night and discarded milk pumped at 7 am. She then breastfed her infants until 11 pm. After 7 days of therapy, milk samples were obtained at 4 am, 8 am and 11 pm for 27 of the next 45 days. The median average daily quetiapine milk concentration was 3.7 mcg/L. Median milk concentrations were 10.7 mcg/L at 4 am, 3.7 mg/L at 8 am and 0.9 mg/L at 11 pm. The authors calculated that if the infants had been fully breastfed, they would have received a daily dosage of 0.38 mcg/kg or 0.02% of the maternal weight-adjusted dosage. By withholding nursing during the night, the infants' quetiapine dosage was reduced by 55% compared to the dose they would have received if they had been breastfed around the clock.[12]
Nine breastfeeding mothers who were taking rapid-release quetiapine in an average dose of 41 mg daily provided milk samples at approximately 0, 1, 2, 4, 7, 12, and 24 hours after a dose. The peak milk concentration of quetiapine occurred at 2 hours after the dose and declined with a half-life of 7.4 hours. The average milk concentration was 5.7 mcg/L (range 1.4 to 13.9 mcg/L). The authors estimated the mean infant quetiapine dose was 0.16% of the maternal weight-adjusted dosage.[13]
A woman was taking oral extended-release quetiapine 300 mg daily during the last 3 months of pregnancy and postpartum. She breastfed her infant and provided a milk sample on two occasions. At one month postpartum, her serum quetiapine level at 17 hours after a dose was subtherapeutic and quetiapine was not detectable in milk. The low levels were thought to be a result of poor compliance with the dosage regimen. At 3 months postpartum, the serum level was in the therapeutic range at 11 hours after a dose and a milk level at the same time was 30 mcg/L, corresponding to a relative infant dosage of 0.09%.[14]
A woman with schizophrenia received brexpiprazole 2 mg once daily, risperidone 2 mg twice daily and quetiapine 12.5 mg twice daily during pregnancy and postpartum. The concentration of quetiapine in milk was below 0.27 mcg/L on day 4 approximately 2 hours after the last dose, on day 5 at 6.5 hours after the last dose, and on day 6 at 22 hours after the last dose.[15]
Infant Levels. A 3-month-old infant who was breastfed 6 to 7 times daily during maternal use of 400 mg daily of quetiapine had a plasma quetiapine level of 1.4 mcg/L. This level was 6% of the mother's quetiapine plasma level at the same time.[7]
In a study of 9 women taking quetiapine in an average dose of 37 mg daily (range 6.25 - 100 mg daily), simulations of infant exposure indicated that the infant would be expected to attain serum concentrations <0.6% of the maternal serum quetiapine concentration.[9]
A woman was taking quetiapine 100 mg each night for treatment of bipolar disorder during 2 pregnancies. and during breastfeeding. She breastfed both preterm infants and on 2 days, milk was pumped 1 hour after the dose, at the presumed time of the peak milk quetiapine level and given to the infant. Infant serum levels were measured one hour after the breastmilk intake on 2 separate occasions. In one infant, serum quetiapine levels were <1 and 3 mcg/L on days 6 and 33 of age, respectively. In the second infant, serum quetiapine levels were 0 (<0.096 mcg/L) and 15 mcg/L on days 4 and 6 of age, respectively.[16]
A breastfed newborn infant whose mother was taking brexpiprazole 2 mg once daily, risperidone 2 mg twice daily and quetiapine 12.5 mg twice daily during pregnancy and postpartum had serum levels measured. At birth, the cord blood level was 0.36 mcg/L from maternal use during pregnancy. The neonate ingested small volumes of colostrum and milk 12 times from 46 to 86.5 hours after birth. By 16.5 hours postpartum, the infant’s serum quetiapine concentration was undetectable (< 0.25 mcg/L) and it remain undetectable up to 137 hours postpartum when sampling was discontinued.[15]
Effects in Breastfed Infants
One mother took quetiapine 25 mg daily orally during pregnancy and continued to take quetiapine 50 mg daily orally during lactation. At 6 weeks the infant was doing well. No further follow-up was reported.[17]
Another infant whose mother was taking 200 mg daily of quetiapine began to exclusively breastfeed at 8 weeks of age. The infant was developing well at 4.5 months of age and no adverse effects were reported.[5]
A nursing mother with postpartum psychosis was started on quetiapine at 6 weeks postpartum at a dose of 25 mg daily along with unspecified benzodiazepines. The quetiapine dosage was increased gradually to 200 mg daily over the next 6 weeks and up to 300 mg daily over the ensuing 4 weeks (16 weeks postpartum). Mirtazapine 15 mg daily was also started at 8 weeks postpartum. Breastfeeding (extent not specified) was continued until 16 weeks postpartum when it was stopped because of reduced milk production. During this time, the infant was excessively drowsy until the benzodiazepine dosage was decreased at the same time as the quetiapine dosage was increased. The infant was followed for at least 2 months after breastfeeding ended and no effects on the infant's growth, motor or psychological development or signs of infant withdrawal were noted.[18]
A nursing mother with bipolar disorder began taking 20 mg of paroxetine at 4 months postpartum and was then started on quetiapine 200 mg twice daily at 6 months postpartum. She breastfed regularly (extent not stated) and no obvious adverse effects were noted in the infant.[19]
A woman who was treated chronically with quetiapine 400 mg and fluvoxamine 200 mg daily took the drugs throughout pregnancy and postpartum. She partially breastfed her infant (extent not stated) for 3 months from birth. No adverse events were seen and the infant developed normally.[20]
Six nursing mothers took quetiapine in doses of 25 to 400 mg daily in addition to an antidepressant (usually paroxetine) for major depression postpartum. Their breastfed infants' development were tested at 9 to 18 months of age with the Bayley scales. Measurements were slightly low on the mental and psychomotor development scale in one infant and on the mental development scale in another. All other scores were within normal limits. The authors concluded that the low scores of the 2 infants were probably not caused by the drugs received by the infants in breastmilk.[6]
An infant was born to a mother taking quetiapine 400 mg daily, fluoxetine 40 mg daily and oxycodone 20 mg 3 times daily. The infant was breastfed 6 to 7 times daily and was receiving 120 mcg of oral morphine 3 times daily for opiate withdrawal. Upon examination at 3 months of age, the infant's weight was at the 25th percentile for age, having been at the 50th percentile at birth. The authors attributed the weight loss to opiate withdrawal. The infant's Denver developmental score was equal to his chronological age.[7]
One 60-week-old infant who was 50% breastfed was breastfed during maternal therapy with quetiapine 75 mg daily mg daily and venlafaxine 225 mg daily. No adverse reactions were reported by the mother or in the medical records.[21]
A woman with bipolar disorder who delivered twins and was taking sodium valproate in a therapeutic dosage was started on quetiapine 200 mg and olanzapine 15 mg at 11 pm daily after 20 days postpartum. She withheld breastfeeding during the night and discarded milk pumped at 7 am. She then breastfed her infants until 11 pm. The mother continued feeding the infants on this schedule for 15 months. Monthly follow-up of the infants indicated normal growth and neither the pediatricians nor the parents noted any adverse effects in the infants.[12]
A mother taking quetiapine 100 mg each night for bipolar disorder breastfed 2 successive preterm infants. Both infants were reported to be developing normally at their last follow-up visits (exact times not specified).[16]
A woman with bipolar disorder took quetiapine 25 mg and lamotrigine 100 mg daily for the treatment of bipolar disorder during two pregnancies. After the first birth, she did not breastfeed, but she breastfed (extent not stated) the second infant. At the 2-month well baby checkup, the infant was meeting all developmental milestones.[22]
A woman received a combination of 300 mg lamotrigine and 300 of quetiapine daily for postpartum bipolar II postpartum depression. The authors reported no major adverse reactions in her breastfed (extent not stated) infant.[23]
An author reported 1 infant who was breastfed (extent not stated) during postpartum maternal treatment for bipolar disorder. Her quetiapine dosage was 200 mg daily. The mother reported no adverse effects in the infants.[24]
A prospective cohort study of infants breastfed by mothers in an inpatient mother-baby psychiatric unit in India followed 2 infants who were exposed to quetiapine in breastmilk; most received partial supplementation. Neither had any short-term adverse effects. Infants were followed for 1 to 3 months after discharge and one of the infants who was also exposed to quetiapine in utero had motor and mental delay.[25]
A woman was taking oral extended-release quetiapine 300 mg daily during the last 3 months of pregnancy and postpartum. At 3 months postpartum, her breastfed (extent not stated) infant had no apparent adverse effects and was developing normally.[14]
Patients enlisted in the National Pregnancy Registry for Atypical Antipsychotics who were taking a second-generation antipsychotic drug while breastfeeding (n = 576) were compared to control breastfeeding patients who were not treated with a second-generation antipsychotic (n = 818). Of the patients who were taking a second-generation antipsychotic drug, 60.4% were on more than one psychotropic. A review of the pediatric medical records, no adverse effects were noted among infants exposed or not exposed to second-generation antipsychotic monotherapy or to polytherapy.[26] The number of women taking quetiapine was not reported.
Effects on Lactation and Breastmilk
Unlike the phenothiazines, quetiapine has a minimal effect on serum prolactin levels.[27-29] However, galactorrhea has been reported.[30] The maternal prolactin level in a mother with established lactation may not affect her ability to breastfeed.
Galactorrhea occurred in a woman who was not breastfeeding while she was taking venlafaxine 112.5 mg daily and quetiapine. Galactorrhea occurred 10 days after her quetiapine dose was increased to 50 mg daily a few days after starting the drug at 12.5 mg daily. Her serum prolactin level was 27.3 mcg/L (normal 2 to 30 mcg/L) and decreased to 8.5 mcg/L 2 weeks after discontinuing the drug. Galactorrhea ceased 1 week later.[31]
Patients enlisted in the National Pregnancy Registry for Atypical Antipsychotics who were taking a second-generation antipsychotic drug while breastfeeding (n = 576) were compared to control breastfeeding patients who had primarily diagnoses of major depressive disorder and anxiety disorders, most often treated with SSRI or SNRI antidepressants, but not with a second-generation antipsychotic (n = 818). Among women on a second-generation antipsychotic, 60.4% were on more than one psychotropic compared with 24.4% among women in the control group. Of the women on a second-generation antipsychotic, 59.3% reported “ever breastfeeding” compared to 88.2% of women in the control group. At 3 months postpartum, 23% of women on a second-generation antipsychotic were exclusively breastfeeding compared to 47% of women in the control group.[26] The number of women taking quetiapine was not reported.
A woman began using quetiapine 4 weeks postpartum for intrusive thoughts. She took her daily dose of 50 mg at 11 pm after the last nursing of the day. Every night she experienced a tingling sensation and milk ejection about 30 to 40 minutes after the dose over a period of 6 months. On one occasion she did not take the dose and the milk ejection did not occur. When she resumed the drug the next night, the milk ejection resumed.[32] Milk ejection was probably caused by quetiapine.
Alternate Drugs to Consider
(Antipsychotic) Haloperidol, Olanzapine, Risperidone; (Bipolar Disorder) Divalproex, Lithium, Olanzapine, Risperidone, Valproic Acid
References
- 1.
- Uguz F. A new safety scoring system for the use of psychotropic drugs during lactation. Am J Ther 2021;28:e118-e26. [PubMed: 30601177]
- 2.
- Larsen ER, Damkier P, Pedersen LH, et al. Use of psychotropic drugs during pregnancy and breast-feeding. Acta Psychiatr Scand Suppl 2015;445:1-28. [PubMed: 26344706]
- 3.
- Uguz F. Second-generation antipsychotics during the lactation period: A comparative systematic review on infant safety. J Clin Psychopharmacol 2016;36:244-52. [PubMed: 27028982]
- 4.
- Pacchiarotti I, Leon-Caballero J, Murru A, et al. Mood stabilizers and antipsychotics during breastfeeding: Focus on bipolar disorder. Eur Neuropsychopharmacol 2016;26:1562-78. [PubMed: 27568278]
- 5.
- Lee A, Giesbrecht E, Dunn E, et al. Excretion of quetiapine in breast milk. Am J Psychiatry 2004;161:1715-6. [PubMed: 15337669]
- 6.
- Misri S, Corral M, Wardrop AA, et al. Quetiapine augmentation in lactation: A series of case reports. J Clin Psychopharmacol 2006;26:508-11. [PubMed: 16974194]
- 7.
- Rampono J, Kristensen JH, Ilett KF, et al. Quetiapine and breast feeding. Ann Pharmacother 2007;41:711-4. [PubMed: 17374621]
- 8.
- Kruninger U, Meltzer V, Hiemke C, et al. Pregnancy and lactation under treatment with quetiapin. Psychiatr Prax 2007;34 (Suppl 1):S75-6. doi:10.1055/s-2006-940185 [CrossRef]
- 9.
- Yazdani-Brojeni P, Taguchi N, García-Bournissen F, et al. Quetiapine in human milk and simulation-based assessment of infant exposure. Clin Pharmacol Ther 2010;87 (Suppl. 1):S3-4. doi:10.1038/clpt.2009.268 [CrossRef]
- 10.
- Tanoshima R, Yazdani-Brojeni P, Taguchi N, et al. Quetiapine in human breast milk - population PK analysis of milk levels and simulated infant exposure. J Popul Ther Clin Pharmacol 2012;19:e267-8.
- 11.
- Var L, Ince I, Topuzoglu A, et al. Management of postpartum manic episode without cessation of breastfeeding: A longitudinal follow up of drug excretion into breast milk. Eur Neuropsychopharmacol 2013;23 (Suppl 2):S382. https://www
.sciencedirect .com/journal/european-neuropsychopharmacology /vol/23/suppl/S2 - 12.
- Aydin B, Nayir T, Sahin S, et al. Olanzapine and quetiapine use during breastfeeding: Excretion into breast milk and safe breastfeeding strategy. J Clin Psychopharmacol 2015;35:206-8. [PubMed: 25679127]
- 13.
- Yazdani-Brojeni P, Tanoshima R, Taguchi N, et al. Quetiapine excretion into human breast milk. J Clin Psychopharmacol 2018;38:362-4. [PubMed: 29912789]
- 14.
- Pastol J, Le Marois M, Guilhaumou R, et al. Measuring drug concentrations in breast milk to improve therapeutic monitoring and patient adherence in bipolar disorder: A case report. Aust N Z J Psychiatry 2022;56:96. [PubMed: 33938286]
- 15.
- Konishi T, Kitahiro Y, Fujiwara N, et al. Pharmacokinetics of brexpiprazole, quetiapine, risperidone, and its active metabolite paliperidone in a postpartum woman and her baby. Ther Drug Monit 2024;46:687-91. [PubMed: 38648649]
- 16.
- Van Boekholt AA, Hartong EG, Huntjens-Fleuren H, et al. Quetiapine concentrations during exclusive breastfeeding and maternal quetiapine use. Ann Pharmacother 2015;49:743-4. [PubMed: 25975996]
- 17.
- Balke LD. Quetiapine effective in the treatment of bipolar affective disorder during pregnancy. World J Biol Psychiatry 2001;2:303S.
- 18.
- Seppala J. Quetiapine ('Seroquel') is effective and well tolerated in the treatment of psychotic depression during breast-feeding. Int J Neuropsychopharmacol 2004;7 (Suppl 2):S245. doi:10.1017/S1461145704004547 [CrossRef]
- 19.
- Ritz S. Quetiapine monotherapy in post-partum onset bipolar disorder with a mixed affective state. Eur Neuropsychopharmacol 2005;15 (Suppl 3):S407. doi:10.1016/S0924-977X(05)80825-9 [CrossRef]
- 20.
- Gentile S. Quetiapine-fluvoxamine combination during pregnancy and while breastfeeding. Arch Womens Ment Health 2006;9:158-9. [PubMed: 16683078]
- 21.
- Newport DJ, Ritchie JC, Knight BT, et al. Venlafaxine in human breast milk and nursing infant plasma: Determination of exposure. J Clin Psychiatry 2009;70:1304-10. [PubMed: 19607765]
- 22.
- Lévesque S, Riley C. Fetal exposure to lamotrigine and quetiapine in two consecutive pregnancies. Arch Womens Ment Health 2017;20:237-9. [PubMed: 27785634]
- 23.
- Sharma V, Sommerdyk C. Lamotrigine in the prevention of bipolar II postpartum depression. Prim Care Companion CNS Disord 2016;18. [PubMed: 27907274]
- 24.
- Uguz F. Prophylactic use of olanzapine and quetiapine from pregnancy to the postpartum period in women with bipolar disorder: A case series. J Matern Fetal Neonatal Med 2017;30:2569-71. [PubMed: 27809629]
- 25.
- Sinha SK, Thomas Kishore M, Thippeswamy H, et al. Adverse effects and short-term developmental outcomes of infants exposed to atypical antipsychotics during breastfeeding. Indian J Psychiatry 2021;63:52-7. [PMC free article: PMC8106424] [PubMed: 34083820]
- 26.
- Viguera AC, Vanderkruik R, Gaccione P, et al. Breastfeeding practices among women taking second-generation antipsychotics: findings from the National Pregnancy Registry for Atypical Antipsychotics. Arch Womens Ment Health 2022;25:511-6. [PubMed: 34318375]
- 27.
- Atmaca M, Kuloglu M, Tezcan E, et al. Quetiapine is not associated with increase in prolactin secretion in contrast to haloperidol. Arch Med Res 2002;33:562-5. [PubMed: 12505103]
- 28.
- Maguire GA. Prolactin elevation with antipsychotic medications: Mechanisms of action and clinical consequences. J Clin Psychiatry 2002;63 (Suppl 4):56-62. [PubMed: 11913677]
- 29.
- Arvanitis LA, Miller BG. Multiple fixed doses of "Seroquel" (quetiapine) in patients with acute exacerbation of schizophrenia: A comparison with haloperidol and placebo. The seroquel trial 13 study group. Biol Psychiatry 1997;42:233-46. [PubMed: 9270900]
- 30.
- Glocker C, Grohmann R, Engel R, et al. Galactorrhea during antipsychotic treatment: Results from AMSP, a drug surveillance program, between 1993 and 2015. Eur Arch Psychiatry Clin Neurosci 2021;271:1425-35. [PMC free article: PMC8563638] [PubMed: 33768297]
- 31.
- Pae CU, Kim JJ, Lee CU, et al. Very low dose quetiapine-induced galactorrhea in combination with venlafaxine. Hum Psychopharmacol 2004;19:433-4. [PubMed: 15303249]
- 32.
- Passier A, Lamers M, van den Berg K, et al. Quetiapine intake and milk ejection reflex in a breastfeeding woman: A case report. Neurotoxicol Teratol 2023;98:25. doi:10.1016/j.ntt.2023.107238 [CrossRef]
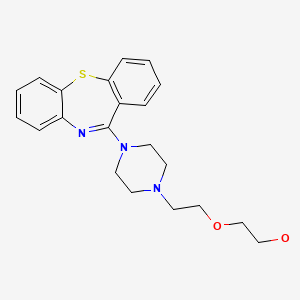
Substance Identification
Substance Name
Quetiapine
CAS Registry Number
111974-69-7
Drug Class
Breast Feeding
Lactation
Milk, Human
Antipsychotic Agents
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Olanzapine.[Drugs and Lactation Database (...]Review Olanzapine.. Drugs and Lactation Database (LactMed®). 2006
- Review Risperidone.[Drugs and Lactation Database (...]Review Risperidone.. Drugs and Lactation Database (LactMed®). 2006
- Review Chlorpromazine.[Drugs and Lactation Database (...]Review Chlorpromazine.. Drugs and Lactation Database (LactMed®). 2006
- Review Escitalopram.[Drugs and Lactation Database (...]Review Escitalopram.. Drugs and Lactation Database (LactMed®). 2006
- Review Perphenazine.[Drugs and Lactation Database (...]Review Perphenazine.. Drugs and Lactation Database (LactMed®). 2006
- Quetiapine - Drugs and Lactation Database (LactMed®)Quetiapine - Drugs and Lactation Database (LactMed®)
- eggc.vipGWI (0)BioProject
- eggc.vipBq4 (0)BioProject
- eggc.vipJLv (0)BioProject
- Borreliella burgdorferi B31Borreliella burgdorferi B31Causes Lyme diseaseBioProject
Your browsing activity is empty.
Activity recording is turned off.
See more...
